Playlist
Show Playlist
Hide Playlist
Control of Adult Male Hormonal Secretion
-
Slides Reproductive Hormonal Pathophysiology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
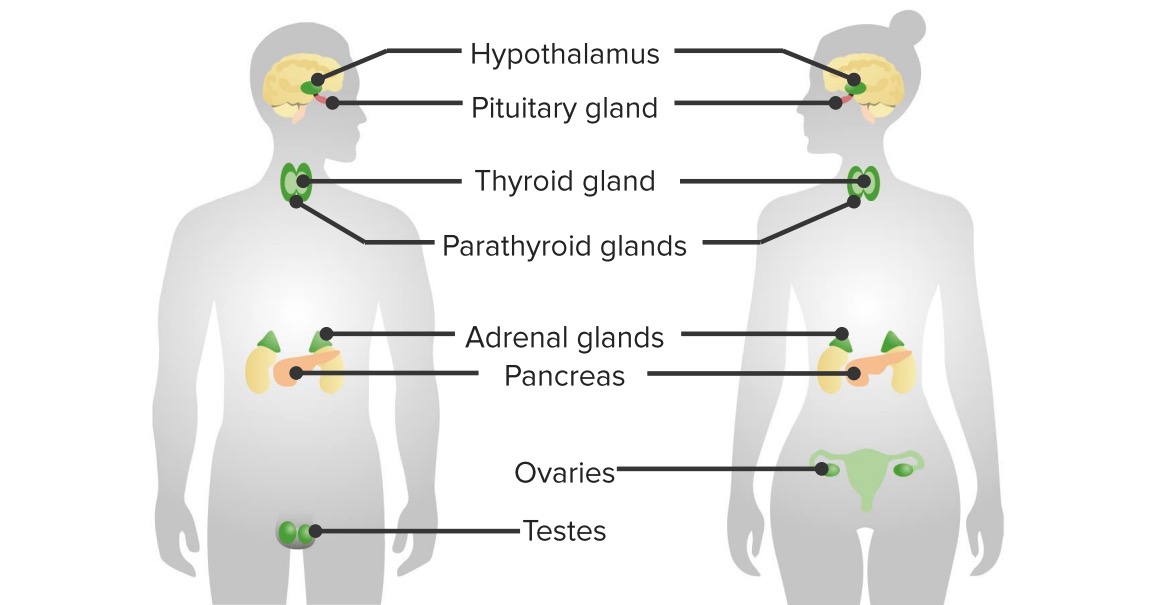
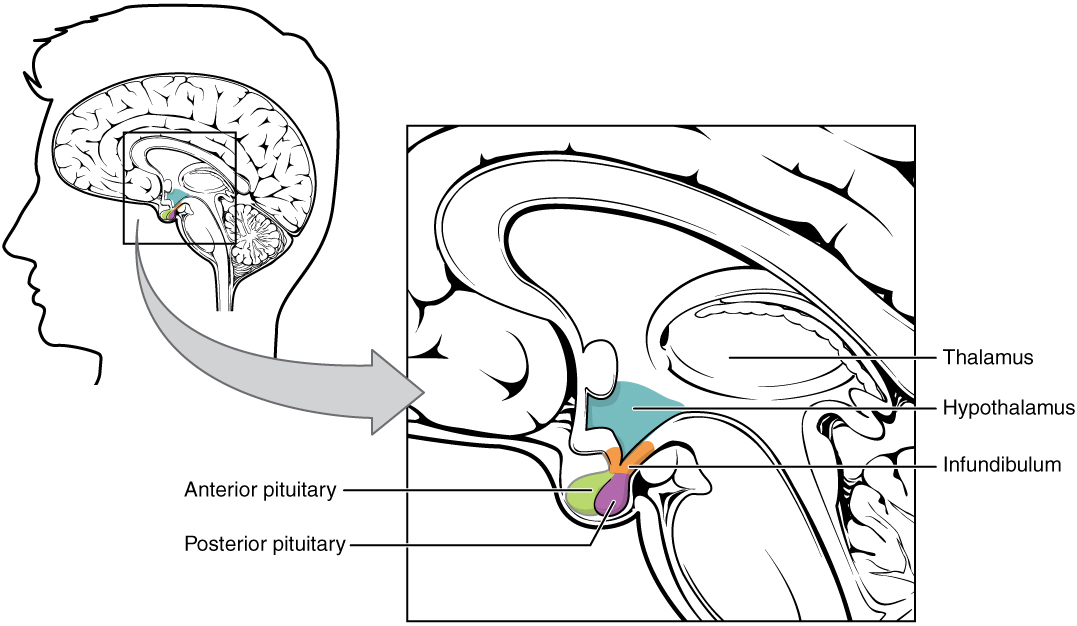
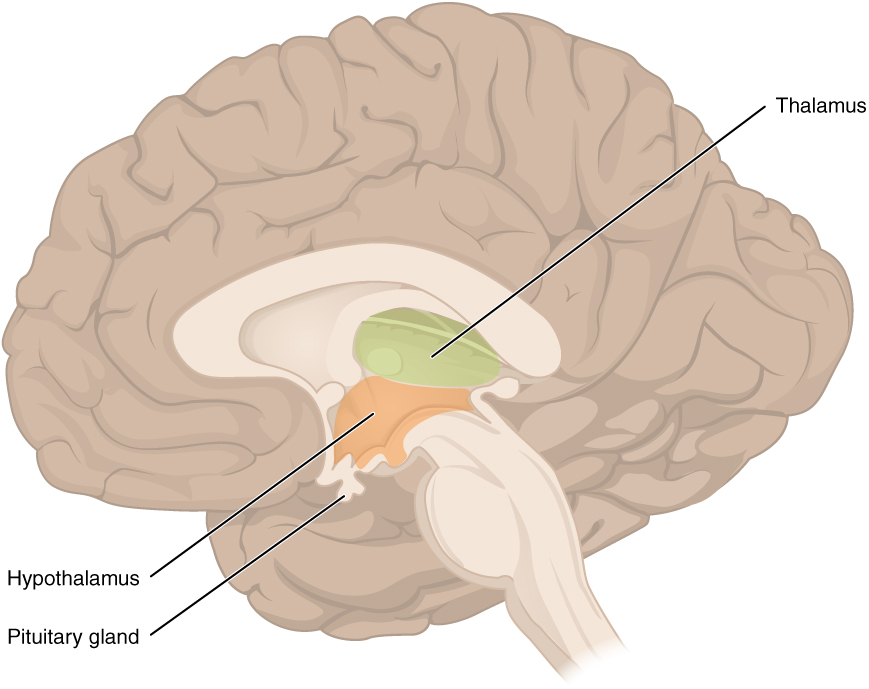
00:00 In this topic of reproductive hormonal pathophysiology, I'm going to emphasize quite a bit of normal so that by the time we get into abnormal, things are crystal clear. We'll begin by looking at the control of adult male hormonal secretion. Close your eyes. Conceptualize this. We'll begin with hypothalamus. Next, tell me about the manner in which gonadotropin releasing hormone, GnRH is being released. Pulsatile, boom, boom, boom, boom, boom. 00:35 Out comes my GnRH. It works upon the anterior pituitary. From the anterior pituitary, out then comes the LH and FSH. Identify the LH. The LH works down on the testes. 00:50 So it arrived into circulation. It has moved down into the testis. 00:56 On the testis, it is then bound to LH receptors. It will then go through cyclic AMP, protein kinase, and will then activate a very important enzyme known as desmolase which will then convert cholesterol into testosterone. Do you remember all these? Stop. 01:14 Now, you're in the testis and testosterone is required for spermatogenesis. 01:23 You're going to move the testosterone which is lipid soluble from the Leydig cell which is the outer or superficial cell into your inner cell which is known as your Sertoli cell. Of the two cells here, I would want you to focus upon the inner Sertoli cell. Because of all the important functions that it has, I'm not by any means dismissing the responsibility by Leydig but the Leydig in general is providing testosterone for the Sertoli cell. Now, if you produce your testosterone, it goes into Sertoli cell. In the meantime, the Sertoli cell is the home of your sperm. Not immature sperm, that's for sure. 02:10 S - Sertoli, S - spermatogenesis. What hormone must you have in the Sertoli cell to properly influence spermatogenesis? Now, that's signal transduction. That's at this point beyond your pay grade. But you definitely need to know that testosterone is responsible for proper spermatogenesis. 02:31 So at any point in time, any pathology that you come across in which testosterone is not present in adequate amounts, your male is infertile, period. 02:42 You can have enough sperm. The sperm count could be normal but you want to have proper spermatogenesis. It is that important. 02:50 Now, with that said, you take a look at testosterone and you see there are two routes of exit from your Leydig cell. Do you see there? The first route of exit we will focus upon will be into your right and into the Sertoli cell. Lipid soluble, no problem passing through the - what's the name of this barrier? Well, some would say the blood–brain barrier. 03:14 But I would recommend clinically that you do not. This is the blood-testis barrier. 03:19 The testosterone will pass through the blood-testis barrier. 03:24 I'm in my Sertoli cell but this is lipid soluble. How can you guarantee that testosterone will not leave the Sertoli cell? The Sertoli cell then contains a binding protein. This is specifically called an androgen-binding protein, androgen-binding protein. Now, with the binding proteins, we've talked about the concept a number of times. It is important for you to know your actual binding globulins that the liver produces versus the binding proteins that you find within the individual cells. We had the same conversation earlier with thyroid-binding globulin, inter-globulin. We're having the same conversation now with testosterone, with androgen-binding protein and and your sex hormone binding globulin from the liver. Why do you need this in the Sertoli cell? So you can anchor the testosterone in your Sertoli cell so that you can properly mature your sperm. All the sperm is being deposited into what lumen? The Sertoli cell surrounds a seminiferous tubule. Correct? That seminiferous tubule then transports your sperm forward into let's say, the testis, through the epididymis, through the vas. It's stored in your seminal vesicle. In the Sertoli cell, you also have a very important hormone that it produces called inhibin. You focus your view on inhibin, B. 04:59 you'll notice a dash line. The dash line represents the fact that inhibin inhibits anterior pituitary hormones. At any point in time, for example, do you remember our discussion on cryptorchidism and bilaterally? If you did not have inhibin then what happens to my levels of LH and FSH? Obviously increased. Make sure that you use proper and common sense type of feedback physiologic mechanisms. If that's one route, what about the second route of exit of testosterone? I want you to come back to Leydig cell. 05:35 From the Leydig cell this time, I want you to go directly downward into the periphery. There’s every possibility that testosterone also gets into circulation. When it does in the peripheral tissue, there’s an enzyme that is known as 5?-Reductase. What does that 5?-Reductase mean to you? It will convert your testosterone into DHT. How important is that? Really important, dihydrotestosterone. Later on, you and I will be going through certain pathologies in which the receptors aren’t working properly. 06:11 You’re not able to properly convert pathologically your testosterone into DHT. 06:17 Of course pharmacologically, we’ve already talked about BPH without hypertension, benign prostatic hyperplasia. The drug that you’re going to use is to target that very enzyme. I told you about my little, silly story about my hair loss and Propecia being cosmetically a drug that inhibits the same enzyme, 5?-Reductase. If you take a look at the verbiage above, it explains everything that I just walked you through so that you actually see what I’m talking to you about.
About the Lecture
The lecture Control of Adult Male Hormonal Secretion by Carlo Raj, MD is from the course Reproductive Hormone Disorders.
Included Quiz Questions
Which of the following hormones directly controls the release of anterior pituitary gonadotropins?
- GnRH
- Inhibin B
- FSH
- LH
- Testosterone
Which of the following pairs is INCORRECT?
- Cell: Leydig cells Hormone: inhibin B
- Cell: Sertoli cells Function: spermatogenesis
- Cell: Leydig cells Hormone: testosterone
- Cell: Sertoli cells Hormone: FSH
- Cell: Leydig cells Hormone: LH
Which of the following statements is INCORRECT?
- Testosterone moves through an active channel to cross the blood-testis barrier.
- The intratesticular concentration of testosterone is 50 times the peripheral concentration.
- Testosterone is produced by Leydig cells under the control of LH.
- Testosterone can be kept inside Sertoli cells by binding to ABP.
- Testosterone can be converted by 5-alpha-reductase into DHT.
Which of the following statements is INCORRECT?
- The amount of testosterone and sperm produced by the testes is dependent on the influence of FSH alone.
- Blocking of 5-alpha-reductase enzyme is used to treat some diseases where DHT can cause or potentiate the disease.
- FSH controls the spermatogenesis process by Sertoli cells.
- Testosterone will be kept inside Sertoli cells and affect the maturation process of spermatogenesis.
- Inhibin B exerts a negative feedback on the production of FSH.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Doctor Raj is very clear in his explanations. This has helped a lot.