Playlist
Show Playlist
Hide Playlist
Diabetic Neuropathy with Case
-
Slides 02-03 Diabetes Mellitus part 2.pdf
-
Reference List Endocrinology.pdf
-
Reference List Diabetes Mellitus.pdf
-
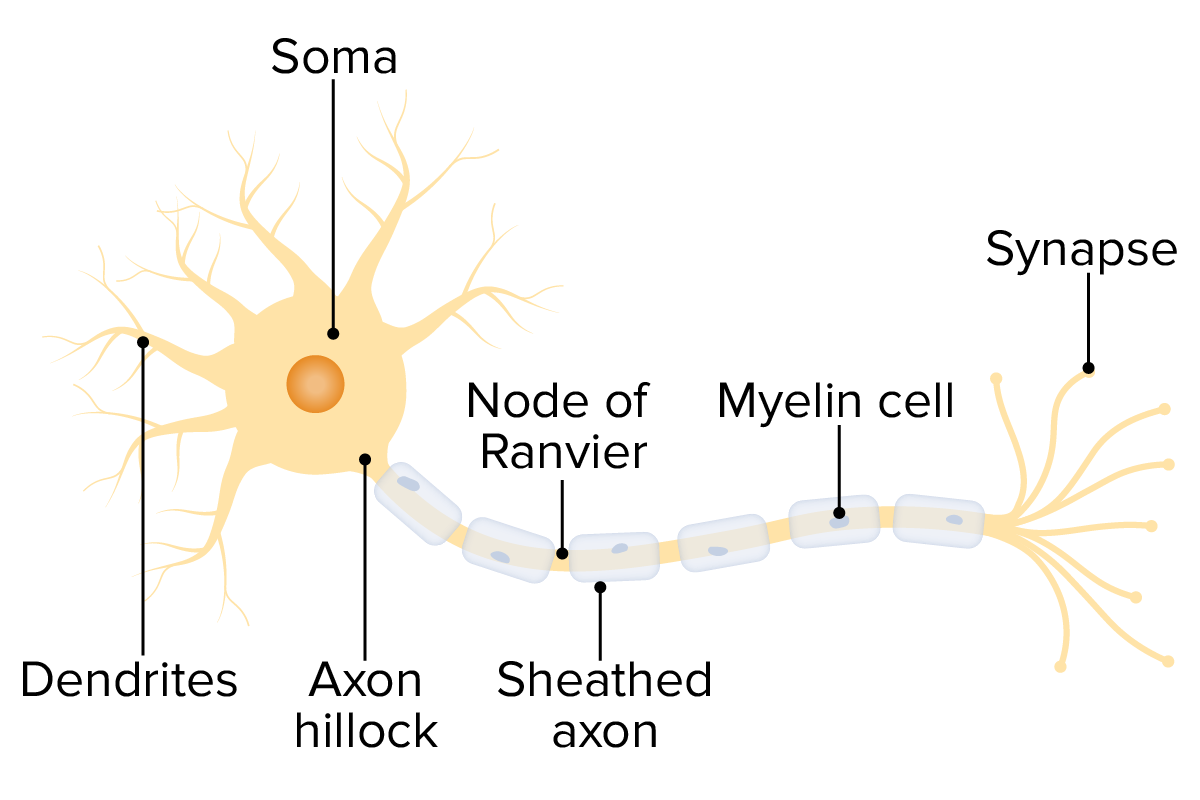
Download Lecture Overview
00:00 Let's go on to another case. Here, a 55-year-old man presents with burning and shooting pains in his feet and lower legs, which becomes more severe at night. In the past 6 months, the pain has become much worse and disturbed his sleep. He has type 2 diabetes mellitus for 12 years and essential hypertension for 5. What is the most likely etiology of this patient's condition? This patient has distal symmetric sensorimotor polyneuropathy due to his longstanding diabetes. In this condition, pain is often worse at night and may be described as lancinating, prickling, gnawing, or excessively sensitive. Early symptoms typically involve the tips of the fingers and toes, which proceed proximally leading to a stocking glove pattern of pain and sensory loss. If nociceptors fibers are affected, loss of feeling may occur and may result in painless injuries. There are several categories of diabetic neuropathy which may present separately or in combination. Symptoms of diabetic neuropathy depend on the nerves or nerve root that is affected and may present as a focal or diffuse disease. Early optimal glycemic control can prevent the development of neuropathy and sustained optimal glucose levels can delay the progression of neuropathy. In the image on the right, you can see the classic presentation of glove and stocking peripheral neuropathy. The condition as it worsens and with worsening glycemic control will then progress both up the arm and up the leg respectively. The classification of diabetic neuropathy consists of the diffuse variety, which is the most common, and this is distal, symmetric, and sensorimotor polyneuropathy as well as autonomic neuropathy. Mononeuropathies or involvement of just single nerves may also occur. 02:00 These may be isolated or involve peripheral nerves. The cranial nerves II, the ulna, media, and then femoral nerves as well as peroneal nerves are commonly involved. And then finally the mononeuritis multiplex, which is a single nerve involvement which is isolated from other nerves. 02:21 Radiculopathy or polyradiculopathy may also occur. This may present as a truncal radiculopathy or a diabetic amyotrophy. In this case, they will be proximal muscle weakness, which is a hallmark of this condition. Muscle weakness may also occur in severe cases. It is a risk factor for muscle and joint deformities otherwise known as Charcot foot or diabetic foot ulcers. Assessment for ankle reflexes, vibration sensation with 128 Hertz tuning fork and fine touch with a 10g monofilament as well as pinprick sensation are required. In these images, you see a severe Charcot joint. If you look at the ankle of this patient, you can see that there is gross deformity of the architectural structure. You can also see laxity of the ligaments as demonstrated on the image on the right. There is also a chronic diabetic foot ulcer on the lateral aspect of his right foot. 03:27 We can treat diabetic neuropathy with antidepressants, anticonvulsants of which the most common is gabapentin, or topical capsaicin cream which can provide mild to moderate relief. Let's talk a little bit about autonomic neuropathy. Symptoms of autonomic neuropathy may be single organ or multiple organ. Gastroparesis, diarrhea, constipation, neurogenic bladder, abnormal sweating and erectile dysfunction are features of diabetic autonomic neuropathy. Cardiac manifestations include resting sinus tachycardias, orthostatic or postprandial hypotension which is low blood pressure after eating, exercise intolerance or even silent myocardial infarction. Cardiovascular autonomic neuropathy is an independent risk factor for mortality in diabetics. Patients with type 1 diabetes for 5 or more years and all patients with type 2 diabetes need to have an annual assessment. Medical history and clinical exam followed by testing of temperature, pinprick sensation for small fiber function, vibration sensation using a tuning fork to assess large fiber function, and an annual 10g monofilament testing to identify the feet that are at risk for ulceration and amputation.
About the Lecture
The lecture Diabetic Neuropathy with Case by Michael Lazarus, MD is from the course Diabetes Mellitus. It contains the following chapters:
- Case: 55-year-old Man with Pain in Feet and Legs
- Diabetic Neuropathy
- Autonomic Neuropathy
Included Quiz Questions
What is the most likely diagnosis in the following patient? A 55-year-old man presents with burning and shooting pains in his feet and lower legs, which become more severe at night. In the past 6 months, the pain has become much worse and disturbs his sleep. He has had type 2 DM for 12 years and essential hypertension for 5 years.
- Diabetic neuropathy
- Guillain-Barre syndrome (GBS)
- Diabetic myelitis
- Diabetic myopathy
- Secondary syphilis
What is the most common presentation of diabetic neuropathy?
- Symmetric polyneuropathy in stocking-glove distribution
- Symmetric polyneuropathy spreading outward from the torso
- Isolated mononeuropathy commonly affecting a cranial nerve
- Truncal radiculopathy with proximal muscle weakness
- Foot ulcer
What is not a component of a usual diabetic foot examination?
- Proprioception testing
- Monofilament testing
- Pinprick testing
- Vibratory testing with a tuning fork
- Ankle reflexes
What is the most likely cause of the following patient's condition? A 55-year-old man presents with burning and shooting pains in his feet and lower legs, which become more severe at night. In the past 6 months, the pain has become much worse and disturbs his sleep. He has had type 2 DM for 12 years and essential hypertension for 5 years.
- Neuropathy due to long-standing diabetes mellitus
- Neuropathy due to long-standing hypertension
- Diabetic foot
- Peripheral vasculitis due to long-standing hypertension
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |