Playlist
Show Playlist
Hide Playlist
Hepatitis B
-
Slides GD liver disease.pdf
-
Download Lecture Overview
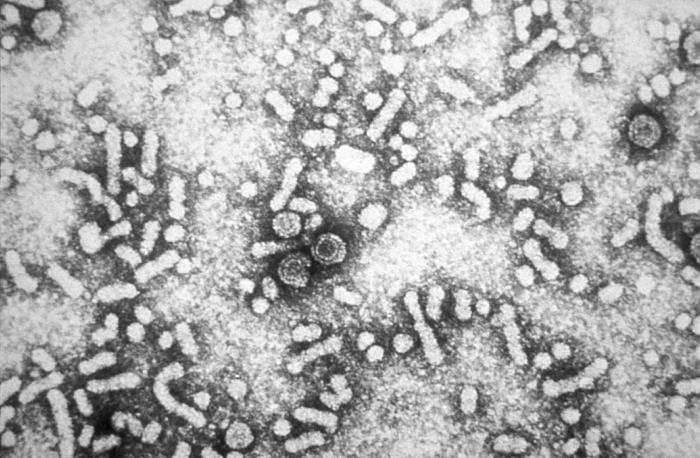
00:01 Quickly here, hepatitis B. 00:03 Now, we’re getting to more chronic users. 00:05 And hepatitis B, obviously, there is going to be vaccination involved. 00:09 And in immunology and microbiology, you’ve covered these topics further. 00:13 What I'm going to provide to you is more of a clinical background for each one of these viral hepatites. 00:20 400 million worldwide. 00:22 Obviously, need to know this quite a bit. 00:24 DNA virus with incubation. 00:26 You need to know that hepatitis B is a DNA virus. 00:30 Last time we talked anything about this, at some point in time, is that there is every possibility in chronicity. 00:38 Two major chronic viral hepatites that are important for you and I, for pathology and cancer will be hepatitis B, which is a DNA virus and hepatitis C which would be an RNA virus. 00:52 It’s important that you know what kind of molecular goes on to cancers. 00:58 Transmission here, parental or sexual routes. 01:02 High risk of vertical transmission. 01:04 What does that mean to you? You are thinking about a pregnant lady that is now giving birth; and during delivery, there is every possibility that through the vaginal canal there might be vertical transmission unfortunately to the newborn. 01:16 Think of this as being part of your torch. Hepatitis B. 01:20 Leading risk factor for liver cancer worldwide. 01:24 Also, keep in mind, hepatitis C – and make sure that you know how to identify hepatitis B or C. 01:30 This is a DNA virus. 01:33 Only 5% of adult infection develop chronic hepatitis, while the majority of perinatal infections are chronic. 01:41 So, there are two populations here. 01:43 Very rarely do adults go on to chronicity. 01:47 That would be more hepatitis C. 01:48 C in hepatitis C – C for chronicity. 01:54 However, could you move on to chronicity in hepatitis B? Sure, you can, but a measly 5%. 02:00 Still important, though. 02:02 Now, if a childhood vertical transmission, ohh, that’s a little bit – that’s difficult. 02:07 That's more challenging and there's every possibility or likelihood of a child going on to chronicity. 02:15 Clinical presentation of hepatitis B: Symptomatic disease more severe than hepatitis A, hence we’re going to elaborate on it further. 02:26 Jaundice rarely lasts greater than four weeks. 02:30 So, you’re thinking about – if you find jaundice in a patient with hepatitis B, you’re thinking about, well, this must've been a timeline of approximately one month. 02:39 1% incidence of fulminant hepatitis. 02:42 Thank goodness. 02:46 Move on to extra hepatic manifestations of hepatitis B. 02:50 Here, you do want to pay attention to (inaudible). 02:52 Angioneurotic edema. 02:56 This is important. 02:57 30% of your patients – this patient may come to you and may complain of – ‘doc, my tummy hurts.’ And also, you notice that there's blood in the urine. 03:11 And you find that upon serology, you find an increase in ALT. 03:17 Wow, that's interesting. 03:18 The liver is involved and I'm finding abdominal pain and I'm finding hematuria. 03:27 Should be thinking about polyarteritis nodosa. 03:29 30% of your patients with hepatitis B might actually be suffering from polyarteritis nodosa. 03:35 These would be adults for the most part and the two symptoms that I gave you – hey, doc, my stomach hurts, the abdominal region. 03:42 Radiate to the back? No, nothing like that. 03:44 And I'm finding hematuria. 03:46 So, you need to be – make sure that you’re quite astute with paying attention to your patient with such symptoms. 03:53 And when we you say polyarteritis nodosa, obviously, this is a vasculitis. 03:57 The vascular system that is being affected here would be the mesenteric blood vessel. 04:03 What does that vasculitis mean to you? Inflammation, inflammation, inflammation of your blood vessel until there's occlusion, lack of blood supply to the abdominal region, mesentery, anytime there's ischemia. 04:16 How is the patient feeling? Pain. Pain. So, pain in the abdomen. 04:20 In addition, you have the renal blood vessels might start undergoing microaneurysms and may result in, as I told you, hematuria. 04:30 Keep that in mind. 04:31 Spend a second on polyarteritis nodosa and its association with hepatitis B. 04:37 Also, association with MPGN (membranoproliferative glomerulonephritis). 04:43 So, what does this mean to you? MPGN, what kind of symptoms? Is it strictly nephritic, is it strictly nephrotic or is it both? Both. 04:55 So, there might be hematuria and hypertension and there might be also massive edema and a greater than 3.5 grams of protein loss. 05:03 Allow for each one of these symptoms to give you amazing information for a particular condition, so that you can choose the correct answer. 05:12 Stick with me and I will get you there. 05:15 MPGN, nephritic, nephrotic, type 1 much more common than type 2. 05:21 Now, we can move on. 05:23 Mononeuritis multiplex, that’s interesting. 05:27 Mononeuritis multiplex, what does that mean? One nerve that's being affected, an inflammatory process in multiple, multiple organs. 05:35 Maybe it’s a radial nerve that’s affected, wrist drop. 05:39 Maybe it's the common peroneal nerve, foot drop. 05:42 Just as an example. 05:43 One nerve in which it may affect multiple systems resulting in the sequelae that you would expect to see. 05:52 Important here as well, cryoglobulinemia. 05:55 This is more so found in hepatitis C. I will tell you that right off the back. 05:59 If it’s any type of viral hepatitis that you’re worried about with cryoglobulinemia, what does that mean to you? Allow the name to speak to you. 06:07 Cryo means cold. 06:09 Upon exposure to cold, because of the immunoglobulins that are involved in viral hepatites, that upon exposure to cold, the globulins will do what? Oh, yes. 06:19 They will then precipitate. Right? When they precipitate, this is then referred to as being your cryoglobulinemia. 06:27 During cold conditions, it then aggregates or precipitates. 06:31 Interesting. 06:32 So, two major cold issues that you want to know for your boards and your wards. 06:36 When you're cold and you find that the fingers are now cyanotic – that's Raynaud's – or if you find cryoglobulinemia, cold. 06:46 And oftentimes, whenever you think about or you hear about a patient in which there is ascending paralysis, it's preceded by infection and usually viral. Viral. Gilliam-Barre syndrome.
About the Lecture
The lecture Hepatitis B by Carlo Raj, MD is from the course Liver Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is caused by a DNA virus?
- Hepatitis B
- Hepatitis C
- Hepatitis A
- Hepatitis E
- Hepatitis D
A patient had ischemia of the mesenteric vessels along with hematuria. He also has increased liver transaminase levels. He was diagnosed with polyarteritis nodosa. Which of the following tests must the patient have to assess for associated conditions?
- ELISA for detection of hepatitis B
- ELISA for hepatitis C
- PCR for CMV
- Hepatitis A antigen test
Which of the following is NOT an extrahepatic manifestation of hepatitis B?
- Post-streptococcal glomerulonephritis
- Membranoproliferative glomerulonephritis
- Mononeuritis multiplex
- Polyarteritis nodosa
A patient presents with yellow discoloration of the skin and eyes and ascending paralysis in the feet. The liver transaminase levels show an AST:ALT ratio of 1:2. A diagnosis of hepatitis B infection was made. Which of the following associated conditions is responsible for the patient's paralysis?
- Guillain-Barre syndrome
- Mononeuritis multiplex
- Polyarteritis nodosa
- Multiple sclerosis
- Amyotrophic lateral sclerosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text