Playlist
Show Playlist
Hide Playlist
Diabetic Ketoacidosis (DKA) – Diabetes Complications
-
Slides AcuteChronicDiabetesComplications EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
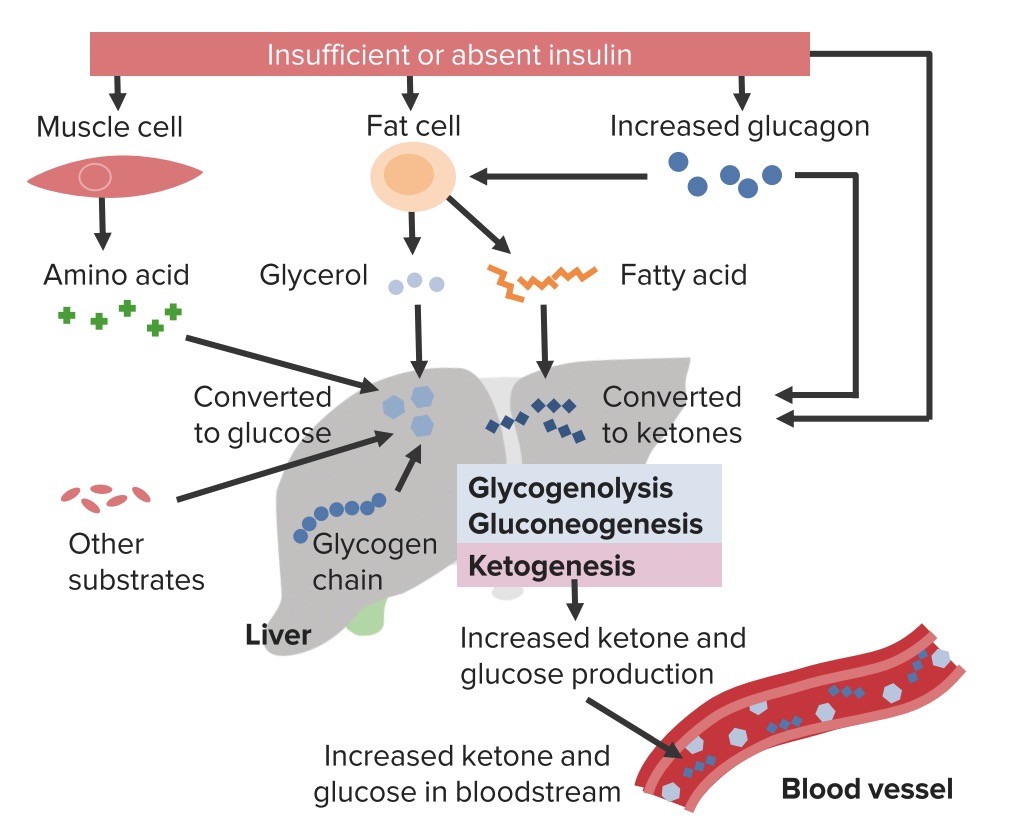
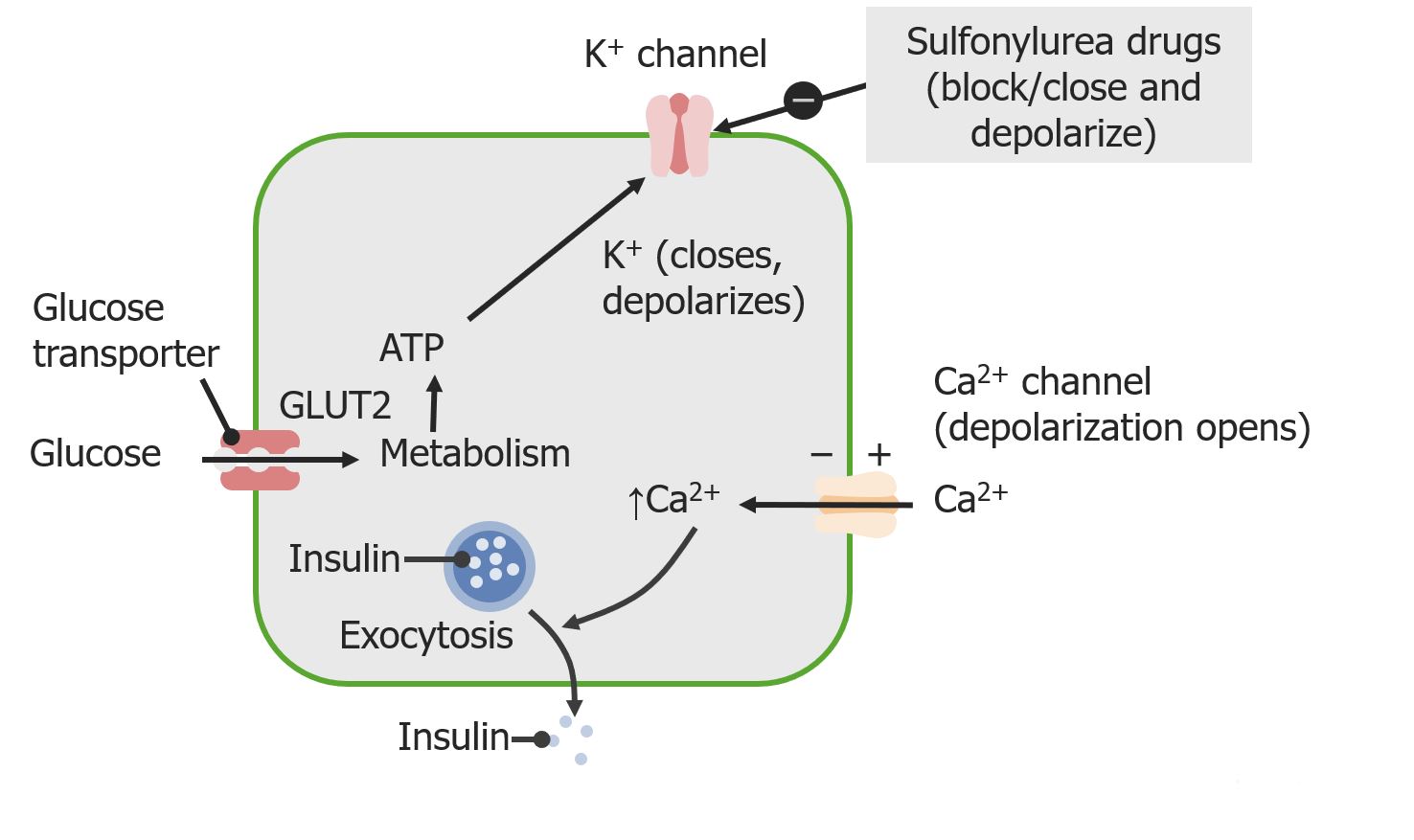
00:01 We had looked at this earlier, but let’s just make sure that we’re clear about the complication of diabetic ketoacidosis. 00:06 Remember, it’s much more common or it could be more commonly found with uncontrolled type I diabetes and in type II diabetes, it could be found under severe stressful situations. 00:18 For example, if you have a type II diabetic who is then undergoing surgery, that’s quite a bit of stress that the patient’s feeling. 00:25 So, therefore, during that time, if poorly controlled, type II diabetic may start getting into a state of diabetic ketoacidosis. 00:33 So, what does this mean to you? Biochemically, it means that your breaking down lipid, you’re forced to do so. 00:41 Would you please take a look at the picture on your right. 00:44 I want you to take a look at the title of this illustration. 00:49 In other words, you’re absent of insulin or insufficiency of insulin. 00:55 Now, in your head, you should be thinking about a seesaw and by seesaw I mean, the balance between insulin and the counter-regulatory hormones referring to your stress hormones and specifically which one would that be here? Glucagon and whenever you have glucagon, then you must be thinking permissive action with cortisol. 01:16 If glucagon is now winning this battle or found to be in greater abundance, you would expect your muscle to start breaking down glucagon, you would expect your lipids to start breaking down… welcome to lipolysis, beta oxidation within the mitochondrial matrix all because of increased glucagon. 01:33 Let’s walk down further. 01:35 What do you end up finding when you breakdown your lipid as triglycerides? Focus on the middle cell, please, and the glycerol would be your backbone and the tri referring to your three fatty acids, these are all being broken down. 01:50 In the meantime, in the liver, what kind of things are taking place here? Converted to glucose amino acid is because glucagon is then in the liver which is your middle structure here, in the grey is undergoing gluconeogenesis, isn’t it? What’s my topic? Diabetes mellitus, uncontrolled… diabetic ketoacidosis. 02:11 Your patient… how much glucose is in your plasma in DKA? Is it 50 with plasma and glucose or would it be a concentration of maybe 400 or 500? The latter, 400, 500 or 600… absolutely uncontrolled type I or type II diabetes mellitus. 02:34 With all that said, if that’s your end objective, take a look at the bottom right corner there and you find the blood vessel. 02:42 You would expect there to be hyperglycemia and with uncontrolled diabetes, you’ll also expect your ketones or ketoacids, beta-hydroxybutyric acid, acetoacetic acid and a little bit of acetone to be also deposited into your plasma. 02:58 Once you have these ketoacids inside your blood vessel, then at this point, you endogenously produce acids. 03:05 We will then call this metabolic acidosis, you would expect to find your bicarb to be less than 22 and quite remarkably depressed. 03:15 Remember, whenever you deal with metabolic acidosis, you are focusing upon bicarb. 03:21 Normal level bicarb is between 22 to 26, if you remember. 03:25 If you find your bicarb to be 18, 15 whatnot, then you know that you’re in a state of metabolic acidosis. 03:32 You will always confirm this by looking at the pH which would definitely be less than 7.35… might be 7.3, 7.2, right? Metabolic acidosis. 03:45 Protein catabolism to glucose and can also be seen as starvation, but think type I diabetes more so with diabetic ketoacidosis. 03:59 Further let’s give you an overview of the complications that you can expect with uncontrolled diabetes mellitus. 04:07 What’s your insulin level in this patient, please? Depressed or maybe completely absent. 04:12 You’re going to breakdown your protein, muscle wasting. 04:16 Your second line in the liver gluconeogenesis... in the liver glycogenolysis because we don’t have insulin, all these results in increased glucose into circulation. 04:29 In addition, take a look at the balance here in the box in the grey, you have decreased insulin and the counter-regulatory hormones have increased. 04:38 These include your glucagon and epinephrine. 04:41 All of these is then going to contribute to hyperglycemia and DKA, as I told you, could be ridiculously high. 04:51 Now, just to make sure we’re clear, your next step of management, management becomes big time important, doesn’t it? So, your next step of management here with such massive or exaggerated hyperglycemia, meaning to say that your patient is severely and extensively filtering all these glucose into the urine, drawing in all this water… welcome to osmotic diuresis. 05:18 You might be losing up to six litres of water or urine per day, what’s your next step of management? IV fluids. 05:26 Keep that in mind, we’ll talk about this again. 05:29 Lipolysis taking place resulting in beta oxidation; you have ketoacidosis… metabolic. 05:34 Now, here, when there’s metabolic acidosis and your bicarbs maybe 18 or 16 or whatnot and then immediately minutes thereafter, what is your breathing rate? Your respiratory rate would be increased because you’re trying to compensate by decreasing carbon dioxide. 05:53 How did you decrease your carbon dioxide? You blow off your… you blow it off in a rapid rate, whooh, whooh, whooh, whooh. 05:59 And when you do so, this breath that you’re smelling from patient with diabetic ketoacidosis... 06:05 sweet odour, huh, sweet odour, why? Because of that acetone, we call this kussmaul’s breathing. 06:13 Important here more biochemistry as to integration. 06:19 First and foremost, you want to keep in mind for pathology, three different lipases that we have in our body. 06:28 In gastro, we talked about the three different lipases, we definitely talked about them in vascular pathology. 06:36 In the pancreatic lipase, we have lipoprotein lipase, we have hormone-sensitive lipase… remember those. 06:43 Make sure that you know each and every single one of those and its clinical significance. 06:47 The pancreatic lipase as you know is used as a marker as far as you’re concerned for pancreatic damage specifically pancreatic lipase. 06:56 Then we have lipoprotein lipase which is our discussion here. 06:59 Lipoprotein lipase is found within the peripheral blood… in the blood. 07:03 What’s the third type of lipase that I mentioned? Hormone sensitive lipase. 07:08 Do you remember these? Keep all three separate. 07:11 At this point, our discussion is lipoprotein lipase also called capillary lipoprotein lipase located in your blood vessel. 07:18 It’s responsible for doing what? It’s responsible for metabolising your triglycerides into the respective free lipids and what that means is that if you’re taking up lipid from the diet, you’re forming chylomicron. 07:34 The chylomicron is then put into circulation and guess who works upon your chylomicron? Your lipoprotein lipase so you can then extract your triglycerides. 07:44 Clear? Number two, if you’re moving from the liver out towards your tissue, that’s VLDL and that also is worked upon by or acted upon by lipoprotein lipase. 07:58 So, extracting all the triglycerides… lipoprotein lipase is… what’s my point? In a diabetic patient, especially DKA, what do you expect their triglyceride levels to be? Really high, really high, really high. 08:13 So, what I’m trying to say is if you don’t have the insulin, you have decreased activity of your lipoprotein lipase, you’re not able to properly extract your triglycerides from the respective packages or vessels, chylomicron or VLDL, this would then remain back in your circulation contributing to hypertriglyceridemia; increased chylomicron, increased VLDL leading into clinical significance or finding of hypertriglyceridemia. 08:44 Each one of these points here with complications that we find with diabetes mellitus, extremely important from a biochemical point of view. 08:54 It’s a beautiful overview of things that you want to keep in mind and integrate. 08:58 If you feel weak at any point here, please go back and refer to biochem, physio whatnot… make sure you know the normal first so you can understand the abnormal. 09:08 So, DKA is more common in type I characterized by hyperglycemia and anion gap metabolic acidosis. 09:14 What is the anion gap? The formula is one major cation clinically, one major cation. 09:21 “What about potassium, Dr. Raj?” Hmm, 3.5 to 5.0; use it if you wish, clinically though, you will be using sodium 135 to 145. 09:31 From this, you subtract your anions… there are two of them, you’re going to take both into consideration. 09:36 These then include your chloride 95 to 105 plus what’s the other major anion? Bicarb, between 22 to 26. 09:45 If you’re weak in this area, I’d recommend that you go back and take a look at your acid-base physiology. 09:51 Ketonemia, of course, and anion gap. 09:54 Fatigue, blurred vision and polydipsia, polyuria… yeah, lots of polyuria… lots. 10:00 Nausea, vomiting, abdominal pain; kussmaul’s respiration and fruity breath. 10:06 What does that even mean? Remember this is compensation, you’re trying to blow off the carbon dioxide. 10:12 The common precipitants… new onset diabetes, inadequate insulin use or infections. 10:17 What’s happening, what’s predisposing the patient into DKA? The patient just started developing diabetes, completely exhausted insulin either from type II perhaps rarely, but could happen especially under stressful situations and definitely type I. 10:33 Remember, you could be in your 20’s and still develop type I diabetes mellitus. 10:37 New - onset, the patient doesn’t know that he or she is suffering from it, all of a sudden resulting in DKA; inadequate insulin use, infection. 10:47 Let’s talk about management. 10:52 First step, make sure that you replenish the fluid… IV fluids. 10:58 Oftentimes three to six litres, that’s how much this patient is urinating all over the place. 11:06 Add dextrose to IVF when glucose is less than 200 and what that means is the following. 11:11 What’s occurring is the fact that you’re giving fluids and initially with all of that fluid that is then being given, there’s every possibility that along with this obviously you’re going to give insulin infusion, right? Now, as you give insulin, what then happens to this glucose? It rapidly, rapidly, rapidly decreases and if at any point in time if you so desire to also control the glucose. 11:40 Remember, you want to monitor your glucose at all times when you’re giving insulin… an IV resuscitation is important and dextrose becomes an important component. 11:49 When you start finding your glucose levels dropping below 200, but that is not how the patient is presenting initially. 11:55 Is that clear? Your patient is presenting initially with ridiculously high levels of glucose. 12:02 “So, Dr. Raj, what’s causing the decrease of glucose?” Oh yes, IV fluid is being given along with insulin, obviously that insulin is going to decrease that glucose rapidly. 12:14 In certain patients, you definitely want to be careful; close monitoring of not only their glucose but then also electrolytes… do not forget that. 12:24 What does insulin do with potassium? It takes it up into the cell, it technically stimulates the sodium-potassium ATPase pump and with that pump, you’re going to pump the potassium into the cell, your patient is now rendered hypokalemic and that is really dangerous for the heart, isn’t it? Because now you’re causing hyperpolarization of the resting membrane potential… not good. 12:49 In addition, also pay attention magnesium and phosphate. 12:53 Magnesium… remember, if your magnesium levels start dropping, that is not good either. 12:58 Your patient is now predisposed to seizures and perhaps even long QT syndrome; once again, heart issues. 13:06 Subcutaneous insulin administration before discontinuing insulin infusion completely. 13:11 Always make sure that you’re able to properly wean your patient off.
About the Lecture
The lecture Diabetic Ketoacidosis (DKA) – Diabetes Complications by Carlo Raj, MD is from the course Pancreatic Disease and Diabetes.
Included Quiz Questions
What is increased in diabetic ketoacidosis?
- Acetoacetic acid
- Glycerol
- Potassium
- Amino acids
- Glutamic acid
What is NOT a response to low insulin levels?
- Decreased lipolysis
- Increased ketones
- Increased glycogenolysis
- Increased protein catabolism
- Increased gluconeogenesis
What is NOT a reaction to decreased intracellular glucose?
- Increased glycolysis
- Increased glucagon
- Increased glycogenolysis
- Increased protein degradation
- Increased lipolysis
What acid-base disorder occurs in a patient with diabetic ketoacidosis?
- Anion gap metabolic acidosis
- Anion gap respiratory acidosis
- Non-anion gap metabolic acidosis
- Metabolic alkalosis
- Non-anion gap respiratory acidosis
What is NOT expected in patients with diabetic ketoacidosis?
- Weight gain
- Polyuria
- Polydipsia
- Abdominal pain
- Fruity breath
A patient in DKA is administered insulin. Suddenly, the patient experiences a tachyarrhythmia. What is the most likely cause of this abnormality?
- Hypokalemia
- Hypoglycemia
- Hypomagnesemia
- Hypophosphatemia
- Hypovolemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
simple and informative and I really like the way he uses his voice to keep us on point with him
I like it very much,before I was confused about this topic but now I can say that I am 100% clear