Playlist
Show Playlist
Hide Playlist
Hypotonic Fluid Disorders
-
Slides Dehydration IntegratedRenalPathology.pdf
-
Reference List Pathology.pdf
-
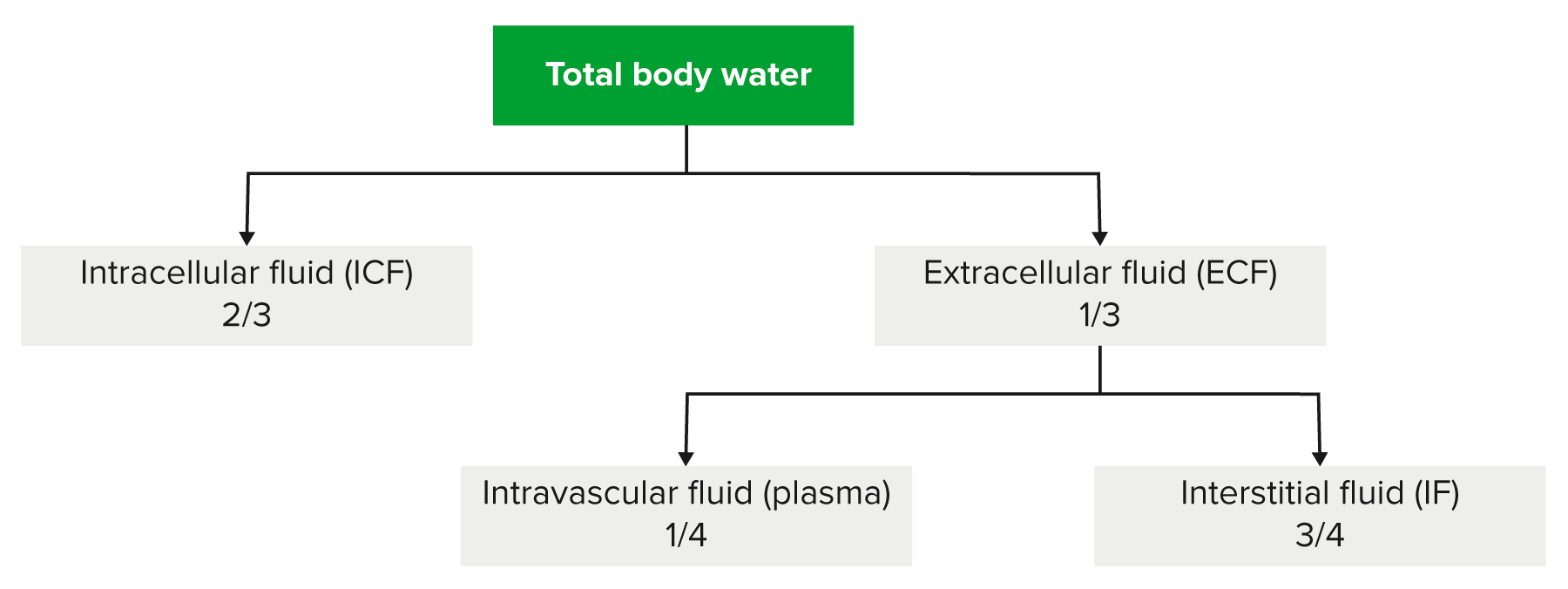
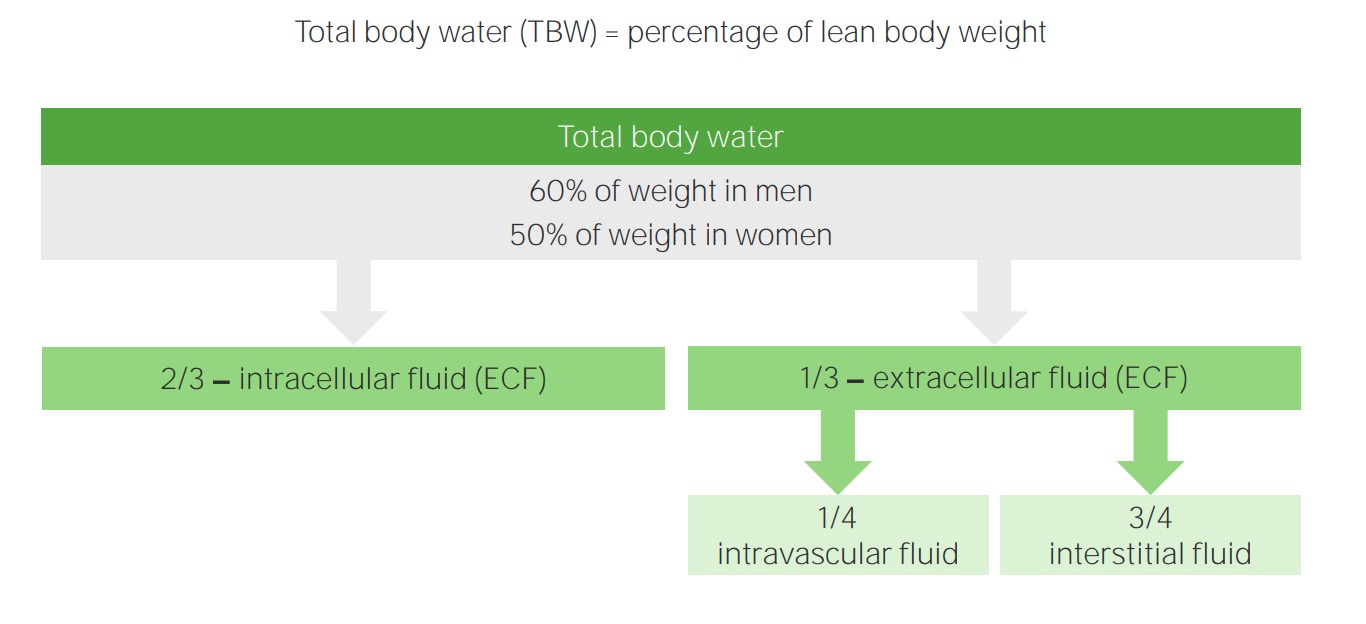
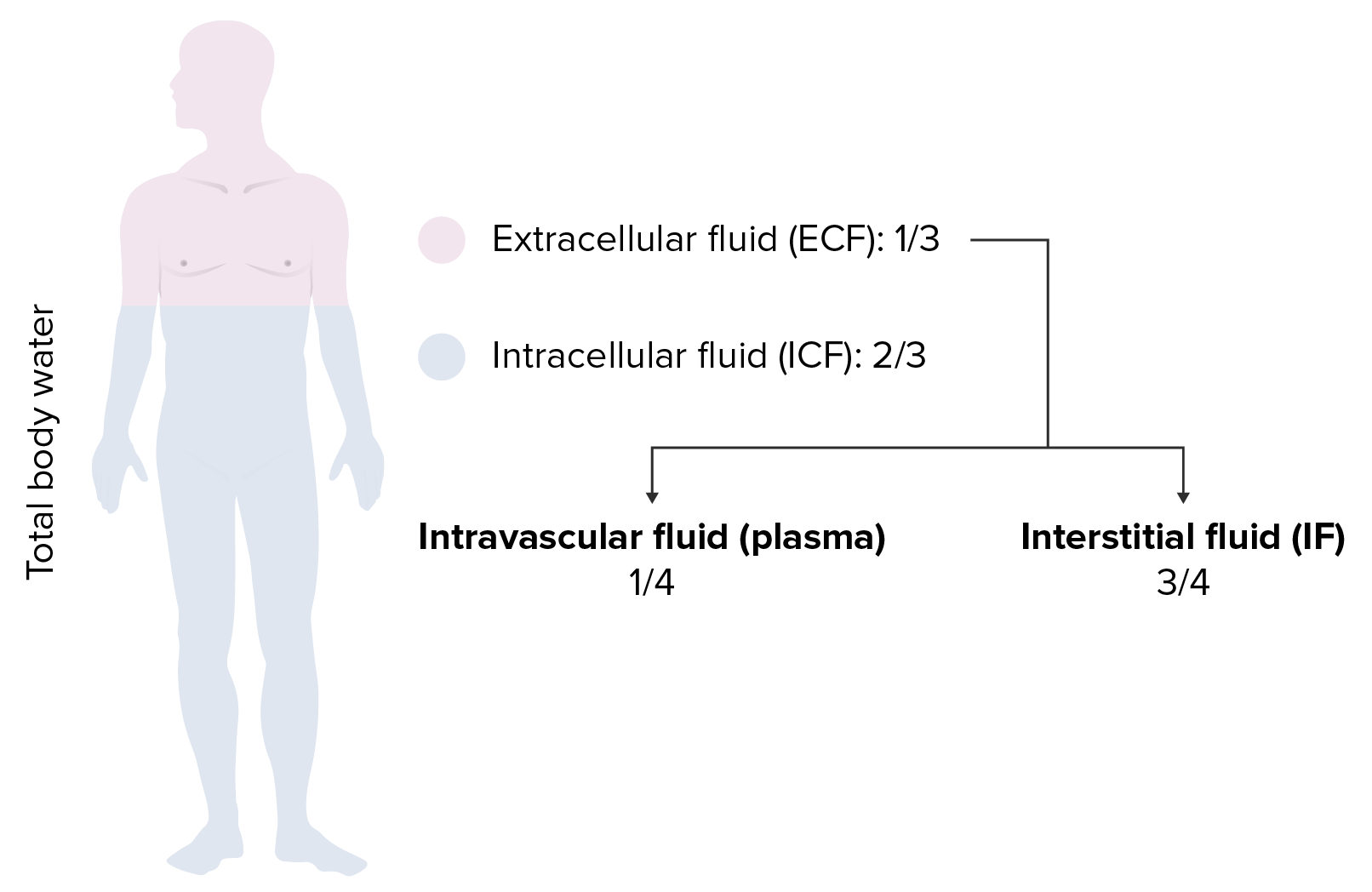
Download Lecture Overview
00:00 Hypotonic fluid disorders is our next discussion. At this point, we have completer discussion of isotonic. 00:07 So, with hypotonic fluid disorders, overall, hyponatremia is always present. 00:14 So, once you have hyponatremia, what are you going to call this patient or what's the issue here? Decreased plasma osmolarity. Are we clear? The osmotic gradient will be present. 00:27 Let me ask you a question. Was there an osmotic gradient with isotonic fluid disorders? Yes or no? With isotonic fluid disorders, was there an osmotic gradient? Nope. Here is the first time that we’re going to take a look at an osmotic gradient between the ICF and ECF. 00:44 So, we're going to find water shifting, close your eyes, predict this. Water is going to shift from the ECF into the ICF. Now, when you say hyponatremia, when you say hypotonic fluid disorders, what compartment are we dealing with as being hypotonic,only the ECF. I always told you that. 01:04 Always begin with the plasma compartment. That's what you're paying attention to. 01:09 So, if the plasma compartment is hypotonic and you have decreased plasma osmolarity, then where is there more solute? Where is there more solute? In the ICF. 01:18 So therefore, fluid is going to do what? Enter the ICF. That’s what happens to ICF volume. 01:23 It will expand. Most likely, what will happen to ICF osmolarity? It will decrease. 01:29 How can I do this so quickly? I told you about these four steps over and over again, ECF volume, ECF osmolarity, ICF volume, ICF osmolarity, four steps, always. 01:39 There's no magic bullet here. It’s about understanding, repeating, repeating, repeating, repeating this information. So, hypotonic, what do we have. Well, there might be, now listen, hypertonic loss of sodium. So what does that mean? Remember that example that I gave you where literally you're flushing down your sodium through the toilet? that's what this is. So, if you're flushing sodium down the toilet, please tell me what your plasma osmolarity is. Good, decreased. What's my topic? Hypotonic fluid disorders. 02:15 Next, now we're going to find changes in magnitude of our arrows. So, what are you losing a lot more of? Take a look at the ratio here. Total body sodium has two arrows, which means that you're losing greater amounts of sodium than you are of water. In the denominator, you only have one arrow. 02:37 So, what are you losing more of? Sodium. Are you also losing fluid? Yes, you are. 02:43 If you’re losing more sodium than water, what happens to that ratio? Decreases. What is this ratio? What is it determining? Plasma osmolarity. Aah, are we seeing it now? So, if that ratio is decreased, take a look please. Next comment, plasma osmolarity is decreased, simple. What about ECF volume? It contracts. Why? Because total body water is decreased. Now, as the total body water decreases, ECF volume decreases, what happens to plasma osmolarity? It decreased, plasma osmolarity decreased. 03:20 So, where is that water shifting into? The ICF. Are you seeing this? Literally, water is passing through the cell membrane, ICF volume expands. So now what do we have? We have signs of volume depletion are present. We have mucous membrane that are dry and you have skin tenting, right, decreased skin turgor. Examples, okay now, before we take a look at this, would you please predict what kind of pathologies? You miss some pathologies where you're losing sodium in excess. Would it be Conn's syndrome or would it be Addison's disease? Good, it would be Addison's disease. What kind of congenital adrenal hyperplasia would give you loss of your sodium? 90% of all congenital adrenal hyperplasia is this enzyme deficiency. 04:14 So, when we do and when you've done all congenital adrenal hyperplasia, you’ve heard of 21-beta-hydroxylase deficiency, you’ve heard of 11-beta-hydroxylase deficiency, 17-beta-hydroxylase deficiency, 17-beta-hydroxysteroid dehydrogenase deficiency. 04:27 You know all these, right, or at least you've heard of them. Of all of them, the one that you pay attention to majority of the cases will be 21. So in 21 guess what? You cannot form DOC, deoxycorticosterone, nor can you form aldosterone. Wow! There's no mineralocorticoid in your body. 04:47 Go back to the very first statement here and what's the most important thing that we're losing in excess, the sodium in excess. If there's no mineralocorticoid, you're going to be losing lots of salt. So therefore, everything that we just talked about on this slide is going to be present in your patient. Move on. Gain of pure water, a second example of hypotonic fluid disorder. You have pure gain of water, only there's nothing here about salt. 05:16 Take a look at the ratio here. You're increasing, increasing, increasing the denominator like crazy. 05:21 Close your eyes. Just you know this math. If you increase the denominator, what happens to the ratio? It decreases. What does this ratio then represent? Plasma osmolarity. Are we okay here? So, if you increase the denominator, the ratio decreases. Take a look at plasma osmolarity. 05:37 What’s my topic for this entire section? Hypotonic fluid disorder, but this was a different way of developing it, wasn't it? Gain of pure water. Are you ready for this? I’m going to put you through the ringer but you got this. Tell me about the ECF volume when you gain pure water. 05:53 You're drinking, let's say, pure water. Tell me about the ECF volume, increased. 05:57 Tell me about ECF osmolarity. Well, the topic is hypotonic, decrease in plasma osmolarity. 06:03 Next, what happens, ICF volume, you're going to go into the ICF. ICF expansion, what happens to ICF osmolarity? Decreases. There you go. Expansion of ECF and ICF volumes. 06:17 Normal skin turgor. That's important for you to understand. So here, you’re gaining pure water but you have a decrease in plasma osmolarity. Understand that you will not have hypovolemia. 06:29 Examples, SIADH, or the example that I just gave you was drinking excess water, compulsive water drinking. What might be your diagnosis in that patient? Who is this who's drinking too much water? It's called primary palliatives here. 06:46 Maybe your patient is schizophrenic, a little crazy. That's your psychogenic palliatives here. 06:52 You get what I'm saying here. With SIADH, small cell lung cancer, paraneoplastic perhaps. 06:59 Move on. Here, still continue to a condition or our issue with hypotonic fluid disorder. 07:05 But this is hypotonic gain of sodium. Now, this is a little tricky. Hence, you really want to make sure that you know what total sodium means. What does serum sodium mean? Close your eyes. 07:17 It means total body sodium over total body water. This is going to determine what plasma osmolarity. 07:23 So, let's say that you're in the 6th hour or 7th hour of an exam room. All day, it's just been a marathon. 07:30 Your brain just drained. You're expecting me to think? At some point, why not use a little bit of math as a crutch to help you? By that, I mean the following: Let’s say that you have a gain in both sodium and total body water. Well then, you think to yourself, "Well, what gained more?" In this case, there was total body water that was gained more than your total body sodium. 07:55 So, the denominator has increased more so. What then happens to the ratio? Decreases. 08:02 I’m sorry. What does this ratio mean? It determines plasma osmolarity. So, if the ratio decreases, thus, your plasma osmolarity. Are we clear? Good. Now, the examples, this is completely different from gaining pure water. Go back. Take a look at gaining pure water. In gaining pure water, what did you only affect? Your only affected total body water, period. Thus, the ratio decreased. 08:27 Here, what's my difference? Yes, you increased total body water but you also increased total body sodium. What the heck kind of conditions are these, Dr. Raj? What are my differentials? Watch and learn. We have expansion of ECF and ICF volumes. Why? Because your plasma osmolarity decreased, water shifted into your ICF. It caused pitting edema. I’m seeing it now. 08:52 Pitting edema, okay, so it must be issues such as right-sided heart failure. Oh, it must be issues such as decreased oncotic pressure. How is this occurring as cirrhosis, no synthesis of albumin? What about nephrotic syndrome? How much protein are you losing, greater than 3 ½ grams? Significant pitting edema. Now, the states of pitting edema, cardiac output is decreased, just to make sure we’re clear here, causes release of catecholamines. Why? Why? Don't memorize this. 09:26 So, you have decreased cardiac output, states of pitting edema, where is my fluid? In the interstitium. 09:31 What about the plasma compartment? Effective circulating volume is decreased. 09:37 So now, the body thinks, whew, I need to, need to, need to increase my catecholamines such as your epinephrine, norepinephrine. In addition, what about down in the kidney? Fluid is escaping from the vasculature. I want you to go into afferent arteriole, you're going to release renin. Here comes my RAAS. Next, you’re going to stimulate ADH release because the body doesn’t know any better. So therefore, kidney reabsorbs slightly hypotonic sodium-containing fluid. That's the issue here. So the kidney reabsorbs slightly hypotonic but it’s sodium-containing fluid so overall, you’re then going to have a decrease in plasma osmolarity. 10:22 Next, alteration in Starling's pressure redirects the sodium-containing fluid into the interstitium, hence, the pitting edema. We talked about this plenty. Then finally, what's your underlying issue? How do you correct all of this if you're dealing with heart issue? Please make sure that you manage the heart and that cardiac output is now restored. That’s the only way that you can correct this because apart from that, the body doesn't know any better. 10:52 So we have hypotonic fluid disorder. This is probably one of the trickier ones in which you are gaining well, hypotonic sodium increase. More so, total body water but sodium is also involved, hence, pitting edema. Now, correction of hyponatremia, what do you want to do here? As I told you earlier, if there is going to be something like your IV fluids and you gave it too quickly, then what's been circled here is the fact that in the pons, you see that area which is kind of dark there, that darkness represents the fact that there is a demyelinating disorder when given IV fluid too quickly. This is called and what's in bold here is central pontine myelinolysis. As a general rule, take a look at the middle of this paragraph here, give slowly over the first 24 hours, period. 11:50 If you give it too quickly, you're worried about a demyelinating disorder. 11:53 In terms of pathogenesis, a number of theories out there, we're not going to spend time on that.
About the Lecture
The lecture Hypotonic Fluid Disorders by Carlo Raj, MD is from the course Fluid and Electrolyte Balance.
Included Quiz Questions
Which of the following is ALWAYS true as a result of any hypotonic fluid disorders?
- Intracellular fluid volume expansion
- Extracellular fluid volume expansion
- Decrease in oncotic pressure in the capillary
- Increase in hydrostatic pressure in the capillary
- Extracellular cellular fluid osmolality increase
Which of the following is LEAST likely to cause hyponatremia?
- Diarrhea
- Addison’s
- Cirrhosis
- Psychogenic polydipsia
- SIADH
Which of the following etiologies of hyponatremia is associated with normal skin turgor?
- Psychogenic polydipsia
- Addison’s disease
- Cirrhosis
- Right sided heart failure
- 21-alpha-hydroxylase deficiency
Which of the following causes of hyponatremia is associated with a decrease in extracellular fluid volume?
- 21 alpha hydroxylase deficiency
- Small cell carcinoma of the lung
- Nephrotic syndrome
- Right sided heart failure
- Psychogenic polydipsia
Which of the following changes would you NOT expect to see in a patient with hyponatremia associated with pitting edema?
- Decreased total body water
- Release of catecholamines
- Increased total body sodium
- Stimulation of ADH release
- Decrease in effective circulating volume
What is the potential irreversible consequence of rapid correction of hyponatremia?
- Central pontine myelinolysis
- Pitting edema
- Nephrotic syndrome
- Hypertension
- Cellular swelling
Which of the following medical conditions is an example of a hypertonic loss of sodium?
- Addison's disease
- SIADH
- Nephrotic syndrome
- Right-sided heart failure
- Cirrhosis
Which of the following medical conditions is an example of a gain of pure water?
- SIADH
- Addison's disease
- 21-hydroxylase deficiency
- Cirrhosis
- Right-sided heart failure
Which of the following medical conditions is an example of a hypotonic gain of sodium?
- Cirrhosis
- Adult diarrhea
- SIADH
- Addison's disease
- 21-hydroxylase deficiency
Which of the following is a general rule for the correction of hyponatremia?
- Replacement of sodium-containing fluid slowly over 24 hours
- Replacement of sodium-containing fluid rapidly within 1 hour
- Replacement of sodium-containing fluid slowly within 4 hours
- Replacement of sodium-containing fluid rapidly within 30 minutes
- Replacement of sodium-containing fluid slowly within 6 hours
Which of the following is associated with hypertonic loss of sodium?
- ECF volume contraction
- ECF volume expansion
- ICF volume contraction
- Increased plasma osmolarity
- Wet mucous membranes
Which of the following is associated with the gain of pure water?
- Normal skin turgor
- ICF volume contraction
- ECF volume contraction
- Increased plasma osmolarity
- Increased plasma sodium
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lectures, Dr. Raj! My 8 yr old convinced me to rate before I finished the lecture series.