Playlist
Show Playlist
Hide Playlist
Diabetic Ketoacidosis with Cases
-
Slides 02-03 Diabetes Mellitus part 2.pdf
-
Reference List Endocrinology.pdf
-
Reference List Diabetes Mellitus.pdf
-
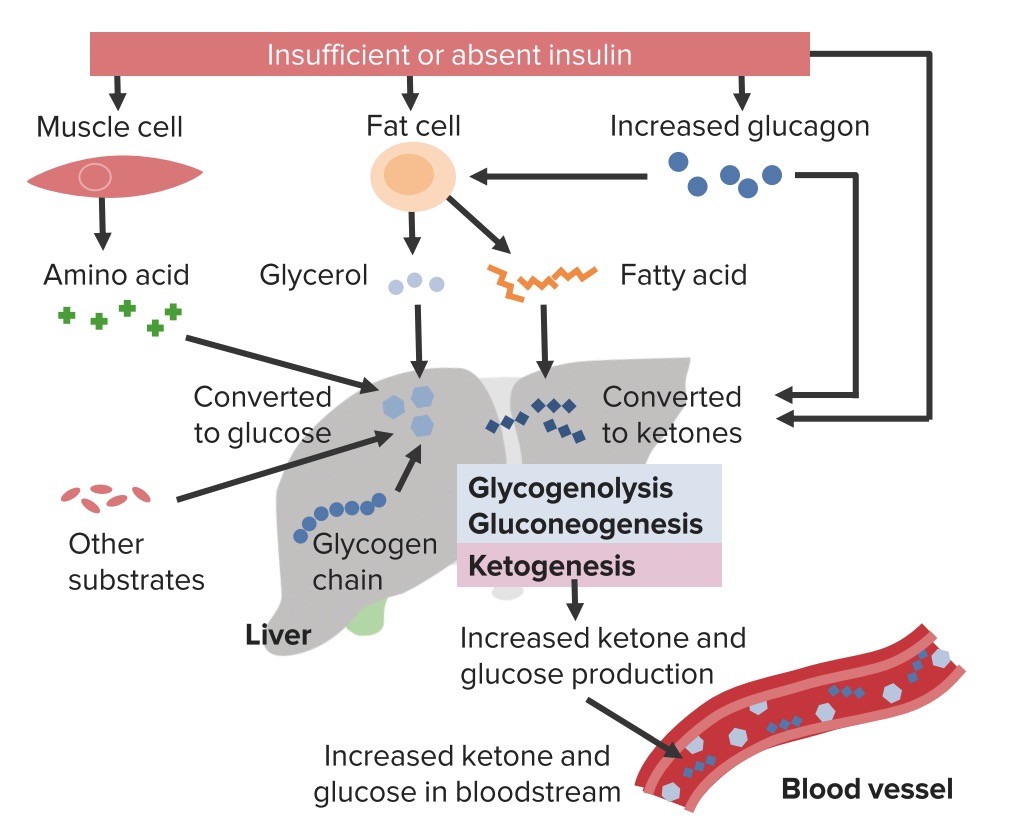
Download Lecture Overview
00:00 The acute complications of diabetes mellitus include diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome. Acute complications of uncontrolled hyperglycemia with life-threatening consequences can occur if not recognized and treated early. Let's go to this case. A 10-year-old boy is brought to the emergency department by his mother due to frequent vomiting, abdominal pain, and weakness. Over the last 5 days, he felt excessively thirsty and has been urinating frequently. 00:33 Family history is non-contributory. His temperature is 37.1°C, his blood pressure is 80/55, and his pulse rate 110 beats/minute. On physical exam, he is non-responsive to verbal commands. 00:47 He has sunken eyes, poor skin turgor, and rapid deep respirations. His lab findings reveal a random plasma glucose of 460 mg/dL. He has an undetectable fasting C-peptide, his serum beta-hydroxybutyrate is elevated, and his GAD antibodies are positive. What is the most likely diagnosis? This is a young boy with vomiting, abdominal pain, and weakness that is progressive. He also manifested with polydipsia and polyuria. Signs of dehydration and tachypnea, that is shallow and rapid respiration, are also present which makes us suspect a respiratory alkalosis. He also has profound hyperglycemia. The presence of undetectable fasting C-peptide is an indication that he has no endogenous insulin production. Also, the fact that his serum ketones are elevated confirms the presence of diabetic ketoacidosis. And finally, the positive GAD antibodies imply that the etiology of his type 1 diabetes is an immune-mediated process. And confirming the diagnosis, this young boy has presented in acute diabetic ketoacidosis. DKA typically occurs in the setting of hyperglycemia with relative or absolute insulin deficiency and an increase in counter-regulatory hormones. 02:18 Sufficient amount of insulin are not present to suppress lipolysis and oxidation of free fatty acids. This in turn leads to ketone body production by the body and a subsequent metabolic acidosis. 02:32 DKA occurs more frequently with type 1 diabetes, although 10-30% of it can occur in patients with type 2 diabetes. It may be the initial clinical presentation in some patients with previously undiagnosed type 1 or type 2 diabetes. 02:49 This next case highlights an increasingly recognized form of diabetic ketoacidosis - euglycemic DKA. 02:57 While our patient illustrates the SGLT2 inhibitor variant, it's crucial to understand that euglycemic DKA can occur in several important clinical scenarios. 03:09 Our patient, a 45-year-old woman, presented with nausea, vomiting, and poor oral intake while continuing her empagliflozin. 03:19 Her labs revealed the diagnostic challenge: a near-normal glucose of 145 mg/dL despite significant ketoacidosis, with a pH of 7.21, anion gap of 22, and elevated beta-hydroxybutyrate of 5.8 mmol/L. 03:39 But here's the broader perspective: euglycemic DKA isn't limited to SGLT2 inhibitor use. 03:47 We see it in several other important clinical scenarios: pregnant women, where metabolic demands are altered; patients who've received insulin just before presenting to the ED; and in any patient with prolonged poor oral intake. 04:02 The common thread is the presence of ketoacidosis without the classic severe hyperglycemia we typically expect in DKA. 04:12 The key teaching point is that we can't exclude DKA based on glucose levels alone. 04:17 Whether it's a pregnant patient with nausea, someone who took their insulin but couldn't eat, or a patient on an SGLT2 inhibitor, we need to maintain a high index of suspicion when the clinical picture suggests ketoacidosis, even if the glucose isn't markedly elevated. 04:36 Management principles remain the same across all these scenarios – these patients need both insulin to reverse the ketoacidosis and glucose supplementation to prevent hypoglycemia during treatment. 04:50 The recognition of euglycemic DKA in any of these settings can be lifesaving.
About the Lecture
The lecture Diabetic Ketoacidosis with Cases by Michael Lazarus, MD is from the course Diabetes Mellitus. It contains the following chapters:
- Complications of Type 2 DM
- Case: 10-year-old Boy with Vomiting and Abdominal Pain
- Diabetic Ketoacidosis
Included Quiz Questions
What is the significance of an undetectable c-peptide level in a patient?
- Decreased endogenous insulin production, suggesting type 1 diabetes
- In conjunction with an elevated plasma glucose level, it suggests the surreptitious injection of a family member's insulin
- Increased endogenous insulin production, suggesting type 2 diabetes
- A high level of insulin resistance, suggesting type 2 diabetes
- Production of insulin from somewhere other than the pancreas, such as an insulin-producing neuroendocrine tumor
By what mechanism are ketone bodies produced?
- Low insulin levels cause the body to obtain energy through the oxidation of free fatty acids, of which ketone bodies are a byproduct.
- A large gap metabolic acidosis induces the release of ketone bodies.
- Insulin resistance directly causes the pancreas to produce ketones.
- Ketoacidosis occurs randomly in patients with type 1 and type 2 diabetes.
- High levels of insulin stimulate the breakdown of fats, which in turn causes the release of ketones.
What is the most likely diagnosis in the case described below? A 10-year-old boy is brought to the emergency department by his mother because of frequent vomiting, abdominal pain, and weakness. Over the last 5 days, he felt excessively thirsty and has been urinating frequently. Family history is noncontributory. Physical examination results: Temperature is 37.1°C (98.7°F), blood pressure is 100/70 mm Hg, pulse is 110 beats/min. He is nonresponsive to verbal commands and has sunken eyes; poor skin turgor; and rapid, deep respirations. Laboratory test results: Random plasma glucose level of 460 mg/dL, undetectable fasting C-peptide, elevated serum beta-hydroxybutyrate level, and positive results for antiglutamic acid decarboxylase (GAD) antibodies
- Diabetic ketoacidosis
- Myxedema coma
- Hyperosmolar hyperglycemic state
- Type 1 diabetes mellitus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |