Playlist
Show Playlist
Hide Playlist
Endothelium Promotes and Inhibits Thrombosis
-
Slides Thrombus Formation Endothelium.pdf
-
Reference List Pathology.pdf
-
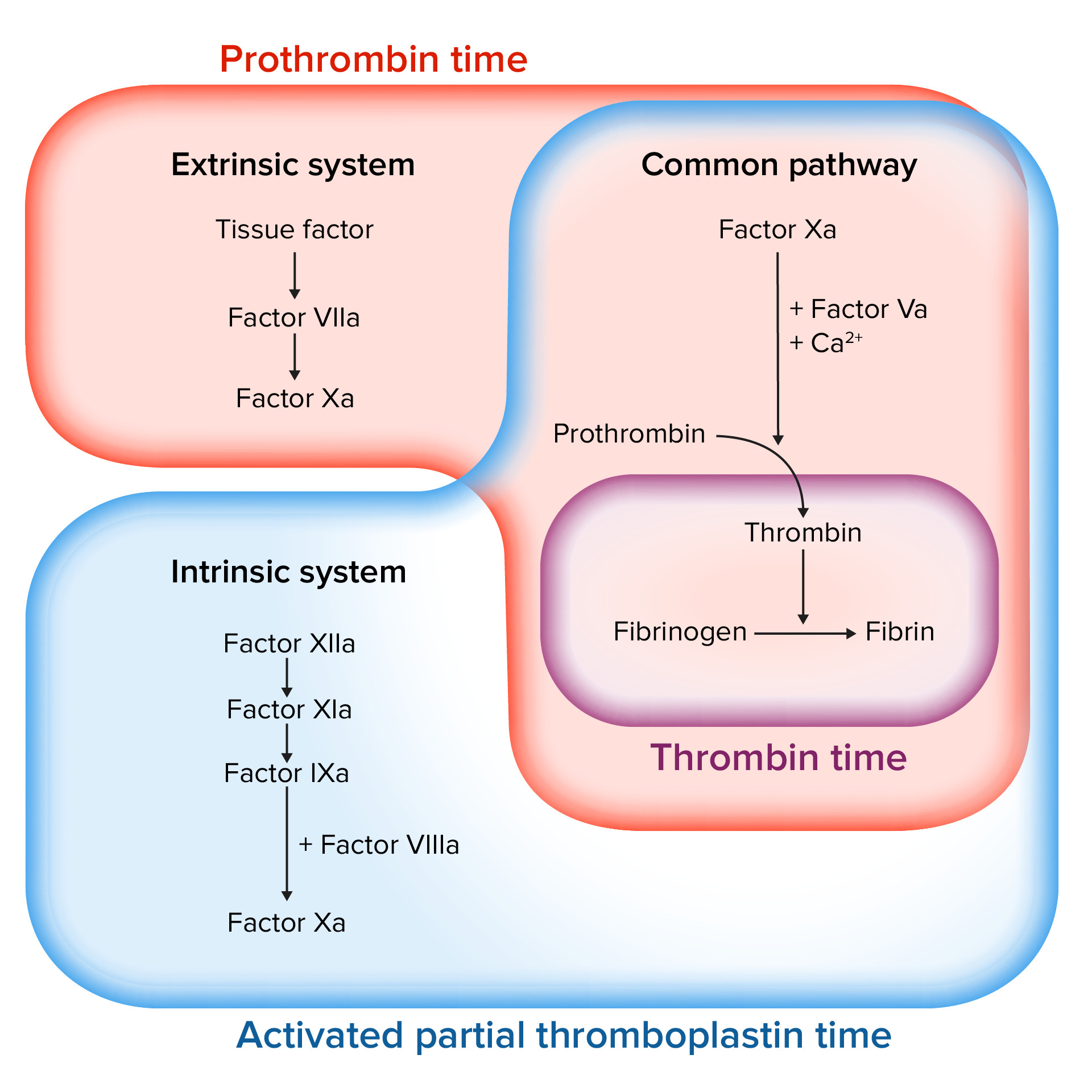
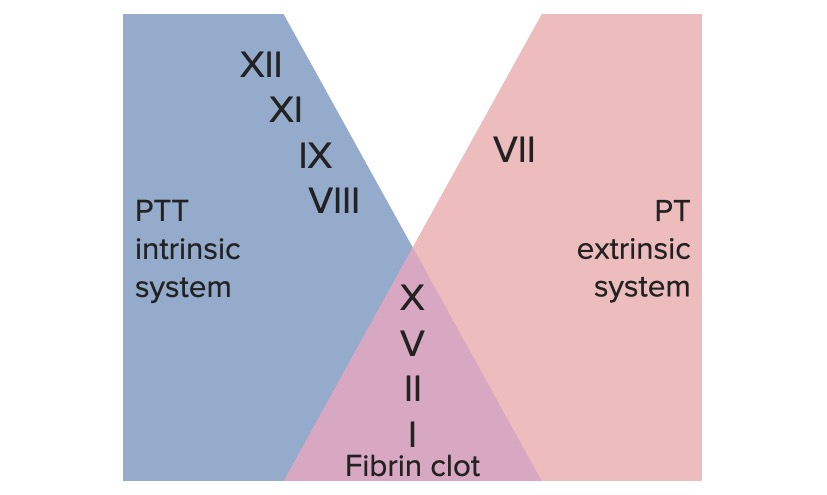
Download Lecture Overview
00:00 Alright, we're going to come now in this session to the final component of the coagulation process. We've talked previously about platelets and their role. We've talked about all the coagulation factors that are in the circulation. And this session deals with endothelium, which is a very important regulatory and counterregulatory component in the grand scheme of things. So here's where we are, back again to our vessel. As I've said, we've talked about platelets, talked about the coagulation cascade, all the multicolored factors, remember all those factors and now endothelium. Okay, by way of review of things that we've talked about but also to bring in some new things. So, endothelium clearly promotes thrombosis. 00:53 Remember it's going to be the source of Von Willebrand factor, VWF, and it's going to be a source of factor VIII. Von Willebrand factor is going to be deposited at those little green dots lining along the collagen that's going to be protein that's going to be very important when the endothelium is lost to allow platelets to adhere via the glycoprotein Ib receptor on the platelets. Factor VIII is going to be a very important part of the coagulation cascade. 01:24 So, normally the rest of the coagulation factors, those are being mostly synthesized in the liver, factor VIII is also made locally. So clearly, endothelial cells contribute to platelet activation, aggregation, and also to the coagulation cascade. Endothelial cells are also important for the extrinsic coagulation cascade. So remember, endothelial cells are going to be a source of tissue factor and that tissue factor is going to be driving extrinsic coagulation. So remember, tissue factor, factor VII, all of that. Okay. So, endothelial cells synthesize tissue factor after they've been stimulated, but they also are covering up tissue factor that lives on smooth muscle cells and lives on fibroblast below the endothelium. 02:20 Okay. So, this combination of effects in an injured vessel is going to lead to platelet adhesion and it's held together finely by the fibrinogen. The platelets remember adhere through their glycoprotein IIb, IIIa receptors and they're held together and then they are going to be cemented altogether by all those polymerized fibrin that's going to be an important kind of link holding the platelet plug together. Even as we are driving thrombosis, we are also inhibiting thrombosis. One last factor that we need to describe is tissue plasminogen activator I. So that activator inhibitor, PAI-1, is going to be important for inhibiting the antithrombotic pathway. Okay, so we have multiple things that endothelial cells are doing to promote clotting. Now, in the next few slides, we're going to talk about the things that they do to inhibit the clotting. Okay, we're going to go from left to right. By the time we finish this slide, we will have filled in multiple things that endothelial cells are doing that inhibit thrombosis. So one of the things that endothelial cells make is they make a heparin-like molecule that interacts with circulating antithrombin III, the green balls, and that will convert that antithrombin III into something that will inhibit thrombin. It also inhibits factors IXa and Xa. So, endothelial cells are making something that will drive the activation of that antithrombin III. Okay, that's one thing. Endothelial cells inactivate the tissue factor VIIa complex because remember they're very upstream driver of the extrinsic pathway so they make something called tissue factor pathway inhibitor, TFPI. And that will block the extrinsic pathway. Endothelial cells have on their surface thrombin receptors. Thrombin is being made activated as part of the coagulation cascade forming that clot out there in the blood vessel lumen it will bind to the thrombin receptor. Remember that proteolysis activating receptor, PAR-1, that's on endothelial cells thrombin binds to that and that will lead to the production of thrombomodulin. Thrombomodulin, much like the name suggests, will convert thrombin to a coagulation inhibitor. Wow. So we're going to take that very potent coagulation driver and flip it on its head and make it an inhibitor of the overall process. And there you have thrombin binding to it and turning over into a different kind of molecule that will work by cleaving additional proteins on the circulation. So, as you can have already expressed probably with yourself "Wow this is complicated." Yes it is. And if I were to design it I'm not sure I would make it quite so complicated but in fact it clearly has worked very well for the vast majority of humans so hard to argue with success. In any event, this thrombin that has been modified by thrombomodulin will act on protein C converting it to an activated protein C. Protein C is synthesized by hepatocytes is in this circulation and it's out there waiting to do its thing when thrombin gets modified. That activated protein C needs another molecule, protein S, and then it becomes an anticoagulation factor and it will inhibit/inactivate factors Va and VIIIa. Okay, so again a feedback inhibition to the entire thrombotic process. Endothelial cells will also make prostaglandin I2 otherwise known as prostacyclin. They will make nitric oxide and they will make adenosine diphosphatase. What are those doing? Well, in fact, those all inhibit platelet aggregation. Prostacyclin is kind of the flipside, the counterregulatory mechanism to thromboxane A2. Nitric oxide will also turn off platelet aggregation. It will also induce vasodilation. And then finally, the adenosine diphosphatase. Remember ADP binds with ADP receptor on the surface of platelets and causes platelet activation? Well, if you break down adenosine diphosphate, ADP. Then you don't get that binding and you don't get the platelet activation. So, another effect that endothelial cells have both on platelets and the coagulation cascade. And finally, endothelial cells make this lovely molecule tissue plasminogen activator or tPA and that actively will break down clots. It actually does fibrinolysis. Remember all those polymerized fibrils? We are now going to cleave those. 08:00 Now it's important that tPA get activated in the total process before we cross link fibrin with factor XIII. However, tPA is being generated almost from the very beginning even as we start the coagulation cascade. So again, the whole goal of coagulation of normal hemostasis is to keep your finger from causing you to bleed to death if you cut it, but at the same time as we stop the bleeding at that site in your finger we will also not thrombose the entire arm. And with that, we have reached the end of this particular session.
About the Lecture
The lecture Endothelium Promotes and Inhibits Thrombosis by Richard Mitchell, MD, PhD is from the course Hemostasis.
Included Quiz Questions
What factor do the endothelial cells synthesize?
- VIII
- IX
- XI
- VII
- VI
What do the endothelial cells inhibit when endothelium favors thrombosis?
- Fibrinolysis
- Platelet adhesion
- Fibrinogenesis
- Tissue factor activation
- Platelet aggregation
What is the function of the heparin-like molecule?
- Inhibits thrombin
- Promotes fibrinogen
- Activates tissue factor
- Activates factor Va
- Promotes platelet adhesion
Thrombomodulin acts as a...
- ...coagulation inhibitor.
- ...platelet aggregator.
- ...thrombolytic agent.
- ...platelet adhesion factor.
- ...tissue factor activator.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |