Playlist
Show Playlist
Hide Playlist
Overview – Cell Wall Synthesis Inhibitors (Antibiotics)
-
Slides Overview Cell Wall Synthesis Inhibitors Antibiotics.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
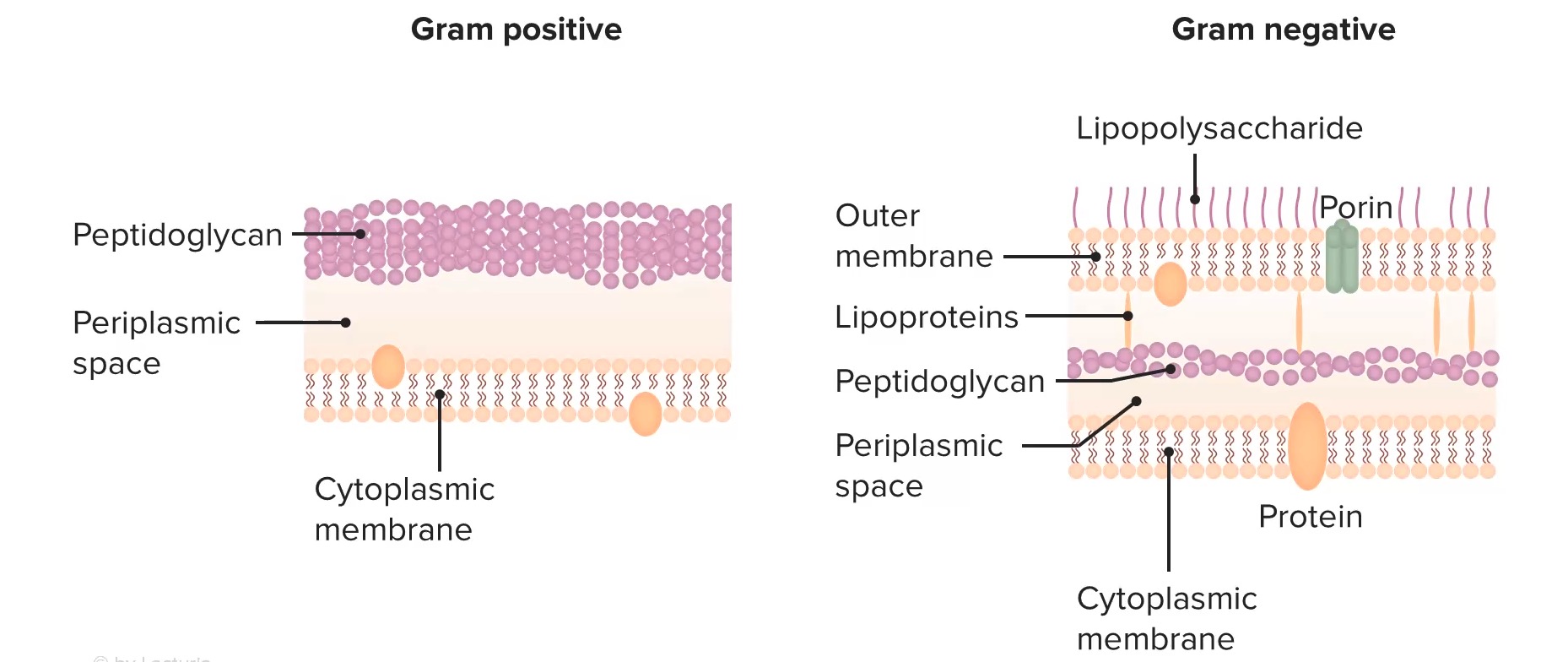
00:01 Welcome to pharmacology by Lecturio. 00:03 I'm Doctor Praveen Shukla and we're going to talk today about antibacterial agents. 00:09 Antibacterial agents fall in several categories. 00:12 We've divided them up here into bacterial cell wall inhibitors, bacterial protein synthesis inhibitors, agents acting against DNA and folic acid, and the anti mycobacterial agents. 00:25 To start off with, let's look at the bacterial cell wall synthesis inhibitors. 00:29 We divide these up into several classes. 00:31 We have the oldest of the group which are the penicillins, cephalosporins, the penems and other miscellaneous agents. How is it that we build a cell wall? Well, cell wall synthesis in the bacteria starts with two major proteins. 00:48 The first one is n-acetylmuramic acid. 00:51 The second is n-acetylglucosamine. 00:53 We'll call them NAM and NAG, just to make things a little simple. 00:56 Now they get joined together like cars on a train. 00:59 So there's a very long chain of these NAM and NAG particles that make up a train. 01:05 In order to make a wall, we need two trains bound together. 01:09 So what we do is we take two chains, chains of amino acids, and we lash them together. 01:15 Now, right now, when you look at them in the picture here, it's just a loose knot. 01:20 But what we're going to do is we're going to use a thing called a penicillin binding protein. 01:24 Now this protein comes along, cleaves off two of the end units, binds them together tightly and keeps on doing that over and over again until you have a very long set of two trains hooked together to make a strong cell wall for the bacteria. 01:44 How do we stop the production of this wall? We use something called a β-lactam antibiotic. 01:50 Now, this β-lactam ring binds to the penicillin-binding protein and prevents it from doing its job. 01:57 What ends up happening is you have a wall that isn't being built. 02:02 The β-lactam antibiotic binds to the penicillin-binding protein, and it prevents the cross-linking of NAM and NAG chains to each other. 02:14 Well, what does that do to an existing bacteria? Nothing. The cell wall was already built. 02:19 What really matters, though, is when the cell wall, pardon me,when the cell wants to start replicating itself. 02:26 So as the cell stretches and decides to divide, the dividing cell can't build new cell wall. 02:35 What you end up with is the existing bacteria and something else called a spheroplast. 02:41 Well, what's a spheroplast? Essentially, a spheroplast is a bacteria without a cell wall. 02:46 Now these spheroplasts are essentially useless. 02:49 They can't do what they're supposed to do, which is infect the body. 02:53 So bacteria that attempt to grow and divide in the presence of penicillin end up shedding their cell walls, and they stop dividing. 03:03 The remaining spheroplasts auto catalyze. 03:06 They break down on their own and they die. 03:09 How is it that we get resistance to these antibiotics? There's three major ways. 03:14 First, there's β=lactamase mediated resistance. 03:18 Now what is β-lactamase mediated resistance? β-lactamases are enzymes within the bacteria itself that actually break down that β-lactam ring. 03:27 If you think about it, it's kind of like warfare. 03:30 The mechanism of most types of resistance occurs through β- lactamases. 03:36 They break down the very antibiotic that's supposed to be killing them. 03:40 This will affect many antibiotics that have a β-lactam ring. 03:44 So this includes the penicillins, the cephalosporins, some of the cephamycins and other carbapenems. So what is a β-lactamase? Well you have here a picture of a β-lactamase. 03:57 It's a beautiful illustration. 03:59 You can see how complex a structure this actually is. 04:03 They're also called penicillinases or cephalosporinases. 04:07 But I would just like you to use the term β-lactamase, because it really reminds us of where these drugs are acting. Now they're produced by gram-positive organisms, but they also can be produced by gram-negative organisms. 04:20 They're usually secreted and may be secreted in response to the presence of an antibiotic. 04:26 So sometimes β-lactamase mediated resistance isn't really obvious until you actually expose the organism to an antibiotic. And then all of a sudden you realize, oh my gosh, this this particular organism is resistant. 04:39 This has become a huge problem now with cephalosporins. 04:42 And of course, you all probably know already that we use cephalosporins much more than we have been using penicillins. Now, sometimes the resistance with cephalosporins is a little bit different. 04:54 This is a new chromosomal-mediated mechanism. 04:57 It's a new threat that we're starting to see. 04:59 We started to see it around 2016 and over the last several years has become more and more prominent. 05:06 We're also seeing now β-lactamase mediated resistance with some of the cephamycins. 05:10 So this is something that we're seeing more and more over time. 05:14 It's going to be more and more important as, as practice goes on. 05:19 Now what do we do about these β-lactamases? Well, specifically with the penicillin based β-lactamases, we can counter it with certain types of inhibitors of these enzymes. One of them, and probably the most commonly known is clavulanic acid. 05:33 So for example, we will pair clavulanic acid with amoxicillin so that we have a combination of medications that's relatively β-lactamase resistant. 05:44 Sulfur bacteria is another one. 05:46 We put it together with ampicillin or tazobactam. 05:49 We'll put together with piperacillin as combination products. 05:53 And they're often sold as combination products on the market. 05:57 The other way that we develop resistance to the β-lactam antibiotics are penicillin-binding protein-mediated resistance mechanisms. 06:06 So this is actually a lot simpler than it sounds. 06:09 Basically, we have a penicillin-binding protein that is resistant to the effects of the β-lactam. 06:16 Now how does that work? Now if you look here we have a picture of naked DNA from the resistant bacteria. 06:23 That naked DNA actually gets incorporated into the cell. 06:27 The host DNA is now changed. 06:30 Okay. When that host DNA produces a new penicillin binding protein, it's slightly different. 06:37 And it's different enough that it is resistant to the β- lactam but is still able to produce a cell wall. 06:43 So you can actually have transmission of DNA from one bacteria to another that provides the resistance. And you produce new penicillin-binding proteins. 06:54 This gives you a reduced affinity to the new β-lactam antibiotic, or to the old β-lactam antibiotic. 07:00 And that's how these types of resistances spread. 07:03 The third type of resistance is called porin-mediated resistance, and it sounds exactly like it is. 07:11 So porins are basically pores. 07:14 They're water-filled channels. 07:16 Here's a beautiful illustration of a porin. 07:19 Now, a porin is a tubular structure that is seen in the cell walls. 07:23 The antibiotics travel through porins to get inside the bacteria. 07:28 But if you have a bacteria, for example, that adapts and makes fewer porins, you'll have less ability for the antibiotic to get in. 07:37 And we see that actually in Pseudomonas all the time. 07:40 Pseudomonas is very commonly recognized as one of the agents that has porin-mediated resistance. 07:46 Now I'll give you a trick for the exams. 07:48 Porin-mediated Pseudomonas both start with P. 07:51 And this is something that got me through at least one of the questions on my exam. 07:55 So try to remember Porin Pseudomonas makes things a little bit easier to remember.
About the Lecture
The lecture Overview – Cell Wall Synthesis Inhibitors (Antibiotics) by Pravin Shukle, MD is from the course Antimicrobial Pharmacology.
Included Quiz Questions
Regarding cephalosporins, which statement is TRUE?
- They inhibit the synthesis of the bacterial cell wall.
- They are used as fungal and bactericidal drugs.
- They inhibit protein synthesis.
- They inhibit dihydropteroate synthase.
- They are more susceptible to penicillinase than other penicillins.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
hello Lecturio Im from Philippines Im so happy that I came to find this very knowledgeable site where I can learn sruffs related to my course which is Pharmacy.
1 customer review without text
1 user review without text