Playlist
Show Playlist
Hide Playlist
Isotonic, Hypotonic and Hypertonic Disorders
-
Slides Dehydration IntegratedRenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
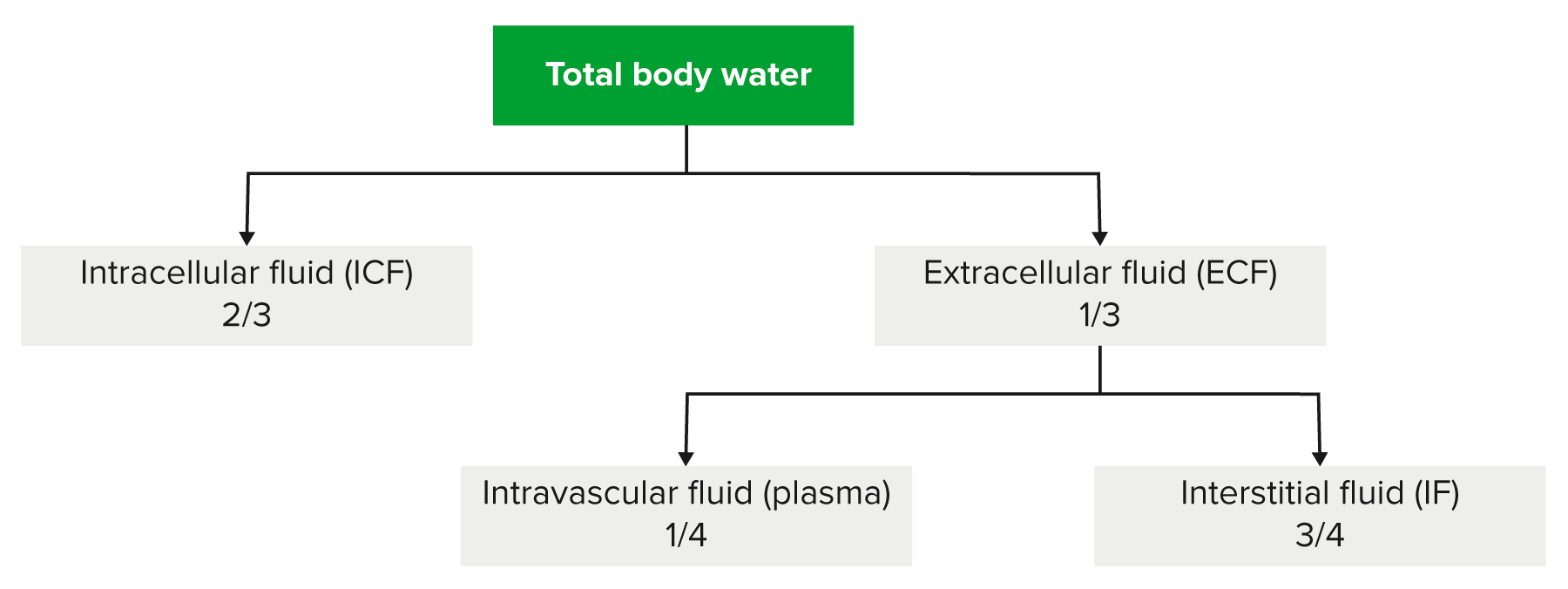
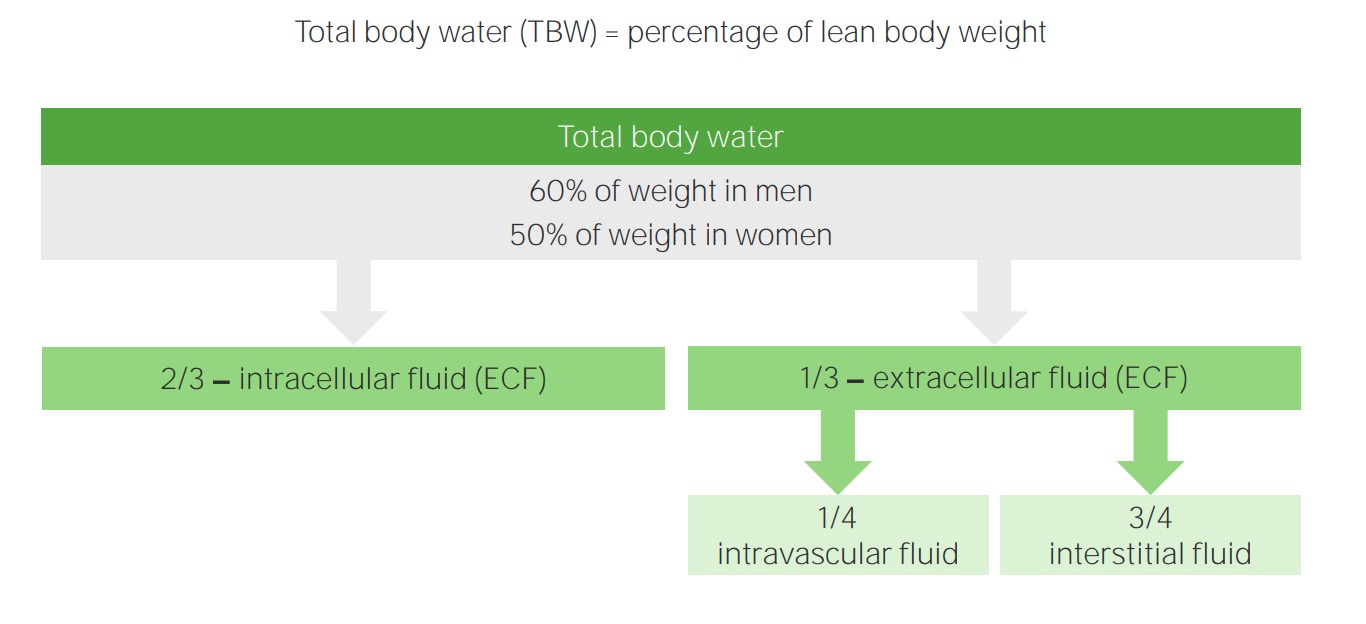
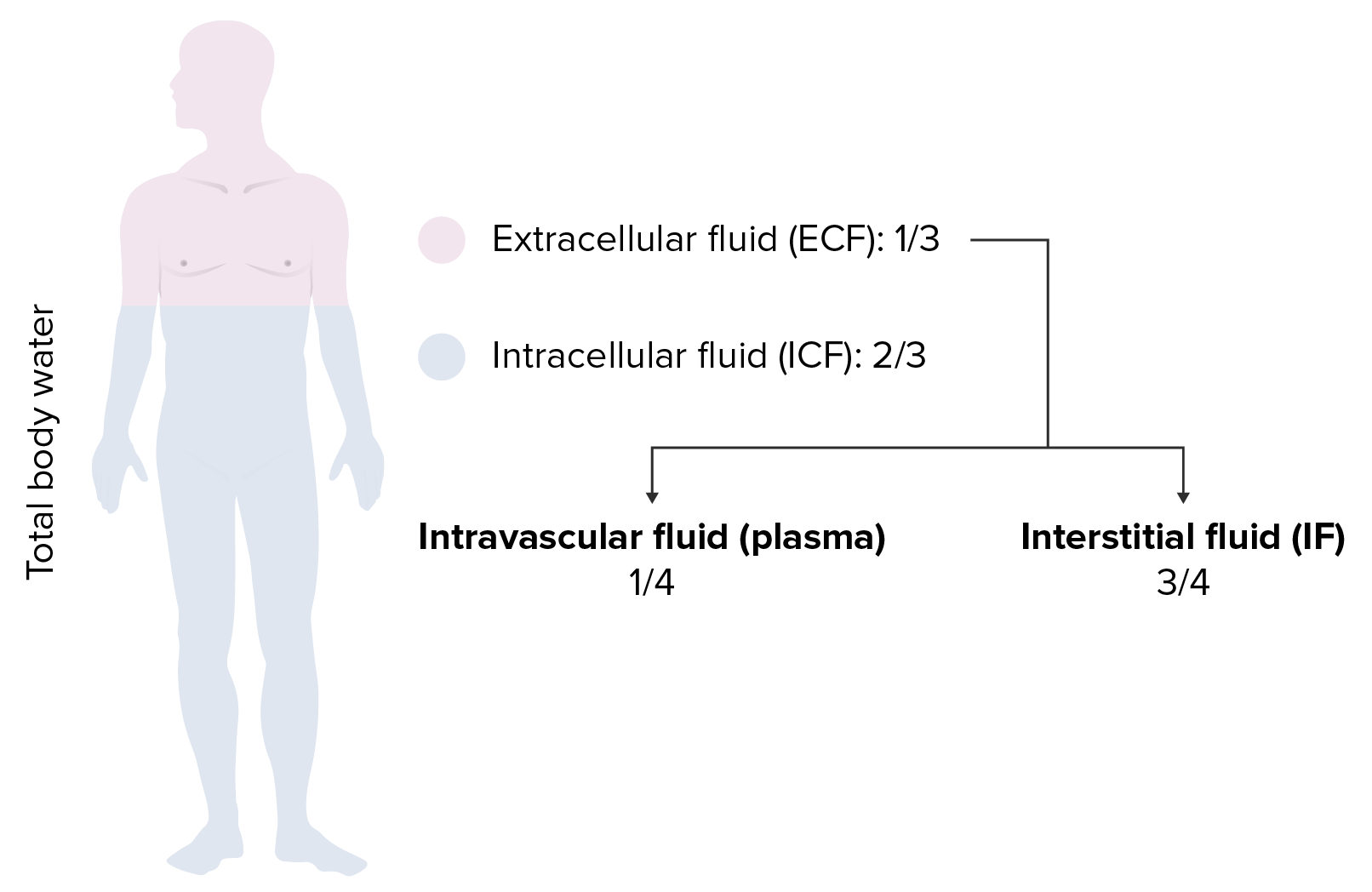
00:01 In this lecture series, we’ll build upon the previous discussion that we laid down firmly about water and sodium pathophysiology. It is imperative that you fully have understood everything that we talked about in the previous discussion before moving onto greater details of isotonic, hypotonic, hypertonic fluid disorders. Understand please that we would be moving through this material rather efficiently. If your foundation isn't strong, you will be confused and you don’t want that. We’re here to clarify things and make sure that your thoughts are organized. Our topic, once again, we'll walk through general definitions of what you're looking for with plasma osmolarity. Up until now, we’ve talked about sodium. We said that it was the main factor to determine plasma osmolarity. 00:52 We also said that as far as normal physiologic effective osmolarity in the clinical realm, it is two times sodium that you’re paying attention to. Now, let’s move into a little bit more details. 01:05 Serum sodium concentration actually reflects a ratio. This ratio is going to be total body sodium, stop there, over total body water. This is what we have. So, serum sodium is equal to total body sodium over total body water. I need you to take a minute and digest this formula because this is then going to determine, as I said, what kind of plasma osmolarity enshifts a fluid that we have between ECF and ICF. Now, total body sodium is the sum of all sodium ware in the ECF. Once again, let me give you the significance of that. 01:49 In the ECF, what do we have, two major compartments. We have the plasma and we have our interstitium, correct? Those two compartments are then divided by what membrane, the capillary membrane. Is that capillary membrane permeable to sodium? Absolutely. So therefore, when we say total body sodium, we're referring to the sodium in both compartments of vascular and interstitium. That must be understood before we move on. 02:16 The serum sodium is the amount of sodium in a liter of serum over the plasma in the vascular compartment. Both compartments are taken into consideration. 02:27 Now, before we move into the discussions of isotonic, hypotonic, and hypertonic disorders, we’ll take a look at overall, what this patient looks like with total body sodium and its assessment. 02:40 Let’s evaluate our total body sodium, shall we? Decreased total body sodium produces signs of volume depletion. So for whatever reason, if you find that the sodium is decreased in one or both compartments, what kind of things can we expect overall? Dry mucous membranes. What about the skin? What does it mean to have tenting of the skin when you pull on it? It means that you pull on it and the skin actually remains as a tent. 03:09 This means decreased skin turgor. Obviously, you won't find it in me. 03:15 Hopefully, you don't find it in you right now because your volume is just fine. 03:20 There is going to be a drop in blood pressure. Stop. Some important physiology here. 03:25 When you have a drop in blood pressure due to hypovolemia shall we say, then you have what, in terms of stretch of your blood vessels? Decreased stretch. When you have a decreased stretch, of your blood vessels, now you tell if there's a drop in blood pressure, what should come out of your autonomic nervous system? The sympathetic, correct? So, you've learned in physiology that through your sympathetic, especially the carotid sinus which houses your glossopharyngeal is going to communicate with the medulla and out comes my sympathetic. Okay. This sympathetic has an effect on the heart. 04:00 Highlight in your head the term here that we're seeing as being reflex tachy. 04:05 How important is that? Quite, there are conditions in pharmacology, or should I say, there are methods in which in pharmacology we manage this reflex tachy by giving perhaps a beta blocker. Correct? So, keep this in mind. Next, when sitting up from a supine position, I was just giving you an example of a maneuver in which your blood pressure might drop. When it does so, then you're looking at reflex tachy as being a possible issue. Evaluation further, now we'll go to the opposite end of the spectrum. 04:39 Meaning to say that in the previous discussion, decreased total body sodium, here we'll have increased total body sodium. Examples: effusion, ascites, and pitting edema. 04:51 Dependent pitting edema, well, if you accumulate too much excess sodium in your interstitium. 04:57 For example, right-sided heart failure, you press upon this, can you pit this? Yes, it is. 05:04 And you find due to low protein that this is going to be transudate specifically. 05:09 Now, the fluid obeys a law of gravity. What does that mean? It then moves to the dependent areas of the body. So for example, it would be either the ankles when you’re standing, or when you’re on supine position, maybe perhaps your flanks, your back. 05:24 Starling’s pressures are altered to produce pitting edema and body effusion. 05:28 By that we mean, well, for example, if it is right-sided heart failure, things we’ve discussed many a time, you're going to then push that fluid out into interstitium. 05:37 An increase in total body sodium increases plasma hydrostatic pressure. 05:42 That's exactly what happens in right-sided heart failure. Due to an increase in plasma volume, you're pushing that fluid where, into the interstitium. Now, an important point. 05:53 An increase in total body sodium increases the weight of the patient. In fact, it is the most common cause of increased weight in a patient who is in a hospital. Now, further evaluation, take a look at the pictures here. If it’s a dry mucous membrane, would you then tell me as to how can you predict or what can you predict in terms of evaluation of total body sodium, dry mucous membranes. This would be a decrease in total body sodium versus what you're seeing in the second picture on your right and that would be pitting edema. Meaning to say that you, as a clinician, have placed your finger on this interstitium or the skin, underneath it being the interstitium and it has pitted. This obviously then represents an increase in total body sodium. 06:46 Fluid movement across the capillary or venule into the interstitial space is driven by the Starling's force. 06:53 Everything we've talked about is in verbiage here. So, we'll walk through this quickly. 06:58 The net direction of fluid movement depends on the Starling’s pressure that is dominant. 07:03 So for example, decreased oncotic pressure, fluid moves out, an increase in hydrostatic pressure, fluid moves out, doesn't it? That’s exactly what we see here. Point one in this paragraph. 07:13 An increase in plasma hydrostatic pressure or you have a decrease in plasma oncotic pressure, meaning to say maybe cirrhosis, improper or lack of albumin synthesis causes the fluid to diffuse where it please from the plasma into the interstitium. Let me ask you a simple question, a discussion that we’ve had but now, we’re going to put this into play. 07:39 What is your effective circulating volume versus your extracellular fluid volume in a patient that has either decreased oncotic pressure or increased hydrostatic pressure? You'll have a decrease in effective circulating volume. Why? Because the fluid is escaping from your vasculature into the interstitium. So, effective circulating volume has decreased. 08:02 Remember the discussion, versus your extracellular fluid volume will be increased overall.
About the Lecture
The lecture Isotonic, Hypotonic and Hypertonic Disorders by Carlo Raj, MD is from the course Fluid and Electrolyte Balance.
Included Quiz Questions
Which of the following is NOT equivalent to serum Na⁺?
- The amount of Na⁺ in the vascular compartment divided by total body water
- The amount of Na⁺ in a liter of serum/plasma in the vascular compartment
- None are equivalent
- All are equivalent
- Total body sodium divided by total body water
Which of the following signs or symptoms is NOT associated with a decrease in total body sodium?
- Decreased heart rate
- Decreased skin turgor
- Positive tilt table test
- Decreased blood pressure
- Dry mucous membranes
What is the most common cause of weight gain in a hospitalized patient with pitting edema?
- Increased total body sodium content
- Increased levels of nutrition
- Increased free water excretion
- Increased sodium excretion
- Increased albumin production
In a patient who is hospitalized with pitting edema due to increased total body sodium, which of the following statements is TRUE?
- Sodium moves across capillary membranes into the interstitial fluid
- Intracellular fluid volume increases
- There is a decrease in plasma volume
- There is a decrease in hydrostatic pressure in the capillary
Which of the following symptoms is associated with a decrease in total body sodium?
- Skin tenting when the skin is pinched
- Negative tilt test
- Reflex bradycardia
- Wet mucous membranes
- Hypertension
Which of the following is associated with an increase in total body sodium?
- Increased plasma hydrostatic pressure
- Decreased plasma hydrostatic pressure
- Decreased weight of the patient
- Non-pitting edema
- Decreased plasma volume
Which of the following is a mechanism of pitting edema?
- Excess of sodium-containing fluid in the interstitial space
- Excess of protein content in edema fluid
- Lack of sodium-containing fluid in the interstitial space
- Increased sodium excretion
- Excess of sodium-containing fluid in the intracellular space
Which of the following is a mechanism of fluid movement out of capillaries into the interstitial space?
- Increased plasma hydrostatic pressure
- Increased plasma oncotic pressure
- Decreased plasma hydrostatic pressure
- Decreased total body sodium
- Increased albumin production
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |