Playlist
Show Playlist
Hide Playlist
Breast Cancer Screening
-
Slides BreastCancerScreening PreventiveMedicine.pdf
-
Download Lecture Overview
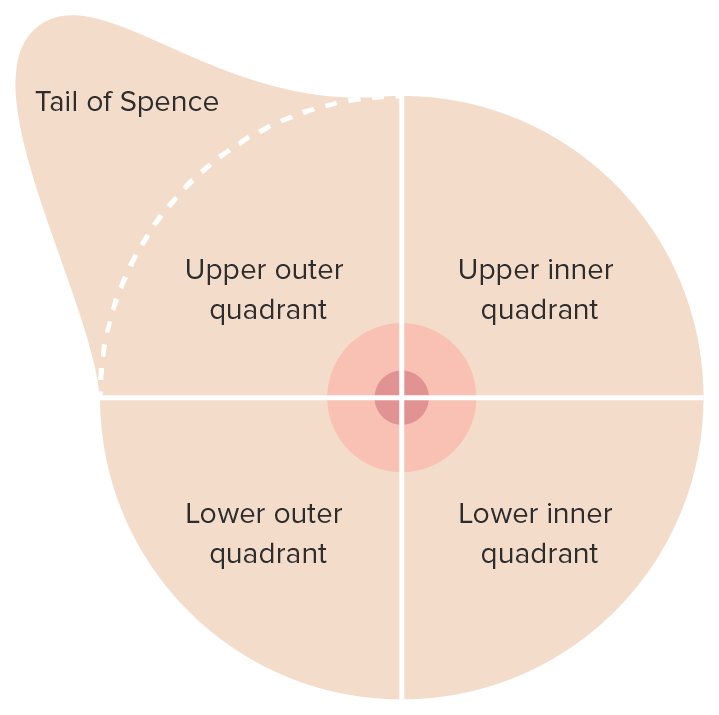
00:01 All right. 00:01 So breast cancer screening is so important and so controversial that it really merits its own discussion. 00:07 So I’m going to try to talk about the guidelines and recommendations for breast cancer screening and also impart some of those controversial areas that you can inform your patients about because at the end of the day, it’s about shared decision-making and what the patient really wants in terms of breast cancer prevention. 00:25 So let’s start with a case. 00:26 You’re seeing a 45-year-old woman, she has no risk factors for breast cancer, and she’s interested in initiating breast cancer screening. 00:33 That’s great. 00:35 Which of the following screening tools is the most proven in reducing breast cancer mortality? Is it MRI, a clinical breast examination by a physician or by a healthcare provider, self-breast examination at home, or mammography? The answer is mammography, and mammography is not perfect, but it certainly has the strongest record of evidence and probably the best balance between picking up early tumors and a lower false-positive rate, and so we’ll talk about these things as we move through the topic. 01:11 Breast examination certainly has a role. 01:13 Self-examination has been demonstrated to increase the number of radiographic studies ordered. 01:19 Patients come in, “I think I feel something new on my breast,” automatically going for a diagnostic mammogram and an ultrasound. 01:25 And it also increases the risk of getting biopsies, so these are actual procedures with potential complications, but it hasn’t necessarily been demonstrated to improve breast cancer mortality, and therefore, it’s generally discouraged certainly by organizations such as US Preventive Services Task Force. 01:41 A clinical breast examination alone is insufficient in terms of finding cancer and therefore it can’t replace mammograms. 01:51 But I do believe that personally it’s better to do a clinical breast examination before referring a patient to a mammogram because you might be able to find some abnormality or even just some degree of fibrosis that you can tell the radiology department to be on the watch for and may change a screening mammogram into a more diagnostic mammogram and therefore a more accurate mammogram. 02:16 So certainly, try to do a clinical breast examination before sending on a mammography. 02:21 Okay. 02:21 So let’s think of another important question facing us as we see this 45-year-old woman without risk factors for breast cancer. 02:29 What should we recommend to her regarding the USPSTF rules for screening for breast cancer among average-risk women? Should screening definitely be initiated by age 40? Should it definitely be initiated by age 50? MRI should replace mammography as the test of choice? Or D, Routine mammography should be continued until age 85? And the answer is B, that screening should definitely be initiated by age 50. 02:57 And here we start delve into some of really the controversial issues around breast cancer screening. 03:05 And it’s worth it I think to use a graph like this, which this is a graph plotting the NNS or number needed to screen to prevent one breast cancer death. 03:15 So for among women between the ages of 40 to 49, about 1,900 women needed to be screened to prevent one breast cancer death. 03:24 Meanwhile, many of these women will be recalled for abnormal exams, abnormal mammograms, that turn out to be eventually normal. 03:33 But extra testing, even some biopsies that will be done, they are unnecessary. 03:39 So that’s one balance. 03:41 That number needed to screen drops as women get older to a little over 1,300 between the ages 50 to 59 years. 03:51 But look what happens by the time they hit 60 to 69 years of age. 03:55 That number drops precipitously. 03:57 And the risk of breast cancer is really fairly linear with age, so as women get older, therefore, they do have a higher risk. 04:05 That’s what led the US Preventive Services Task Force to recommend against routine screening between the ages of 40 and 49, but that’s a hugely controversial call and, therefore, it’s really something that other societies still recommend at least every other year mammography, if not annual mammography in the period between ages 40 to 49 years. 04:30 And the least you want to do is shared decision-making, is explain that higher number needed to screen among women aged 40 to 49, the risk for false-positive results is fairly high, and therefore that’s something that women need to be aware of. 04:49 But they also need to be aware that tumors discovered between ages 40 to 49 when they’re cancerous also tend to be more aggressive as well. 04:58 Then on the back end, there isn’t as much to recommend in terms of evidence screening for breast cancer above age 75, but the trend is clear that the risk of cancer continuous to grow as women grow older. 05:18 So therefore, I really would consider it for breast cancer screening, women who are older than 75 but have a good five to ten-year life expectancy, where it looks very positive; they’re active, they’re healthy, which is a large proportion of those women, should be recommended at least to consider continuing mammography. 05:38 And then in the last years of life, when patients may be faced with conditions such dementia or severe cardiovascular disease, that’s not a time to continue, really, any cancer screening including breast cancer screening. 05:51 But it remains a controversial area, one that hopefully you’re fairly informed about. 05:58 How often to screen? In Europe, biannual screening is generally the rule. 06:04 It’s more efficient overall in identifying cases of breast cancer and that it has a lower false-positive rate and a lower number needed to screen. 06:15 But most US organizations continue to advocate for annual screening for breast cancer. 06:21 Other considerations in screening for breast cancer: Ultrasound alone is not enough. 06:27 MRI does have an increased sensitivity, but the sensitivity is actually too high and therefore there are high rates of false positive studies. 06:36 And so routine screening with MRI is not recommended and should be reserved only for those women at the highest risk of breast cancer as I mentioned. 06:47 And one other thing that’s a good pearl that I’m not sure every student gets is that in doing that clinical breast examination, when I find a new palpable lesion in a woman who’s 50 years old or more, not only would I recommend diagnostic mammography and probably ultrasonography at the same time, but I’ll also do a concomitant referral to a breast surgeon because that case might need a tissue diagnosis such as a fine-needle aspiration in order to get an extra level of security that this indeed isn’t some type of a cancerous tumor. 07:22 All right. 07:23 So we covered the controversial issue of breast cancer screening particularly the initiation and termination of said screening in a fairly brief and efficient way, but I hope you found it really helpful. 07:36 Thanks for paying attention.
About the Lecture
The lecture Breast Cancer Screening by Charles Vega, MD is from the course Preventive Medicine. It contains the following chapters:
- Breast Cancer Screening
- Breast Examination
- Controversies in Starting and Stopping Mammography
- Other Considerations
Included Quiz Questions
What test or examination is most proven at reducing breast cancer mortality?
- Mammography
- Self breast examination
- Clinical breast examination
- Genetic testing
- Low-dose CT
Which of the following statements regarding breast cancer screening is FALSE?
- Breast self-examination is recommended by the US preventive screening task force.
- Breast self-examination increases potential biopsy rate.
- Breast self-examination increases the frequency of radiographic studies.
- Clinical breast examination is not the recommended screening tool.
- Mammography is an important screening tool for breast cancer.
How often is breast cancer screening with mammography for average-risk women aged 50 to 74 years recommended?
- Every 1-2 years
- Every 6 months
- Every 3-4 years
- Every 5 years
- Every 10 years
What is the initial step in the workup of a palpable mass in the breast of a 50-year-old woman?
- Mammography
- Fine-needle aspiration
- Magnetic resonance imaging
- Core needle biopsy
- Computed tomography scan
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |