Playlist
Show Playlist
Hide Playlist
End-Stage Liver Disease
-
Slides GD liver disease.pdf
-
Download Lecture Overview
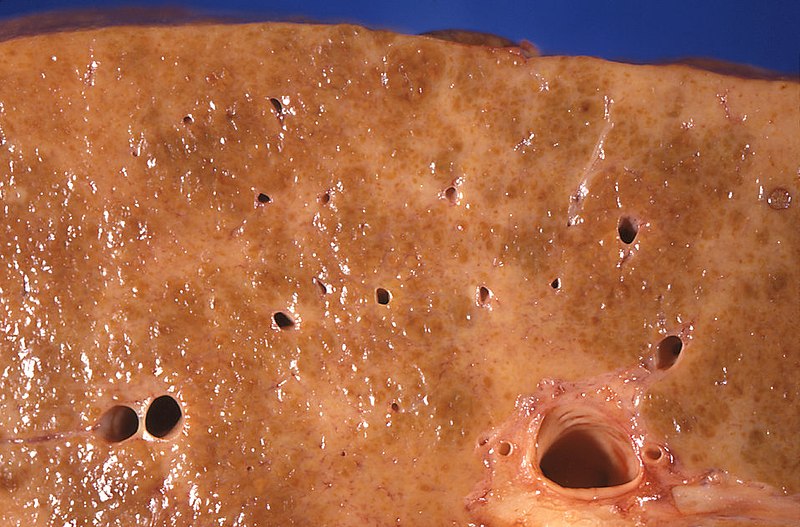
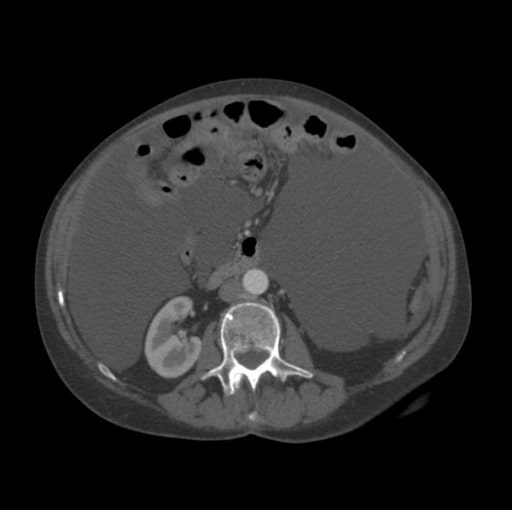
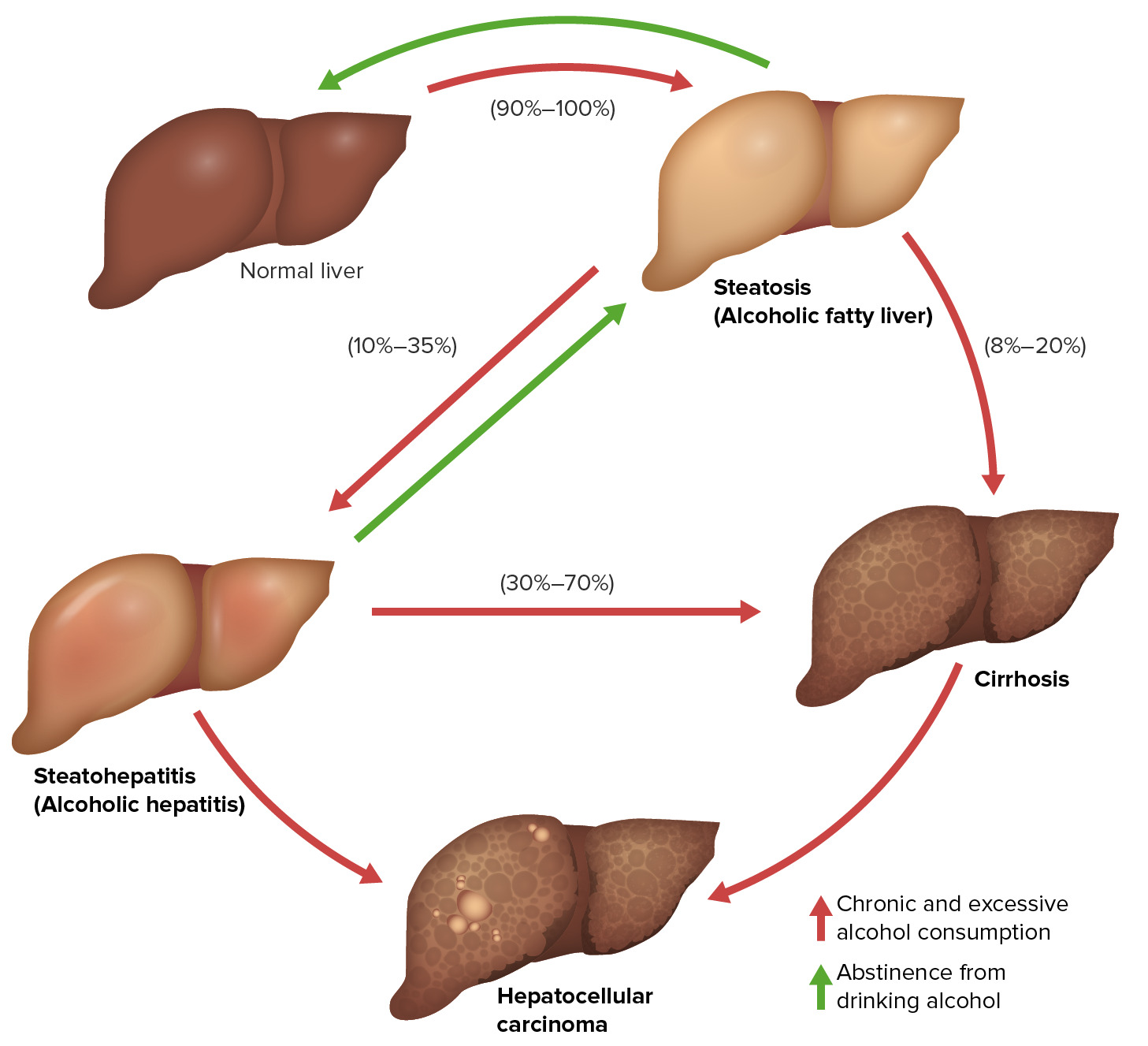
00:02 Our topic of End stage liver disease, and we're going to further detail of cirrhosis, the final common pathway resulting in pretty severe sequelae. 00:12 I will be every once in a while pausing and making sure that we focus on certain concepts that students tend to miss because they overlook it. 00:24 Cirrhosis. 00:25 Final common pathway, progression to irreversible injury due to severe fibrosis which means you are going to find tons of collagen you've heard of trichome stain maybe even reticular stain, and this is specifically for finding fibrosis. 00:41 We'll talk about the clinical consequences in great detail. 00:44 Lots to come. 00:47 Exam. 00:48 When you hear stigmata of cirrhosis we'll walk in each one of these. 00:52 Palmer erythema due to increase estrogen. 00:56 spider angiomata, you've heared *Tangiactasia due to increased estrogen. 01:01 paper money skin, extremely thin. 01:04 bilateral parotid enlargement in addition to other complications we will walk through. 01:09 *gland often associated. 01:12 Here, we have a cirrhotic liver. 01:14 You've noticed that there is a complete loss of that fleshy almost like a pink-like appearance the liver should have. 01:22 In cirrhosis, there will be increase in fibrotic nodules. 01:27 Either micro or macro nodules. 01:29 With all this fibrosis, and the nodules, it looks like, peanut brittle. 01:36 Extremely rough on top. 01:38 The nodules here represent either micro or macro nodules. 01:41 With extensive fibrosis and a shrunken liver. 01:46 So, imagine now that the liver is dead. 01:49 What kind of sequelae are we looking for? Let's begin. 01:54 The consequences. 01:55 Let's begin with synthetic dysfunction. 01:58 Remember that the liver is responsible for producing the most abundant protein in our body, albumin. 02:06 You lose that albumin, hypoalbuminemia due to the lack of synthesis, you lose your oncotic pressure what your patient look like? protruding stomach, what's going on with that? Edema, right? Edema. 02:21 Next. 02:22 Not only is the albumin synthesis been compromised, as is your coagulation factors. 02:28 What are they again? Give me the pro coagulant factors the liver produces. 02:32 II, VII, IX and X. 02:35 The anti-coagulant factors include protein c and protein s. 02:40 Of all of these, II, VII, IX and X which are vitamin K, the test that you are going to use clinically, to find out as to whether or not the function of the liver has been compromised, once again is prothrombin time. 02:54 Once again, please tell me what the time is for prothrombin time. 02:58 11-15 seconds. 03:00 What time is it? Time for you to take your USNLE endocrine what kind of issues are you going to have with cirrhosis and endocrine pathology? The liver is often responsible for metabolizing estrogen. 03:17 If you don't have the liver and it is erratic, your estrogen levels arise. 03:22 Estrogen levels arise especially on a male, impotence. 03:26 hypogonadism, testicular atrophy and gynecomastia you put them all together and what hormone am I referring to? Estrogen. 03:35 This estrogen is going to do what to your blood vessels? It will cause ectasia. What does ecstasia mean? Dilation. 03:42 And what if the pattern of that ectasia looks like spiderlegs? It's called spider angiomata. 03:49 That estorgen is going to cause erythema of the palm. 03:52 Palmer erythema. 03:56 My topic: Dead liver is Cirrhotic liver. 04:00 Let's talk about Cardiopulmonary. 04:02 Interesting. Listen. 04:04 Students get this confused all the time. 04:08 There's one type of hypotension, and massive hypotension. 04:12 in a cirrhotic patient. 04:14 I guess maybe you've got through med school and you just forget that you have two circulations in your body. 04:23 Well, actually, technically, you want to probably want to start thinking about it as three. 04:26 We have our systemic circulation, our pulmonary circulation, and then we have our portal circulation, right? That is how you need to approach this with cirrhosis. 04:37 Follow me. 04:38 In cirrhosis, which we haven't talked about it yet, the portal hypertension we are referring to is esophagal varices. 04:45 I like to use the word "head". You'll see why. 04:48 And they you have hemorrhoids and that is the butt. 04:51 Head, butt and then around the ambilicus we have our kaput. 04:56 Head, butt, kaput, that's portal hypertension. 05:00 That is not our topic yet, but we will come to it. 05:02 I will hit it hard. 05:05 hypotension. 05:08 No such thing as portal hypotension. 05:11 So you will have portal hypertension in cirrhosis but overall, the patient globally, is suffering from hypotension. 05:19 We'll talk about that in great detail. 05:21 Is this clear? I haven't talked about pathogenesis yet but understand your patient will be most likely hypotensive. 05:28 There will be what is known as hepato-pulmonary disease and we'll talk about this. 05:32 And we'll talk about another issue called hepato renal syndrome. 05:41 Let's begin by looking at portal hypertension. 05:44 As I said earlier this will be head, butt, kaput. 05:47 If there is portal hypertension, this will be what kind of force in excess? hydrostatic pressure. 05:54 Dr. Raj, you said that there is decrease in oncotic pressure? I did. 05:58 So, were you wrong? No, I wasn't. 06:00 Really? Watch. 06:02 If you're losing albumin, that is decreased oncotic pressure. 06:05 If you are having portal hypertension, that is increase hydrostatic pressure. 06:09 The combination of the two, what is the stomach that I made? that is ascites. 06:14 Next. 06:16 Of all the three, head, butt, kaput, which one is the emergency? the hemorrhoids? No, it is not. 06:22 I'm sorry, I had to do that. 06:23 It's the esophagial that you are paying attention to. 06:25 Esophagial varices. 06:27 This is the emergency. 06:29 NGI, We talked about teh esophagus in great detail. 06:33 I showed you a number of endoscopic examinations. 06:39 I showed you esophageal varices in the esophagus. 06:42 You saw that there is dilation of the esophageal veins, if that raptures, my goodness, you are going to have hematemesis and there might be choking. 06:54 Meaning to say, the patient is suffocating on his or her own blood. 06:58 That is an emergency. No joke. 07:01 porto-systemic encephalopathy. I'll talk about that in greater detail. 07:04 I will separately, take out. spontaneous bacterial peritonitis. Warrants its own discussion. 07:10 And splenomegaly with thrombocytopenia because their liver gets knocked out, guess what happens to the spleen? Good-splenomegaly. 07:20 I will talk about in greater detail what is known as hepato-renal syndrome. 07:24 It is important that you understand this. 07:25 My topic for all of these four is still cirrhosis. 07:29 Oncologic. Remember please that anytime, anything that causes cirrhosis, the increase of risk for hepatocellular carcinoma. 07:38 On your boards, you are looking for alpha-fetoprotein. 07:42 Ascites is our topic. 07:45 Remember if there is liver damage in cirrhosis, ascites is definitely taking place. 07:50 We'd have to go to the hepatophysiology just make sure that you are clear and there's more. 07:54 in terms of a particular ratio called SAAG. 07:57 As we all shall take a look at. 07:59 So, what is ascites, it is excess fluid of in the peritoneal cavity. 08:05 Two major causes once again; elevated hydrostatic pressure. 08:07 Portal hypertension. 08:09 Due to decrease albumin may result in decrease of oncotic pressure. 08:14 Both of these will contribute to therefore increased amount of fluid in the peritoneal cavity. 08:20 Back to physiology. 08:21 Where is our fluid right now? In the peritoneal cavity. 08:25 Do you know of any blood vessel or vascular system a vascular system at the peritoneal cavity? No. 08:33 So now, you have all these fluid which is not all. 08:37 A lot of it is fluid. 08:38 which escaped the blood vessel and has entered interstitium How much profusion is taking place down to the kidney. 08:48 Not a whole a lot. 08:49 or decreased Or never that you find the * apparatus that then senses the decrease amount of fluid through the arterial what are you going to release? RASS. 09:01 Renin-angiotension-aldosterone axis. 09:04 If you have not corrected the liver issue, you continue to having ascites. More fluid in the peritoneal cavity, thus you are going to have increase aldesterone which does what? reabsorb more sodium or water. 09:18 You've put this all together. I've done this for you many times. 09:22 Right sided heart failure. Nephrotic syndrome and cirrhosis. 09:24 You tell me, what is the common denominator for those three. 09:28 fluid in intertisium decreased in profusion in kidney. 09:35 If you do not the underlying cause, you're going to continue accumulating, fluid in the interstitium. 09:42 In this case, the peritoneal cavity. 09:46 Ascites, clinical presentation, abdominal girth. 09:50 Bulging flanks. 09:52 I have that even without ascites. 09:53 Shifting dullness and fluid wave indicate >500cc. What does that mean? You stand up here, you push the side of their flank, you walk to the other side, and watch the wave come towards you. 10:05 I'm joking. That doesn't actually happen. 10:07 Shifting dullness. You get the point? Because of their fluid, Quite a bit, look at this, greater than 500cc, where? in the peritoneal cavity. Next. 10:18 You think it's possible. 10:20 you think that you might actually end up accumulating fluid elsewhere on some other cavities? especially the pleural activity. 10:27 And we talked about the pleural cavity being an interesting place of developing, hydrothorax. 10:32 You have to refer to this as being, Hepatic hydrothorax. Why? Because you can have malignant hydrothorax. Secondary to ovarian cancer. 10:44 You can have something like Meigs syndrome. 10:47 So, a lot of interesting about pleural effusion. 10:50 We spent time with pleural effusion. 10:52 Investigating transti date versus exit date. 10:57 This is hepatic hydrothorax. 11:00 Management. 11:02 I'll walk you through SAAG. 11:05 But before we get there, At least for now, Memorize the following. 11:10 SAAG. I'll tell you what that stands for. 11:12 Serum Albumin Ascites Gradient But you find it to be greater than 1.1. 11:16 Don't worry. If you didn't catch that, not to worry. I have a table upcoming that goes to greater detail. 11:22 New Entry 192 For now, if you find that your SAAG is greater than 1.1, this to you should indicate portal hypertension. It is that clear. 11:30 The diagnostic evaluation well, if you are thinking about management, and it is not portal hypertension, wouldn't it be good to recommend sodium restriction? Diuretics. 11:45 Why specifically Spironolactone because in a patient with ascites, What do you expect their aldesterone levels to be? High. 11:53 What do you know about Spironolactone? It blocks aldesterone. 11:56 In addition, you have this fluid, remember when you had a pulmonary edema? What kind of loop diuretic did you use to get rid of that fluid? Ah, Furosemide. 12:08 Beginning with 100mg. A little bit more detail here. 12:11 Monitor electrolytes constantly. That is huge. 12:14 And can cause painful gynecomastia as you remember. 12:18 Remember the side effects that may occur with sprinolactone. Gynecomastia is a possibility. 12:23 Why do you want to monitor electrolytes? Because you are using it diuretic. 12:26 And using a aldesterone blocker so therefore, you might have, excess sodium being removed and such. 12:34 Large volume paracentesis with albumin replacement. 12:39 This is accomplished due a large volume needle. 12:41 Placed under ultrasound guidance, or with translumination. 12:44 These needles are then connected to vacuum sealed containers, which induce a negative pressure drawing the fluid into the bottle. 12:52 Here is an important concept. 12:55 It used to be a more high level type of question but you can expect this on your basics. 13:01 It is called transjugular. 13:04 Intrahepatic Porto-Systemic Shunt. New Entry 224 Your main focus here should be, the fact that you are bypassing the liver which is dead. 13:16 It's cirrhotic. 13:18 Here is my problem: So, you are bypassing the liver with a cirrhosis. 13:24 Because you are waiting for a liver transplant. 13:29 So, you're kind of stuck. 13:31 You have to do something in the meantime, to bypass the liver circulation. 13:36 If you bypass the liver circulation, And go straight in to systemic circulation, There is every possibility of tips. 13:44 You'd probably seen the acronym TIPS. 13:48 Or TIPSS. 13:51 It's the fact that when you are bypassing your liver, that you would actually get amonia up into the head. 13:57 And you migh facilitate, or exacerbate hepatic encalophaty. 14:02 But one of those things where you have to take a look at risks vs benefits. 14:06 Because your patient is already cirrhotic. 14:12 Here we have the prognostic scoring in cirrhosis. 14:15 One is called Child-Pugh-Turcotte scoring. 14:18 and the other one is called your MELD. 14:21 At this point, just understand the concept. 14:23 The liver is dead. 14:25 Your arterial pH is less than 7.3. 14:28 And you have Ascites, encephalopathy, bilirubin, albumin levels being decreased, Elevated PT and bilirubin will be elevated. 14:36 All the concepts that we talked about earlier. 14:38 I won't sit here and memorize this table. 14:40 Because you already know all of these. 14:43 On the other side, something called MELD. 14:45 Model for end stage liver disease. 14:47 And for this, you find the PT to be quite elevated. 14:51 You might have renal damage called hepato-renal syndrome, which we'll talk about. 14:55 Creatinine will be elevated and PT will be elevated with INR.
About the Lecture
The lecture End-Stage Liver Disease by Carlo Raj, MD is from the course Liver Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which hormone is responsible for palmar erythema in a patient with cirrhosis?
- Estrogen
- Testosterone
- Epinephrine
- Norepinephrine
- Histamine
Which of the following examination findings is NOT related to the cirrhotic liver?
- Essential tremor
- Palmar erythema
- Spider angiomata
- Bilateral parotid enlargement
- Gynecomastia
Which of the following is NOT a feature of gross examination of a cirrhotic liver?
- Enlarged liver
- Shrunken liver
- Micronodules
- Macronodules
- Firmness in consistency
Which of the following is the MOST likely mechanism of formation of ascites in the cirrhotic liver?
- Decreased oncotic pressure
- Decreased hydrostatic pressure
- Lymphatic obstruction
- Decreased sodium and water retention
- Inflammation
Which of the following coagulation factors will NOT be decreased due to liver cirrhosis?
- Factor VIII
- Factor II
- Factor VII
- Factor IX
- Factor X
What is the cause of thrombocytopenia in cirrhotic liver disease?
- Pooling and sequestration of platelets
- Destruction of platelets
- Consumption of platelets
- Decreased formation of platelets
- Decreased release of platelets from bone marrow to peripheral blood
A 50-year-old man who is an alcoholic had been diagnosed with cirrhosis about 4 years ago. His alpha-fetoprotein levels have increased over 6 months. Which disease is the patient most likely at risk for?
- Hepatocellular carcinoma
- Cholangiocarcinoma
- Pancreatic adenocarcinoma
- Gallbladder carcinoma
- Gastric carcinoma
Which of the following has an increased SAAG ratio of more than 1.1?
- Portal hypertension
- Sarcoidosis
- Henoch-Schonlein purpura
- Secondary peritoneal carcinomatosis
- Primary peritoneal mesothelioma
A patient has cirrhosis and is selected for a liver transplant. Which procedure can be performed to control the symptoms of cirrhosis?
- Transjugular intrahepatic portosystemic shunt (TIPS)
- Whipple's procedure
- Endoscopic retrograde cholangiopancreatography
- Magnetic resonance cholangiopancreatography
- Transhepatic cholangiography
Which of the following is NOT part of the Model for End-stage Liver Disease (MELD) prognostic scoring for cirrhosis?
- Potassium
- PT > 100 seconds
- INR > 7.7
- PT/INR
- Creatinine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lecture , excellent review of all the diseases shown in the video