Playlist
Show Playlist
Hide Playlist
Comparing Hyperglycemic Hyperosmolar Syndrome (HHS) and Diabetic Ketoacidosis (DKA)
-
Slides 02-03 Diabetes Mellitus part 2.pdf
-
Reference List Endocrinology.pdf
-
Reference List Diabetes Mellitus.pdf
-
Download Lecture Overview
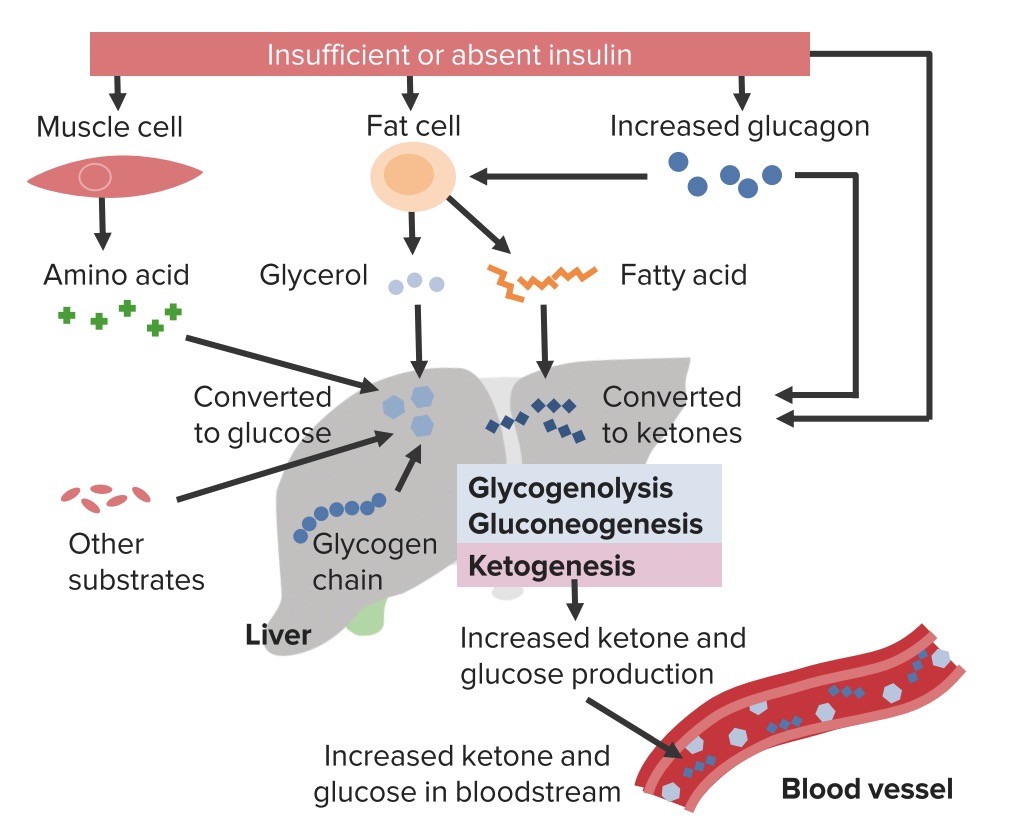
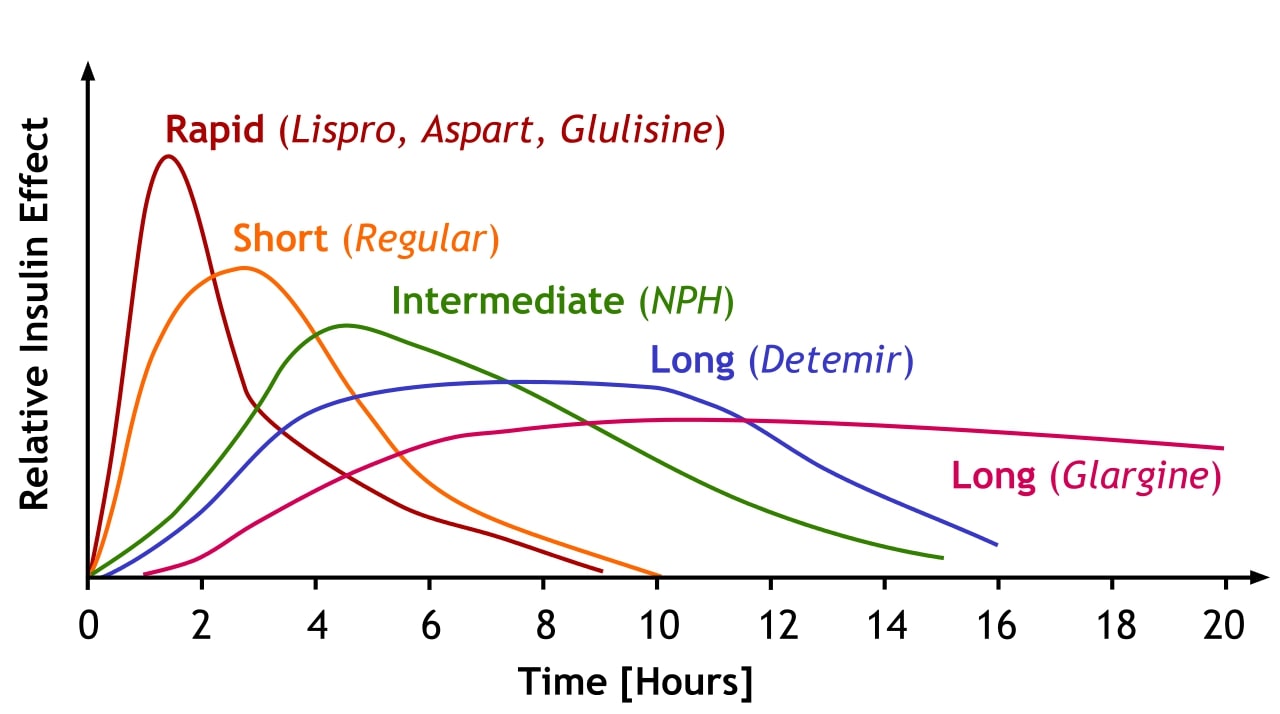
00:00 There are several risk factors that can precipitate extreme hyperglycemia in both DKA and hyperosmolar hyperglycemic syndrome. This include infections, intentional or inadvertent insulin therapy non-adherence, myocardial infarctions, stress, trauma, and confounding medications like glucocorticoids or atypical antipsychotic agents of which Clozaril is a good example. Symptoms of extreme hyperglycemia in both conditions include polyuria, polydipsia, unintentional weight loss, vomiting, weakness, mentation changes, dehydration, and metabolic abnormalities worsen as the hyperglycemia progresses and may progress on to respiratory failure. Patients may then become lethargic, obtunded, they may go into a coma and eventually die. DKA can occur within several hours of the inciting event unlike HHS which is less acute and this may take days or even weeks to develop. HHS typically presents with a more extreme hyperglycemia and mental status change. 01:16 The initial evaluation of severe hyperglycemia should involve the following serologic tests. We start with plasma glucose, serum ketones, blood urea nitrogen, creatinine, electrolytes, and calculate the anion gap. From there, we go on to assess the arterial blood gasses to determine the acid-base status. It's also a good idea to calculate and measure the osmolarity. Complete blood count will be helpful as well. These patients usually develop these extreme conditions because of underlying infections and blood cultures will be very important to obtain too. Likewise, urine studies will help with determining if there is ketone in the urine and also for urine culture to rule out the presence of a urinary tract infection. A chest radiograph is helpful to rule out the presence of an underlying occult pneumonia. And then finally, an ECG is helpful because it allows you to determine whether any electrolyte abnormalities are also represented in EKG changes or in turn if there is an underlying silent myocardial infarction that precipitated the entire process. HHS typically presents with normal or small amounts of urine or serum ketones. Plasma glucose values in this condition are typically greater than in DKA and can exceed 1200 mg/dL. The serum osmolarity is elevated greater than 320 mOsm/kg water. Serum bicarbonate levels are greater than 18 mEq/L and the pH remains greater than 7.3. In DKA on the other hand, ketones are a primary feature. 03:02 Urine and serum ketones are elevated in DKA and a negative measurement though does not necessarily exclude it. Beta hydroxybutyrate is the major ketone body in DKA, but ketone laboratory measurements may often use the nitroprusside reaction. This particular measurement technique only estimates acetoacetate and acetone levels, which may not be elevated initially. Acid-base status in DKA. 03:31 The anion gap is invariably elevated especially when ketones start appearing within the urine and blood. As far as leukocytosis goes, a stress-related mild increase in the white count is often present. Also, higher levels of leukocytes may indicate the presence of an underlying infection. 03:52 In DKA, hyperglycemia is the typical finding at presentation. It has a range of values including normal. The serum sodium is normal or elevated due to severe volume depletion. It can be low due to osmotic shifts of water from the intracellular to the extracellular space, a condition known as pseudohyponatremia. As far as potassium is concerned, this is elevated due to shifts from the intracellular to the extracelluar space due to ketoacidosis and the absence of sufficient insulin. 04:28 Normal or low levels of potassium indicate low stores within the body and will require correction prior to starting insulin therapy to avoid worsening of the hypokalemia and further cardiovascular arrhythmias. Serum amylase and lipase can also be elevated in the absence of pancreatitis in DKA. 04:51 Let's talk about the general principles in the treatment of DKA and hyperosmolar syndromes. 04:57 First, correction of the hyperglycemia with intravenous insulin infusions. Frequent monitoring and replacement of electrolytes will be necessary, correction of hypovolemia with intravenous fluids is a major component and ICU admission for management of severe hyperglycemia because of frequent monitoring that is required with intravenous insulin therapy, electrolyte abnormalities, and possible cardiac effects. Plasma glucose levels should be monitored initially every hour while on insulin infusion therapy. Electrolytes should be monitored every 2-4 hours depending upon the initial deficits and the level of acidosis. Fluid management involves assessing for volume status and giving 0.9% saline at 1 L/hour initially in all patients. Continue this especially if the patient is severely hypovolemic. Switch to 0.45% normal saline at about 250-500 mL/hour if the corrected serum sodium level becomes normal or high. When the plasma glucose levels reach 200 mg/dL in patients with DKA or 300 mg/dL in patients with HHS, switch to 5% dextrose with 0.5 normal saline at 150-250 mL/hour. In terms of insulin correction, give regular insulin 0.1 units/kg as an intravenous bolus followed by 0.1 unit/kg/hour as an intravenous infusion. If the plasma glucose level does not decrease by 10% in the first hour, give an additional bolus of 0.14 units/kg and resume the previous infusion rate. When the plasma glucose level reaches 200 mg/dL in DKA and 300 mg/dL in HHS, reduce to 0.02-0.05 units/kg/hour and maintain the plasma glucose level between 150 and 200 mg/dL until the anion gap is resolved in the case of DKA. With regards to the management of potassium, assess for adequate kidney function and check the urine output. You really would like it to be above 50 mL/hour. If the serum potassium is less than 3.3 mEq/L, don't start insulin. Give intravenous potassium chloride at 20-30 mEq through a central line. 07:34 Add 20-30 mEq of potassium chloride to each liter of intravenous fluid to keep the serum potassium level in the 4-5 range. If the serum potassium level is greater than 5.2, start the insulin and intravenous fluids and check the serum potassium level every 2 hours. Remember when you start the insulin, it's going to drive the potassium from the serum into the intracellular space and may lead to a reduction in potassium levels. That's why when you start insulin you need the potassium to be on the higher end. In terms of the acidosis, if the pH is less than 6.9, give sodium bicarbonate 100 millimoles in 400 mL of water and potassium chloride 20 mEq over 2 hours. If the pH is 6.9 or greater, do not give bicarbonate replacement. Let's compare and contrast some of the features of DKA and HHS. First of all, DKA is more common in type 1 diabetes. It has a rapid onset and may occur within less than 24 hours. It usually results in profound mentation alterations. 08:50 Abdominal pain, nausea, vomiting, and Kussmaul breathing indicating an underlying metabolic acidosis are often present. Glucose levels usually range between 250 and 500 mg/dL. Bicarbonate is usually less than 15 mEq/L. In contrast, hyperosmolar hyperglycemic syndrome is much more common in type 2 diabetes mellitus. It's a gradual onset and takes days to weeks to manifest. Patient's altered mentation is more pronounced and may even be associated with focal neurologic signs. Less common findings are abdominal pain, nausea, vomiting, and Kussmaul breathing. Glucose levels are usually greater than 600 mg/dL. However, bicarbonate levels usually exceed 15 mEq/L. 09:46 Furthermore, in DKA, the anion gap is increased. Serum ketones are positive and serum osmolarity can be variable. In hyperosmolar hyperglycemic syndrome, the anion gap can be normal, in serum ketones, negative or mildly increased, and finally serum osmolarity as you would expect is greater than 320 milliosmoles.
About the Lecture
The lecture Comparing Hyperglycemic Hyperosmolar Syndrome (HHS) and Diabetic Ketoacidosis (DKA) by Michael Lazarus, MD is from the course Diabetes Mellitus. It contains the following chapters:
- HHS vs. DKA
- Treatment of DKA and HHS
Included Quiz Questions
Which of the following is NOT a common precipitant of HHS or DKA?
- Excessive insulin administration
- Myocardial infarction
- Sepsis
- Dehydration
- Prednisone
Which of the following correctly characterizes the laboratory findings of HHS compared to DKA?
- HHS does not show an anion gap, but DKA shows an anion gap.
- DKA typically presents with much higher plasma glucose readings than HHS.
- Serum osmolality is typically higher in DKA.
- pH is typically lower in HHS.
- Bicarbonate level is typically higher in DKA.
Which of the following best characterizes the potassium levels in DKA?
- Hyperkalemia is caused by potassium shifting out of cells in acidic conditions.
- Failure to correct potassium levels can lead to uncontrolled hyperkalemia as DKA is treated.
- Patients with DKA typically present with concomitant hypokalemia.
- There is usually no potassium disturbance in DKA.
- If there is hyperkalemia, it is a direct result of hyperglycemia.
Which of the following is NOT a tenet of DKA treatment?
- Starting subcutaneous insulin immediately
- Aggressive intravenous fluid administration
- Hourly glucose checks
- Electrolyte checks every 2–4 hours
- Adding dextrose to intravenous fluids once the serum glucose level drops below 200 mg/dL
What is one physical examination finding typical of DKA that you may not expect to find in HHS?
- Kussmaul breathing
- Sunken orbits
- Skin tenting
- Focal neurologic signs
- Nausea
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |