Playlist
Show Playlist
Hide Playlist
Inflammatory Myopathies, Polymyositis & Dermatomyositis
-
Rheumatology I 04 Non Arthritic Connective Tissue Diseases.pdf
-
Reference List Pathology.pdf
-
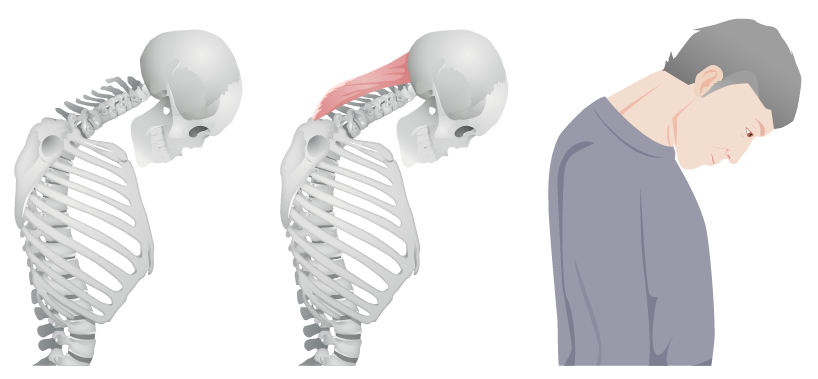
Download Lecture Overview
00:01 Here we have our inflammatory myopathies. 00:03 The two that we’ll discuss are polymyositis and dermatomyositis. 00:09 Let’s put this into perspective. 00:11 With polymyositis, you’re gonna be thinking about your proximal muscles which then spreads out in a symmetrical fashion causing fatigue and tiredness, and inflammation, obviously. 00:27 And what you’ll find here is that there will be involvement of your CD8 cells in polymyositis and involvement of the endomysium. 00:36 Whenever you hear the term dermatomyositis, your focus here is going to be on derm skin issues. 00:46 For example, you’ve heard of heliotrope rash around the eyes, periorbital. 00:51 You’ve heard of Gottron lesion that you might find on your knuckles, and you’ve heard of something like your shawl and face type of rash, maybe even malar. 01:00 That’s dermato, I’m going to talk about this in a second. 01:03 So these are autoimmune diseases of the muscle characterized by a proximal muscle weakness, that will be more so poly, elevated muscle enzymes such as kinases, inflammatory infiltrate of muscle biopsy is what you’re going to be - or what we will be looking for. 01:20 When it’s around the eyelids, the rash, periorbital, we call it heliotropic. 01:26 Think of it as being a halo around the orbit. 01:31 On a knuckle, it’s galled Gottron and then, if it’s rash that you find on the chest like wearing a shawl and on the face, maybe a malar rash. 01:44 What does malar mean to you? The butterfly patterned type of rash. 01:47 That is going to be dermatomyositis, almost always is that understood. 01:52 Interstitial lung disease present, then you would be calling this Antisynthetase syndrome and I need to give you a particular marker that I mentioned earlier but I’ll mention here, it’s called Jo-1, okay, Jo-1, as we shall see. 02:08 The pathogenesis, molecular mimicry from viral infections is the proposed theory that you wanna know. 02:14 Many viral infections can cause this myositis. 02:17 Let’s talk about the signs and symptoms. 02:19 Well, notably, we’ll take a look at polymyositis. 02:22 I told you earlier that the weakness first begins in the proximal muscles, symmetrical. 02:27 Look for a patient that might have difficulty rising from a supine or sitting position, walking up and down the stairs, look for issues maybe in the morning as well. 02:37 So now you have three morning issues, each one, completely different. 02:41 Rheumatoid arthritis, greater than one hour at your stiffness. 02:45 Osteoarthritis, less than 30 minutes, with movement makes it worse, and then here, difficulty at walking proximal muscles and such, we have polymyositis. 02:55 Difficulty combing hair or brushing the teeth. 02:58 It could involve respiratory or dysphagia in the GI system. 03:04 We talked about these rashes in dermatomyositis. 03:08 And how they trope around the eyelid, Gottron over the metacarpal phalangeal, or your knuckles, your PIP. 03:14 A V-shaped rash that you might find around the neck is your shawl distribution. 03:19 You might have a butterfly rash that resembles SLE, Malar, be careful. 03:23 Dermatomyositis symptoms associate with underlying malignancy. 03:27 For example, visceral malignancies, make sure your patient is up-to-date with malignant screening. 03:33 That is important. 03:34 So when you find a Gottron legion, next step of management, please make sure that all malignancies have been properly ruled out or have been properly monitored. 03:43 Take a look at the picture on the left, what do you think this is? The periorbital type of rash that you see here is heliotrope. 03:52 On the right, you have a rash like formation of the knuckle and over the PIP. 03:57 And this would then represent your Gottron legion. 04:00 Diagnosis, similar levels of kinase is elevated, aldolase will be elevated, your transaminases might be elevated, as would be your LDH. 04:13 Look for CK in aldolase and that could be positive. 04:18 Remember, ultimately, many of these will share common markers. 04:22 Here’s one that’s more specific, anti-Jo-1 antibody. 04:26 It can be seen in about 20 or 30 patients in this then therefore along with interstitial lung disease, so we have dermatomyositis and we have interstitial lung disease, this is then called Antisynthetase syndrome. 04:42 A couple of times I’ve mentioned this. 04:44 Hopefully at this point, you’re quite familiar with what’s going on with Anti-Jo-1 antibody when you see this. 04:50 Other markers that are quite important, Anti-Mi-2 antibodies, can be positive to about 10% but look for that especially with dermatomyositis, Anti-Mi-2. 05:02 Anti-SRP will be specific for these inflammatory myopathies. 05:08 Image affected muscle groups with MRI, EMG with muscle biopsy confirms your diagnosis confirmation, and your differentials include thyroid disease, Cushing syndrome, steroids, statin, alcohol, HIV, neurologic, infectious. 05:30 So there’s a list on inflammatory myopathies. 05:33 However, you pay attention to the markers and such, and remember, once again, what if you find Mi-2, what does that mean? You’re thinking about dermatomyositis. 05:43 Management here includes your modulators of corticosteroids and methotrexate, refractory, then you’re thinking about rituximab which is an anti-CD20. 05:54 If resistant to therapy, consider inclusion body myositis as a possible diagnosis. 06:02 Especially if muscle biopsy has not confirmed PM or DM, or has not been done. 06:10 Once again, if it’s resistant to therapy, you wanna make sure that you’ve confirmed the proper diagnosis. 06:16 Inclusion body myositis will be your next step of proper management of your patient.
About the Lecture
The lecture Inflammatory Myopathies, Polymyositis & Dermatomyositis by Carlo Raj, MD is from the course Connective Tissue Diseases. It contains the following chapters:
- Introduction to Inflammatory Myopathies
- Symptoms of Inflammatory Myopathies
- Diagnosis of Inflammatory Myopathies
Included Quiz Questions
Relatively acute onset of myositis, inflammatory arthritis, Raynaud phenomenon, and interstitial lung disease is most suggestive of what condition?
- Antisynthetase syndrome
- Sjögren syndrome
- Psoriatic arthritis
- Systemic sclerosis
- Systemic lupus erythematosus
What is the most common antisynthetase antibody and the most common myositis-specific antibody?
- Anti-Jo-1
- Antibodies to ribonucleoprotein
- Anti-centromere
- Anti-cyclic citrullinated peptide
- Anti-double stranded DNA
Heliotrope rash on the eyelids and inflammatory (Gottron) papules on the dorsum of the hands are characteristic cutaneous findings of what condition?
- Dermatomyositis
- Systemic sclerosis
- Systemic lupus erythematosus
- Rheumatoid arthritis
- Polymyositis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |