Playlist
Show Playlist
Hide Playlist
Intestine Obstruction: Diagnosis & Management
-
Slides SmallBowelObstruction Surgery.pdf
-
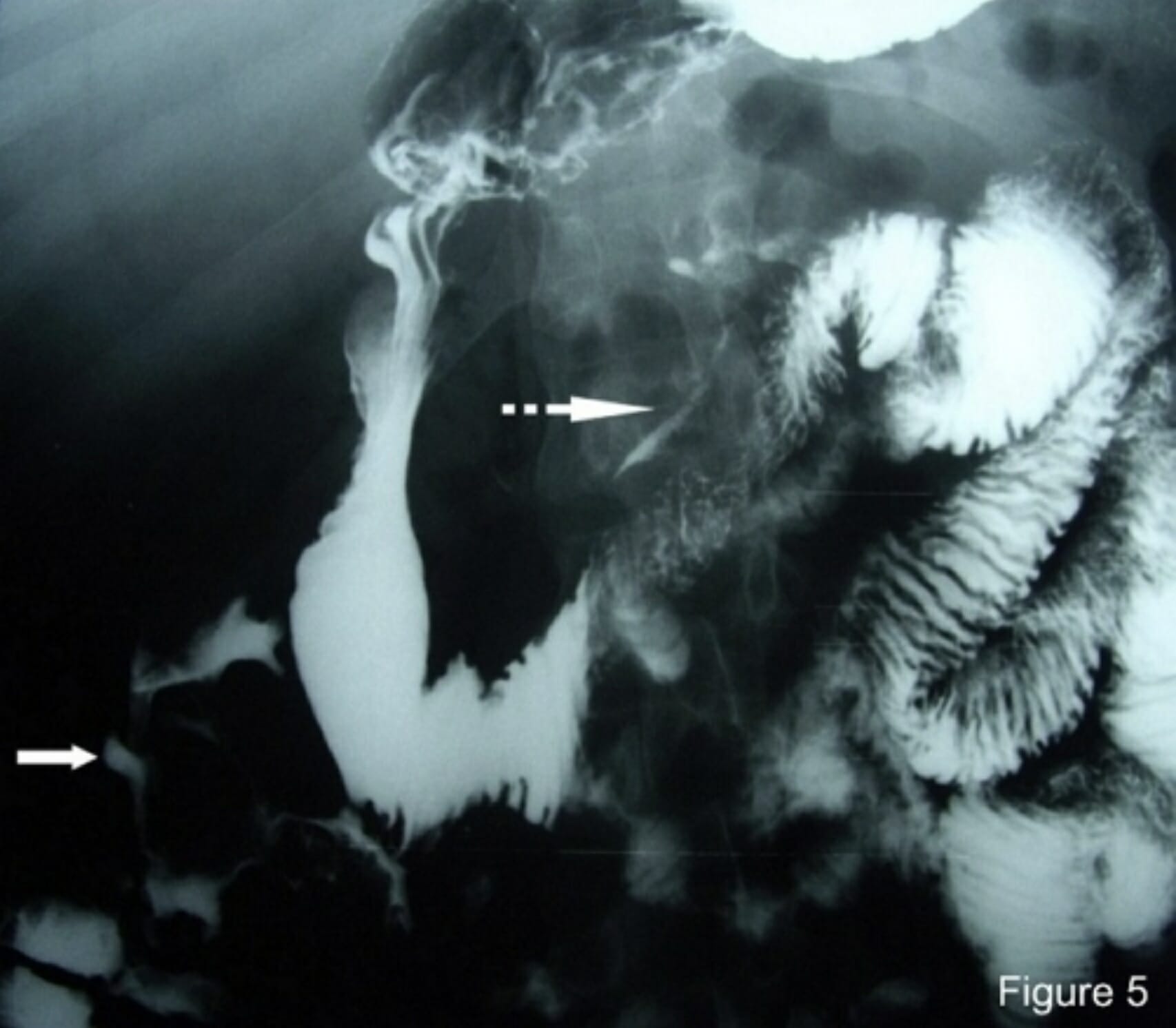
Download Lecture Overview
00:01 One of the ways that one can tell the difference between small intestines and large intestines on an abdominal X-ray is its central location. Additionally, you’ll notice that there’s a lot of distended small bowel in this abdominal X-ray. Frequently, we will also look for air fluid levels. Here’s cross-sectional imaging. The arrow points to an area where we call the transition point. The transition point goes from proximal dilated bowel to distal decompressed bowel. You can think of it as stepping on a garden hose which obstructs the flow of water. Lactate, it’s important to get a lactate particularly in patients who have suspicions of ischemic bowel. A lactate level that is elevated suggests the patient is undergoing anaerobic metabolism. Anaerobic metabolism combined with peritoneal signs or with signs of ischemic bowel is an absolute indication for an exploratory laparotomy. Remember that if this scenario is presented to you. Just a brief reminder of the lactate, Cori cycle. End product of glycolysis during anaerobic metabolism is lactate. Lactate in and of itself is not necessarily harmful. It’s but a mark of anaerobic metabolism. Recall to the Cori cycle that the lactate can be circulated and used for gluconeogenesis. 01:22 However, persistence of lactate may indicate ischemic bowel. What if the lactate is elevated? I’ll give you a moment to think about this. Sure, if the lactate is elevated, it suggests again anaerobic metabolism. There’s not enough oxygen getting delivered to the small intestines or to any organ system for that matter. This is a potential intestinal compromise which may necessitate urgent surgery. Another question for you. What is the difference between a complete and incomplete SBO or partial small bowel obstruction? I’ll give you a moment to think about this. 02:05 A complete bowel obstruction suggests the complete absence of flatus and bowel movement and may more likely lead to ischemic bowel. The classic, classic description of a complete bowel obstruction is either a bowel twisting on itself or that there are two points of obstruction both proximal and distally. 02:24 A special type is called a closed loop bowel obstruction where two points are obstructed. 02:30 This can be the terminal ileum and the ileocecal valve both serving as a point of obstruction. 02:37 The segment of intestines between the terminal ileum and the ileocecal valve can then be easily compromised in terms of its blood supply. Here’s a garden hose illustration of a closed loop bowel obstruction. You’ll notice from this image that the bowel has twisted on itself and you’ll notice that proximally and distally, the intestines cannot move the effluent past this area of twisting. 03:03 What decision processes are involved in the management of small bowel obstructions? Here's my schematic of how to manage small bowel obstructions. I like to think of small bowel obstructions as complete or partial. The difference is how urgent the surgery is. With a complete obstruction, there’s zero chance that that patient will resolve without surgery. Furthermore, without surgery, the intestines may be compromised. Therefore, for complete bowel obstructions, surgery is warranted mostly on an urgent or emergent base. The vast majority though of patients that come in for small bowel obstructions are incomplete or partial in nature. In these patients, we want to look at whether or not they have any signs of bowel ischemia or peritoneal signs. 03:49 Recall, anybody who had peritoneal signs, increased lactate, potentially leukocytosis may need surgery. The vast majority of patients do not present with peritoneal signs and are candidates for a trial of nonoperative management. That’s standard. You know, it used to be that we would never let the sun set on a bowel obstruction. However, with cross-sectional imaging, modern medicine, very few of our patients actually require surgery within 24 hours. Well, what is a trial of nonoperative management? That’s a classic NG tube, NPO status, rehydration via an intravenous fluid. 04:31 Non-surgical management, we discussed already: NG tube, nothing by mouth status, ambulation. 04:38 It sounds so simple and the patients frequently ask me, “What can I do to make this bowel obstruction go away?” I say, “Unfortunately, nothing. But continue to ambulate.” Ambulation is both great for postoperative ileus which is not a mechanical obstruction as well as bowel obstructions. 04:53 As much as we can, minimize narcotic medications. Unfortunately, a small percentage of patients will require surgery. Again, to remind you the indications for surgery: perforation, signs of ischemia, worsening peritonitis, and frankly, failure of nonoperative management. 05:14 This picture that you’re seeing is an intraoperative finding of a segment. You clearly see the difference between the purple bowel which is an ischemic segment versus the normal-appearing bowel next to it. This ischemic segment needs to be resected. Whether or not a primary anastomosis or reconnection of the small intestines is feasible depends on the patient’s clinical status as well as the integrity of the intestines both proximal and distal to the segment of resection. 05:45 Very important clinical pearls to remember: Patients who have never had abdominal surgery are unlikely to have adhesive disease. Therefore, those patients may need a lower threshold to go to the operating room. What do I mean by that? For example, if you’ve never had abdominal surgery, there’s no reason for you to have adhesive disease unless you have had subclinical diverticulitis. In these patients then, all of a sudden, tumor or cancer is higher on the differential diagnosis list. 06:16 High-yield information for your examination: Incarcerated hernias particularly inguinal hernias should be on your differential diagnosis for small bowel obstruction. Post-surgery adhesive disease is one of the most common etiologies. Remember, not all of these patients require surgery. 06:34 Most will resolve with a trial of nonoperative management. So, don’t be in a hurry to rush the patient off to the operating room when presented with this clinical scenario. Thank you very much for joining me on this discussion of small bowel obstructions.
About the Lecture
The lecture Intestine Obstruction: Diagnosis & Management by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following is NOT true about elevated lactic acid concentration in the blood in the setting of intestinal obstruction?
- It is a marker of increased aerobic metabolism.
- It can be caused by increased anaerobic metabolism.
- Combined with the overall clinical picture, it can impact the management.
- It could be a sign of intestinal ischemia.
- Combined with the presence of peritoneal signs, it could be an indication for exploratory laparotomy.
Which of the following results in a complete bowel obstruction?
- Closed loop obstruction
- Tumor
- A single point obstruction
- Surgical adhesions
- A hernia
All of the following are indications for immediate surgery in patients with bowel obstruction except?
- Incomplete obstruction
- Peritoneal signs
- Leukocytosis
- Elevated lactate levels
- Evidence of bowel ischemia
Which of the following is not included in the non-operative management of bowel obstruction?
- Pain management with narcotics
- Dietary restriction to NPO (nothing by mouth)
- Naso-gastric tube insertion
- Intravenous fluid hydration
- Encourage ambulation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Eu gostei do jeito que as informações foram apresentadas, a aula foi clara, simples e direta. Não deixando nada faltar. A parte que envolve diagnostico e manejo esta especialmente boa. Obrigada