Playlist
Show Playlist
Hide Playlist
Dehydration: Isotonic Fluid Disorders
-
Slides Dehydration IntegratedRenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
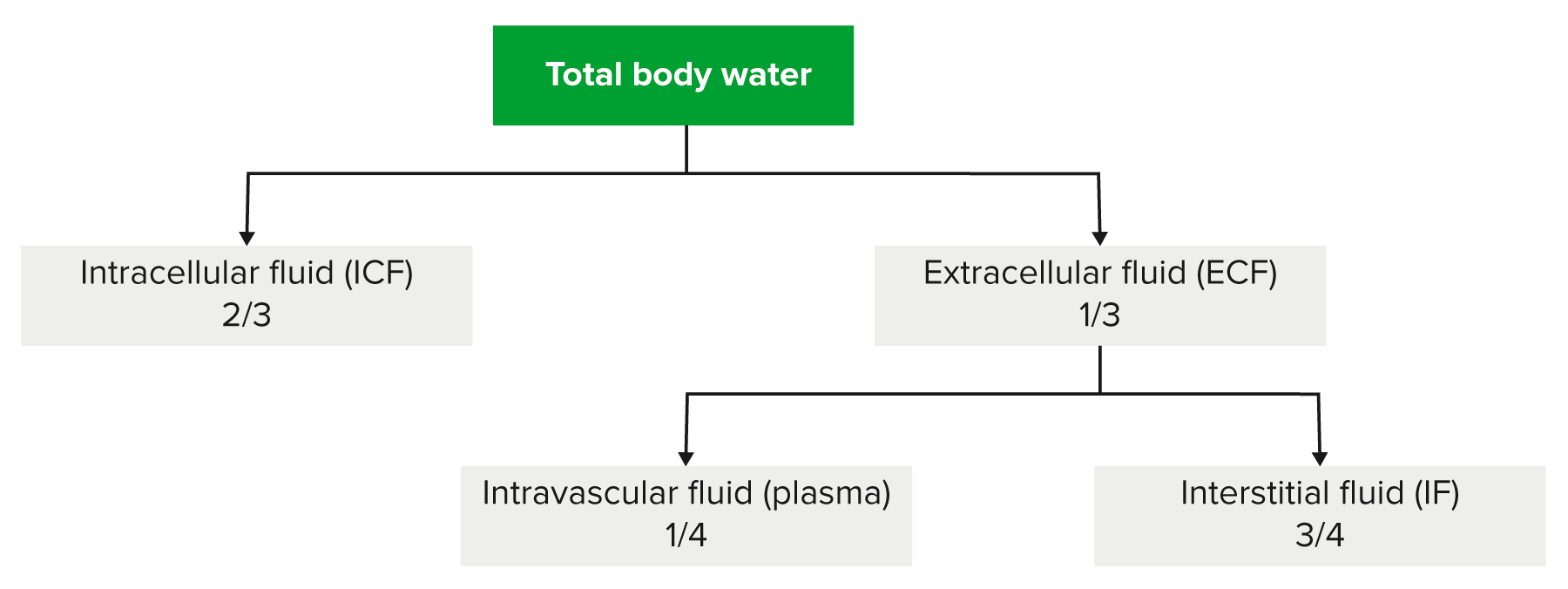
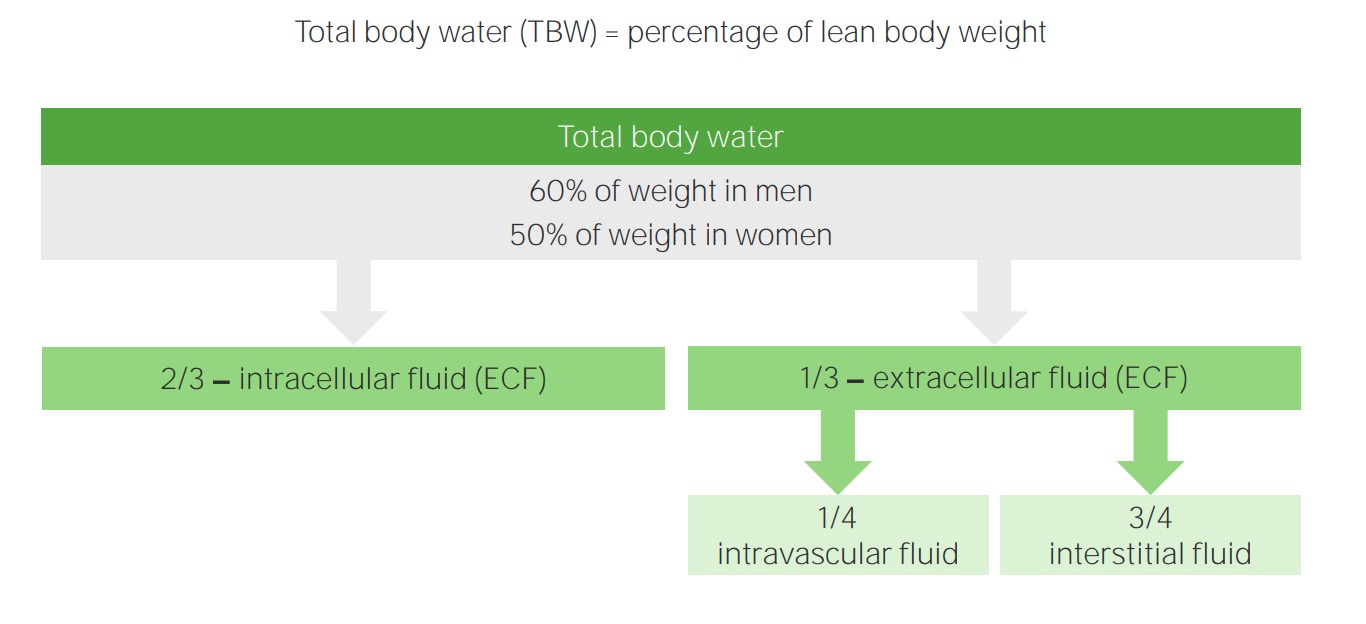
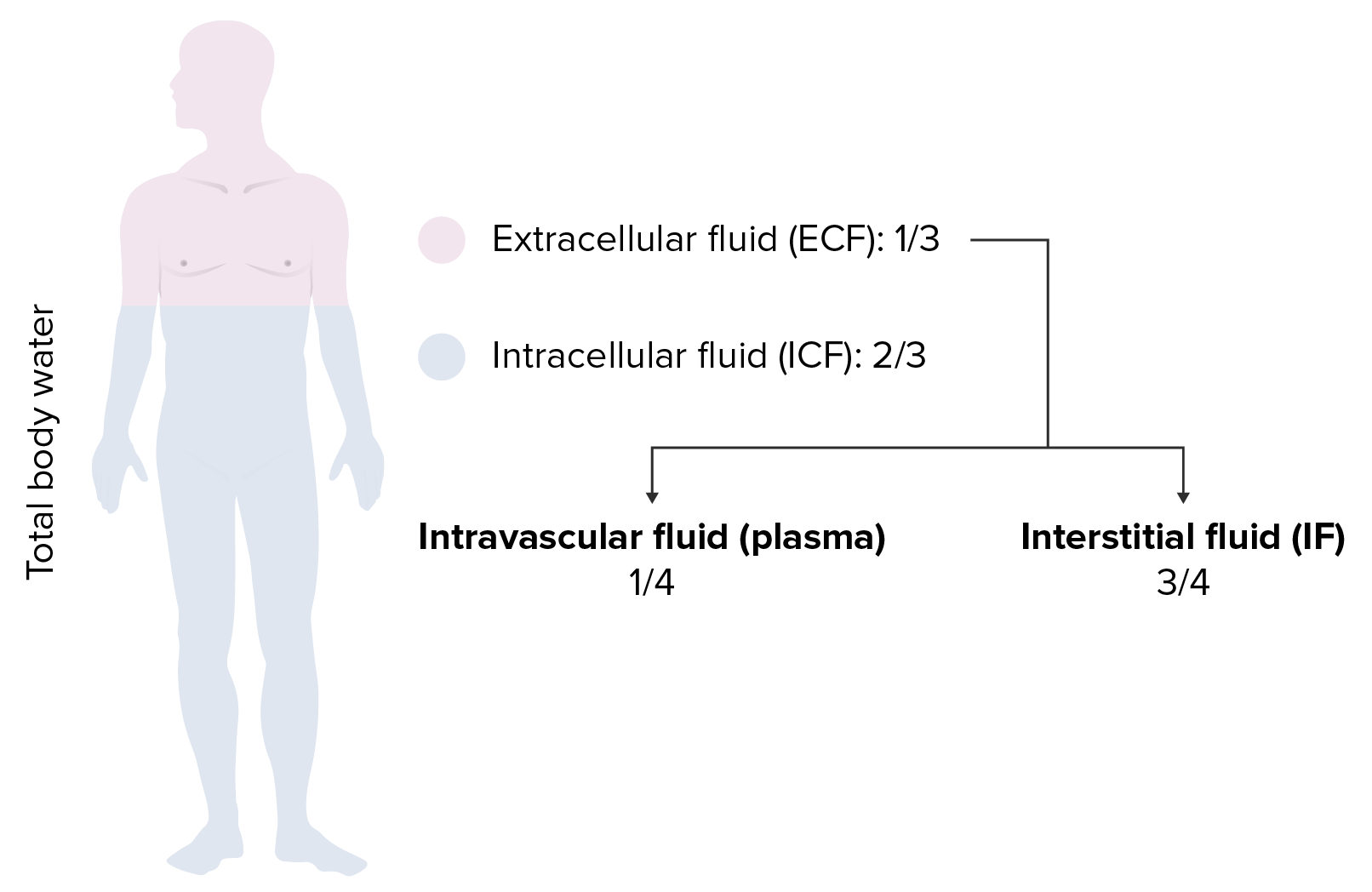
00:01 Let’s talk about isotonic now. First and foremost, in the previous lecture series where we laid down the foundation of our Darrow Yannet box and the shifting of the ICF and ECF, we looked at diarrhea, and diarrhea, adult diarrhea specifically. There is going to be massive loss of volume. 00:23 What volume are you going to always referring first, the ECF volume. That's the volume that you will refer to first. That ECF volume has then decreased in an isotonic fashion. 00:36 Is anything else affected? Not at all. Isotonic net loss of sodium, take a look at this. 00:44 There’s an equal decrease in total body sodium and total body water. So therefore, is there going to be any change in plasma osmolarity? None whatsoever, plasma osmolarity in serum sodium are normal, a proportionate decrease. The only thing that you’re seeing in adult diarrhea is going to be an ECF volume in an isotonic fashion. Now, as we go through this, the arrows, what are these arrows that we’re referring to? You see the ratio of total body sodium and total body water? Those arrows then represent the magnitude of change that we’re going to see. 01:23 The magnitude of that ratio, you see it. The magnitude of that ratio is equal in both total body sodium, total body water. Plasma osmolarity remains the same. There is no osmotic gradient, so there’s going to be no shift. ECF volume contracts and that is it. What does that mean? A decrease in ECF volume. Any change in ECF osmolarity? No. Any change in ICF? Take a look, everything remains the same. However, there are signs of volume depletion. 01:57 What are those signs please? Good, decreased skin turgor, maybe dry mucous membrane. 02:03 Are we clear? Examples include adult diarrhea or perhaps loss of whole blood due to hemorrhage. 02:11 Isotonic gain of fluid, once again, we’re going to walk through this one quicker because now, we lay down the foundation. So, say that you’re giving your patient IV fluids such as saline. 02:23 Normal saline is 0.9%, right? That is isotonic. That must be understood clinically, not 1.0. 02:32 0.9% is normal saline. Okay, if you infused your patient with isotonic saline, maybe perhaps excessively, there's going to be, take a look at the arrows, increase, magnitude will be the same. 02:47 So therefore, the only thing that you do is increase ECF volume but there is no change in plasma osmolarity. Everything is normal. Next, there is no osmotic gradient. You're not going to have any shifting between ECF and ICF but you will have ECF volume expansion and that’s it. 03:04 But the ICF, take a look, remains normal. Pitting edema and body cavity effusion may be present because you'll have this fluid where, increasing ECF. Let me ask you a question now. Now be careful. 03:20 So, this IV fluid that you're putting into your patient, what are you expanding? The ECF. 03:26 Would you tell me the name of the membrane that is specifically in the ECF only? Is that the capillary membrane or is it the cell membrane, in the ECF? That is your capillary membrane, right? That capillary membrane, is it permeable to sodium, yes or no? Yes. 03:46 So, when you infuse saline, is it possible that that fluid might end up in the interstitium? Of course, it can. So, could it be transudate and pitting? Yes, it can. Are you seeing this now? You must understand the fundamentals so that you clearly see your patient and you’re not confused by the distractions and all the – sometimes we call this medical distractions or decorations or whatnot. 04:16 You focus on what you need to so you can come to your patient's diagnosis effectively. 04:20 Example, excessive infusion of isotonic saline. 04:23 Let’s talk about normal saline. It is 0.9%. That must be understood. It is infused in patients to maintain blood pressure but if you put it in, what then happens? You're filling up the plasma compartment and you're also filling up the interstitium. Why do we give it? If we know the plasma compartment is the most important compartment to maintain then why are we giving IV fluid such as normal saline? Why don't we inject our patient with albumin and company? Why not just fresh frozen plasma? Because it’s cheap, and it works, and it helps restore the blood pressure. As expected, some of that normal saline, if you missed it, here it is. It enters the interstitium. What is the interstitium outside of the plasma compartment? What’s the name of the membrane? Good, that is your capillary membrane. 05:17 So therefore, it can enter but understand, you'll have enough fluid in the plasma compartment to raise your blood pressure. Other solutions that are used that are more expensive include Ringer's lactate and 5% albumin. Here you go. Remember, as a clinician, you are also responsible for maintaining cost in the hospital. You’d thought that the information and such but the volume is a lot, you're also responsible for cost in the hospital. You're responsible for keeping it low. That must be understood for every single board exam. 05:52 Ringer’s lactate and albumin would effectively only increase the vascular compartment but it’s expensive. It’s expensive.
About the Lecture
The lecture Dehydration: Isotonic Fluid Disorders by Carlo Raj, MD is from the course Fluid and Electrolyte Balance.
Included Quiz Questions
Which of the following is a similarity between isotonic loss of fluid and isotonic gain of fluid?
- No change in osmotic gradient
- Pitting edema
- Plasma osmolality changes
- Intracellular fluid volume changes
- Decrease in blood pressure
Which of the following is a potential replacement for 0.9% normal saline in the setting of an isolated contraction of the extracellular fluid compartment?
- 5% albumin
- Mannitol
- Dextrose 2.5% water
- 3% normal saline
- 0.45% normal saline
Which of the following is NOT associated with an isotonic loss of fluid?
- Cellular swelling
- Adult diarrhea
- No change in serum sodium concentration
- No change in plasma osmolality
- Hemorrhage
What is responsible for the development of pitting edema in an isotonic gain of fluid?
- The capillary membrane is permeable to sodium and water.
- The cellular membrane is permeable to sodium and water.
- Contraction of extracellular fluid volume.
- The high-protein content of edema fluid
- Shifting of fluid based on osmotic gradient
Which of the following is associated with an isotonic gain of fluid?
- ECF volume expansion
- ICF volume expansion
- Increased serum sodium levels
- Increased plasma osmolarity
- Non-pitting edema
Which of the following is associated with an isotonic loss of fluid?
- Normal ICF volume
- ECF volume expansion
- Decreased serum sodium
- Decreased plasma osmolarity
- Wet mucous membranes
Which of the following solutions stays in both interstitial and vascular compartments?
- Isotonic saline
- Packed red blood cells
- 5% albumin
- Low-molecular-weight dextran
- High-molecular-weight dextran
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |