Playlist
Show Playlist
Hide Playlist
Death and Dying
-
Slides DeathandDying GeriatricCare.pdf
-
Download Lecture Overview
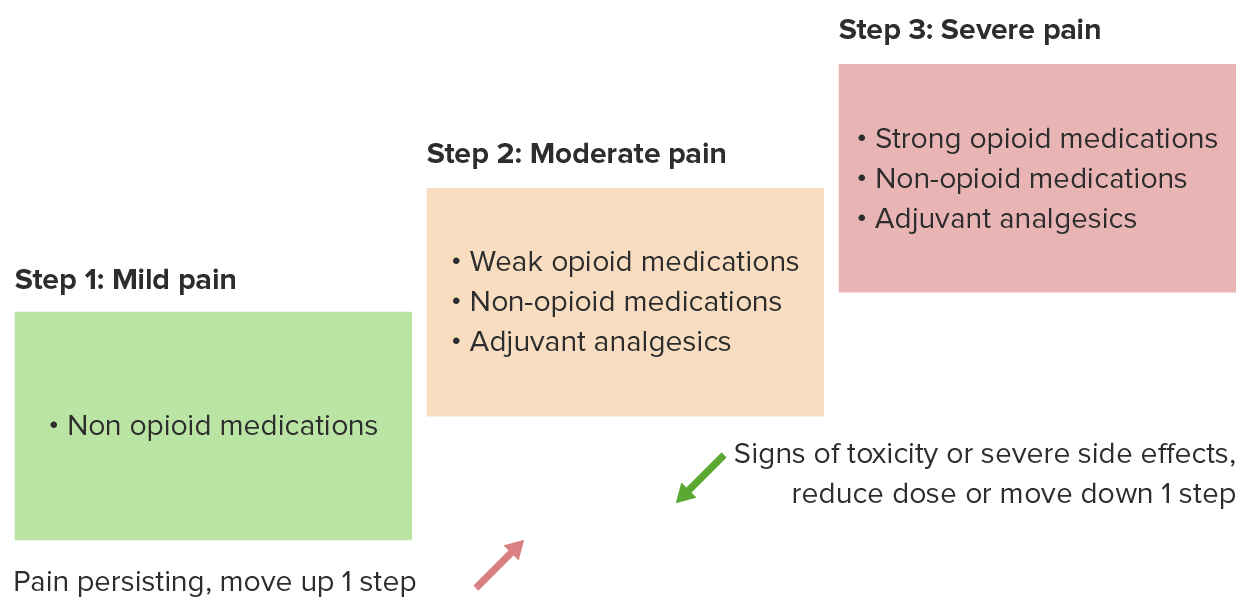
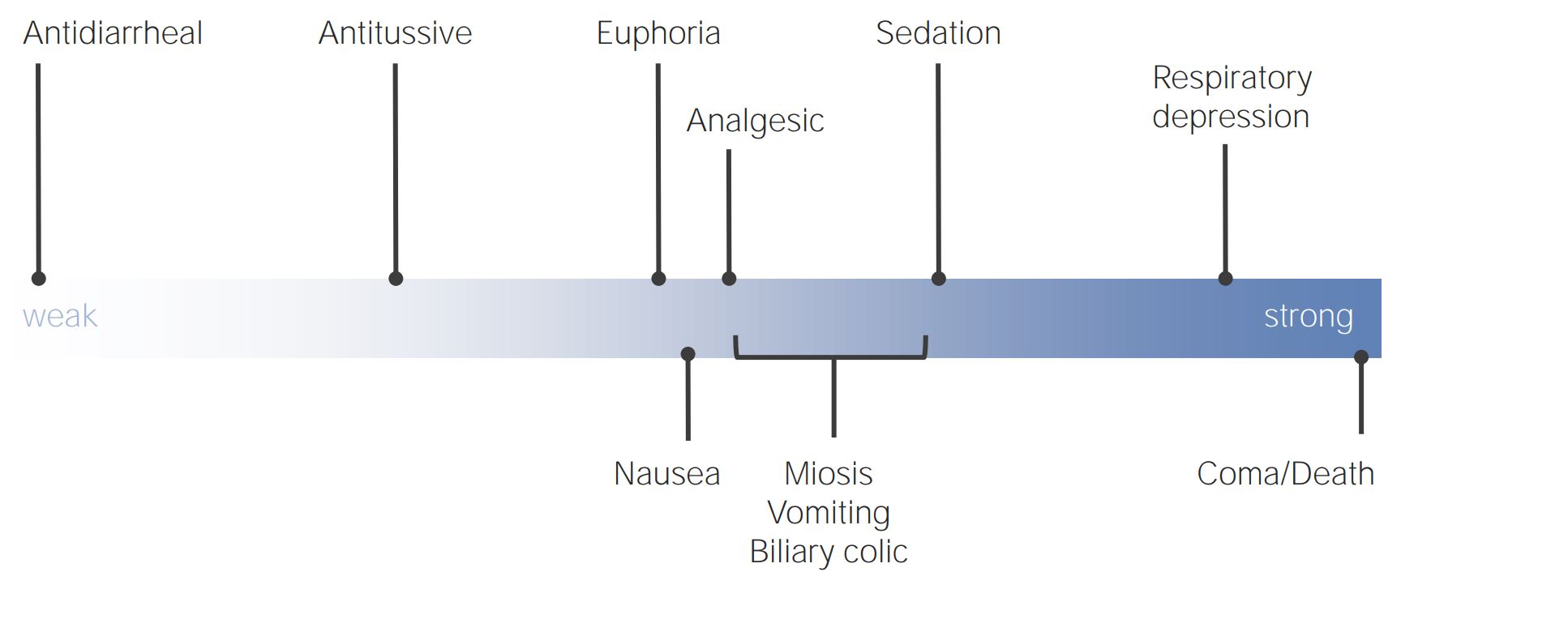
00:01 Now, we're going to cover the difficult subject of death and dying. 00:06 And this is something that a lot of clinicians struggle with, and understandably so. 00:11 It can be a difficult issue. 00:13 Yet, it is critically important that we, as clinicians, are there for our patients during their most difficult moments. 00:19 And so, let’s start with a case and then we’ll move forward from there. 00:23 We have a 93-year-old with increasing pain due to metastatic prostate cancer. 00:28 His other diagnoses include Alzheimer’s disease and heart failure. 00:32 So, what should you consider regarding appropriate analgesia for this patient. 00:37 Is it, A, acetaminophen is the best choice for him; B, the risk of respiratory depression associated with opioids would be unacceptable for him; C, constipation is fairly rare during opioid therapy; or D, opioids are first-line analgesic in this case? What do you think? The answer is D. 00:57 Opioids are first-line analgesic in this case. 01:00 His presumed level of pain due to a severe condition, such as metastatic prostate cancer, along with his end-of-life condition mandate the use of opioids over other therapies. 01:13 And just to say that this is a normal part of the lifecycle, dying. 01:18 There is 100% risk of mortality that each of us carry with us. 01:23 We, as clinicians, really haven't made a dent in that overall risk of dying at some point. 01:28 And therefore, what we really want to focus on is allowing patients to die with dignity and to make them as comfortable as possible and to give the best experience possible to their loved ones as well. 01:43 And that may start with pain management. 01:45 So, you don't want a patient at end-of-life to be suffering a lot, and that involves both pain, but also dyspnea. 01:52 And opioids are effective for both. 01:55 So, that's why they are first-line for pain and dyspnea at the end of life. 02:00 There is a risk for respiratory depression, but when titrated correctly over time, the risk for serious respiratory depression with opioid therapy is quite small. 02:11 And one thing to note is that we will begin patients on a controlled extended-release opioid. 02:18 That's the baseline of therapy, but they should also have breakthrough doses available for breakthrough pain, more severe pain, and that should be about 10% to 20% of the total 24-hour morphine equivalent. 02:31 So, you can calculate what they need in terms of breakthrough medications based on what they're requiring for their 24-hour medications. 02:39 A word about methadone. 02:40 I think it should only be used by very experienced practitioners because it has a long half-life and that accumulation can lead to side effects, such as respiratory depression, unlike other longer-acting types of opioids, such as oxycodone, long-acting morphine or long-acting fentanyl through the transdermal system. 03:04 Methadone is also unique, in that it can promote arrhythmia and overdose, and that’s something that the others don't share. 03:11 Gabapentin also has a role in end-of-life pain, particularly in cases of neuropathic pain. 03:17 And then, for patients with bone pain or skeletal pain, you can consider the use of NSAIDs, bisphosphonates or even corticosteroids to complement the action of opioids. 03:30 So, what about opioid side effects? Constipation is almost universal with these agents. 03:35 So, therefore, I always will prescribe, at the same time I'm prescribing an opioid, particularly for longer-term use beyond a few days, I’m going to prescribe a motility agent, specifically for the gut. 03:48 Senna or bisacodyl can work. 03:52 Failing that, polyethylene glycol is also another agent that’s fairly easy to use and can be effective as well, and I might add that on for patients with more severe constipation related to their opioid use. 04:05 What about nausea? Nausea is something very common that we see among patients at the end of life as well. 04:11 Ondansetron is generally well tolerated and it’s become the drug of choice for nausea. 04:18 But another option may be a drug like haloperidol. 04:21 Watch for sedation with these medications, particularly haloperidol, when they're already receiving opioid therapy, but it can relieve nausea in case when ondansetron isn't enough. 04:32 What about delirium? Confusion at the end of the life is really common. 04:36 It affects most people. 04:38 And nearly half get agitation, which is, you know, difficult for the patient and very difficult for caregivers as well. 04:45 Difficult to see that. 04:47 So, the first thing is, take a hard look at what the patients are taking. 04:51 Are they receiving any anticholinergic therapy or too many sedating drugs? It may be drug side effects. 04:57 And then also look at as to whether they are very constipated or possibly retaining urine. 05:02 All those things may promote delirium. 05:07 For cases of delirium, you can use benzodiazepines, but do recall that benzodiazepines, in combination with opioids, in particular, is associated with a high risk for respiratory depression and serious complications. 05:21 So, use them, but use them parsimoniously. 05:26 For secretions, this is something that patients, and particularly families can feel very disturbing, because patients at the end-of-life don't clear their secretions very well, and therefore, they can have a rattle-y sound to their breath, can be disturbing. 05:41 So, of course, gentle suction and then anticholinergic agents, such as hyoscyamine, can be helpful or even the use of atropine eyedrops titrated orally under the tongue can help with the amount of secretions and make everyone more comfortable. 05:59 But do understand that oftentimes secretions are what's known as the death rattle in the hours before death when patients really don't have the ability to clear their secretions very well. 06:12 Many times are not that distressing to the patient, but they can be very distressing to the family. 06:17 So, you may want to reassure family members as well and loved ones that are in attendance near the time of death that this is actually something very normal and that isn't that disturbing to the patient and, therefore, you don’t necessarily want to overtreat it.
About the Lecture
The lecture Death and Dying by Charles Vega, MD is from the course Geriatric Care. It contains the following chapters:
- Death and Dying
- Pain Management
- Manage Opioid Side Effect
Included Quiz Questions
Which of the following medications are the mainstay of treating pain in the last days of life?
- Opioids
- Benzodiazepines
- Corticosteroids
- Nonsteroidal anti-inflammatory drugs
- Acetaminophen
Which of the following medications is most appropriate for control of both pain and dyspnea at the end of life?
- Opioids
- Benzodiazepines
- Corticosteroids
- Nonsteroidal anti-inflammatory drugs
- Acetaminophen
Which of the following medications is most likely to cause arrhythmias?
- Methadone
- Gabapentin
- Lorazepam
- Morphine
- Ibuprofen
Corticosteroids may be used in the management of which of the following symptoms at the end of life?
- Pain
- Incontinence
- Psychosis
- Excessive secretions
- Delirium
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |