Playlist
Show Playlist
Hide Playlist
Bacterial Meningitis: Management & Empirical Treatment When Gram’s Stain (-)
-
Slides Meningitis InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
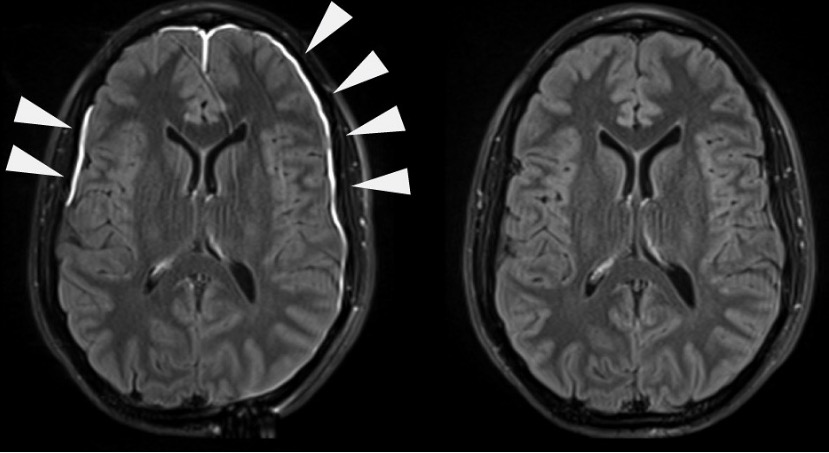
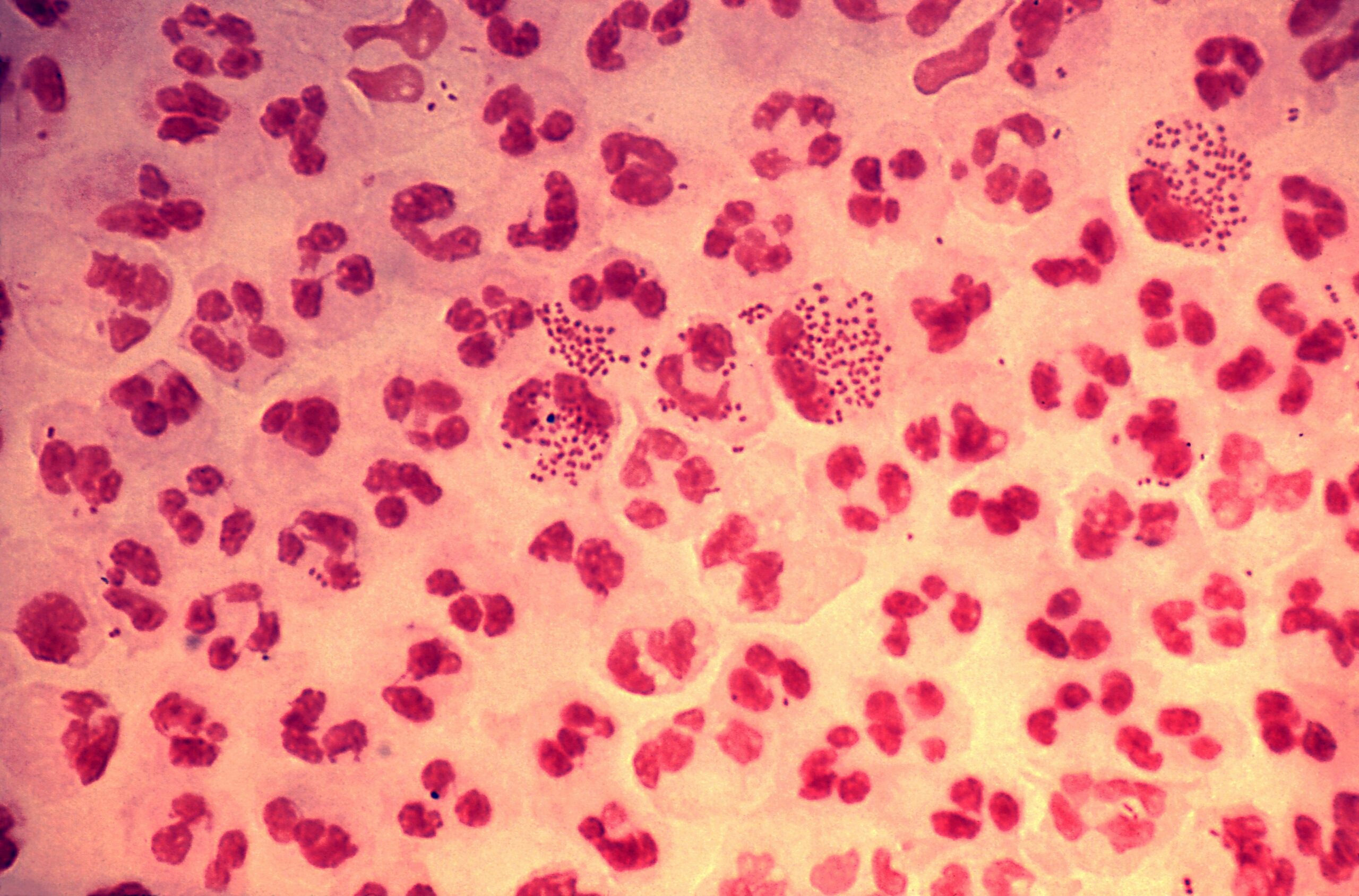
00:02 So, how do you manage bacterial meningitis if the Gram stain is negative? In other words, you're not sure what you're treating. 00:12 Well, you would have to treat for all pathogens that might be present. 00:17 So, in a patient from the age of one month to 50 years of age, you're going to be using ceftriaxone and vancomycin. 00:28 And notice that we’re adding a corticosteroid with that, dexamethasone. 00:33 And the main reason for dexamethasone is to reduce the amount of inflammation that is present because the inflammation causes increased intracranial pressure and may cause some of the irreversible damage that happens because of the inflammatory response in the cerebrospinal fluid. 00:55 Now, there – I've listed there the alternatives for you in patients that cannot take cephalosporins or ampicillin, and that would be meropenem plus vancomycin, again plus dexamethasone. 01:12 Now, if the patient has had some neurosurgery or a cochlear implant or some head trauma, then we need to think about what bugs could cause meningitis there and we’re thinking Staph, we’re thinking Gram-negative rods. 01:28 So, the treatment is going to be vancomycin to cover methicillin-resistant Staph and cefepime, which is an antipseudomonal fourth-generation cephalosporin or ceftazidime, a third-generation, which covers pseudomonas. 01:46 And so, that's what we’re thinking empirically. 01:49 And alternatively, we would use once again meropenem, a carbapenem, plus vancomycin. 01:56 There's not evidence of whether you should use corticosteroids in this setting, but many patients who have had a neurosurgical procedure or trauma are already getting dexamethasone. 02:11 So, now, what if you do have a positive Gram stain, let's say Streptococcus pneumoniae. 02:18 What's recommended is vancomycin plus ceftriaxone plus dexamethasone. 02:26 Now, why vancomycin plus ceftriaxone? There are some pneumococci that are relatively resistant to ceftriaxone, not very common, but vancomycin would be expected to cover that small percentage of pneumococci not susceptible. 02:45 Alternatively, once again, we’re turning to meropenem or moxifloxacin, a fluoroquinolone, plus dexamethasone. 02:56 Or what if your Gram stain shows you evidence of a gram-negative organism, like Haemophilus influenzae or Pseudomonas aeruginosa? Sometimes H. flu can be elongate and resemble other Gram-negative rods, and so the Gram stain doesn't give you certainty. 03:17 So, you're going to have to treat for both, and antipseudomonal cephalosporin will cover both H. flu and Pseudomonas. 03:26 But in this case, because there may be a few percentage that are not covered by these cephalosporins, you would add gentamicin, at least until you get the results of your cultures back. 03:42 And alternatively, you would use once again meropenem, a fluoroquinolone, plus dexamethasone. 03:53 All right. 03:53 If you're pretty sure the patient has that bad meningococcal meningitis, then the treatment of choice in babies, newborns, is actually cefotaxime. 04:05 And cefotaxime and ceftriaxone are very, very similar third-generation cephalosporins bug-wise. 04:13 But because a newborn's liver is not mature, they may not handle ceftriaxone, which is partially excreted by the liver, very well. 04:22 So, you use cefotaxime for newborns. 04:27 Everybody else would get ceftriaxone plus dexamethasone. 04:32 And the reason for ceftriaxone is that you can give it once a day or twice a day at the most. 04:39 And alternatively, it would be penicillin. 04:42 The meningococcus still is completely susceptible to penicillin G or ampicillin or moxifloxacin if patients cannot tolerate a beta-lactam. 04:57 The empirical treatment for a patient suspected of having Listeria on Gram stain would be ampicillin. 05:06 In fact, the organism is more susceptible to ampicillin than it is penicillin G. 05:11 Plus gentamicin for synergism. 05:16 Alternatively, they can receive trim sulfa, meropenem, and questionably this new agent called linezolid. 05:28 But because of some lack of certainty, we add rifampin to that. 05:35 And because of this, this organism is a little bit slow to grow because it's intracellular and more difficult to treat. 05:45 We usually treat this for 21 days, Listeria meningitis. 05:52 Now, if it’s Staphylococcus, we’re going to use vancomycin empirically because of the possibility of methicillin-resistant Staph aureus. 06:05 If we think it's a Streptococcus, then like group B Strep, for example, it would be ampicillin plus gentamicin in a newborn and infants and it would be penicillin in adults. 06:22 Alternatively, if they can't take a beta-lactam, it would be vancomycin. 06:30 Now, what if a patient has visited a doctor's office or is brought to a private physician's office and the private physician feels like they have meningitis. 06:41 Well, of course, they’ve got to transfer them to a hospital. 06:44 There may be valuable time wasted. 06:46 And so, if a private physician happens to have the availability of giving intravenous ampicillin or penicillin, then he or she should do that, just give the medication empirically because of the danger of death with delay. 07:08 Now, the Infectious Disease Society of America guidelines, I will now summarize for you. 07:15 If you have a patient with a suspicion of bacterial meningitis and you have, for example, a patient who is immunocompromised, has a history of papilledema, focal neurologic deficit, or there's going to be some kind of delay in therapy, then that produces an algorithm. 07:40 And you go down one side if the answer is yes and on the other side if the answer is no. 07:46 So, if they do not have any of these, you would go ahead and get blood cultures, you would do a lumbar puncture immediately, you would give dexamethasone and empirical antibiotics. 07:59 You’ve got your cultures cooking. 08:01 And then you would get the spinal fluid analyzed. 08:05 If the findings are consistent with bacterial meningitis, you would continue therapy. 08:12 So, that is if the patient has no immunocompromise, no history of central nervous system disease, no papilledema, no focal neurologic deficit, and you’ve been able to tap them immediately. 08:26 On the other hand, if the answer to that question is yes, then there's going to be a delay. 08:32 You can’t tap them immediately. 08:33 So, you’ve got to get your blood cultures, you go ahead and give them dexamethasone and empirical antibiotics. 08:41 Now, there may be delay in x-ray. 08:45 Well, you don't want the patient to be waiting an x-ray and not have been given antibiotics. 08:51 So, that's why you give them empirical antibiotics and then send them off to x-ray. 08:57 If their head CT scan shows no evidence of increased intracranial pressure, you can now analyze their spinal fluid, a spinal tap can be done.
About the Lecture
The lecture Bacterial Meningitis: Management & Empirical Treatment When Gram’s Stain (-) by John Fisher, MD is from the course CNS Infection—Infectious Diseases. It contains the following chapters:
- Management – Empirical Treatment When Gram’s Stain (-)
- Empirical Treatment Based on CSF Gram’s Stain
- Management Guidelines
Included Quiz Questions
A 61-year-old woman is brought to the emergency department for altered mental status that developed this morning. She has a several day history of fever and productive cough. Two weeks prior, she developed symptoms of acute bronchitis with hoarseness and nasal congestion, which have been slow to resolve. On exam, she is febrile (102°F) and confused. Her pupils are equal, round, regular, and reactive, but she exhibits a left VI nerve palsy. Her lungs reveal dullness to percussion and bronchial breath sounds in the right lower lung field. The heart and abdominal exam is unremarkable, but her neck is stiff and, when flexed, results in bilateral hip flexion. Complete blood count shows a white blood count of 18,000/mm3 with a left shift. Blood cultures are obtained and a lumbar puncture is successfully performed. Which of the following is the most important next step in management?
- Start intravenous ceftriaxone + vancomycin + dexamethasone
- Initiate culture-based antibiotics
- Obtain a brain CT scan
- Start oral amoxicillin/clavulanate
- Obtain Gram stain of sputum
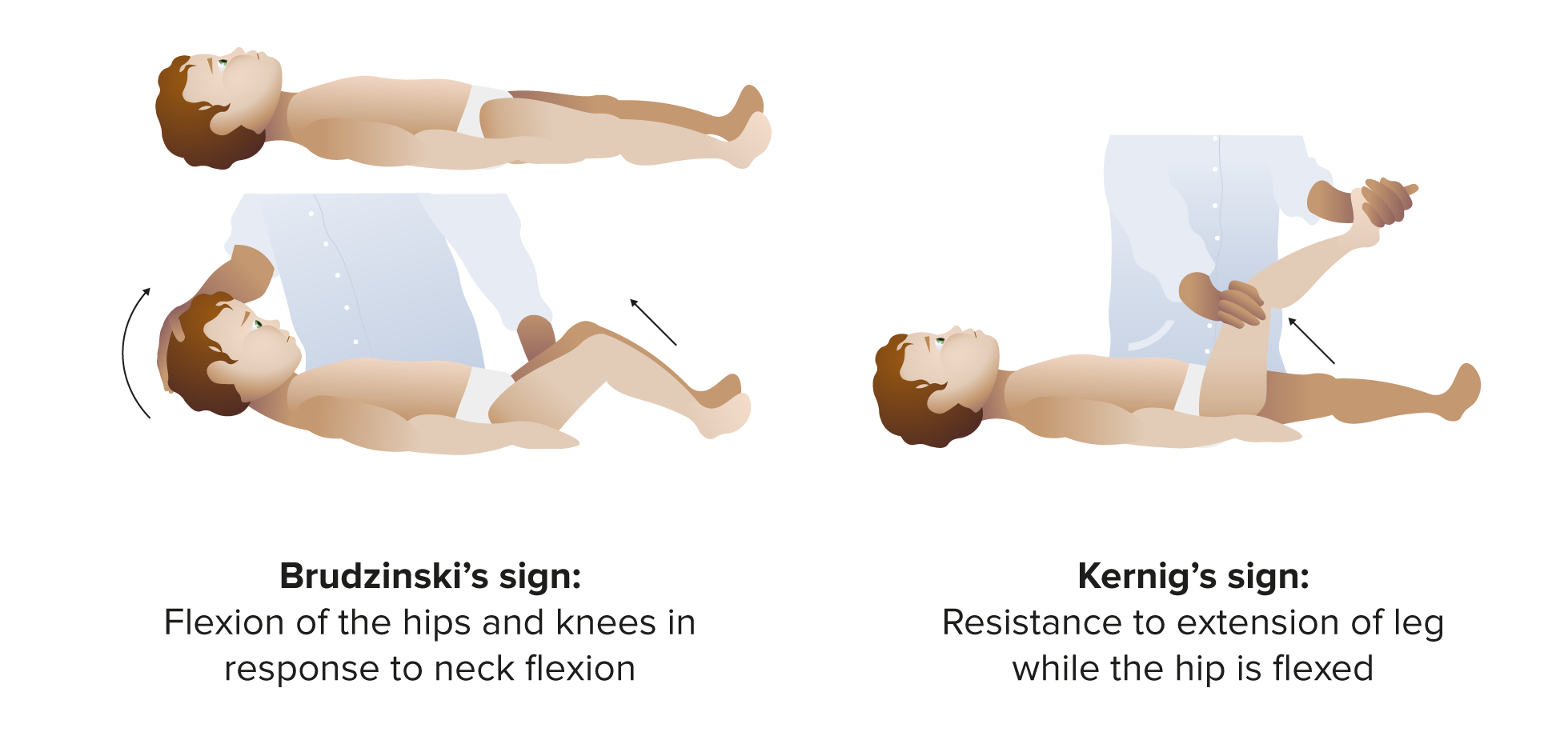
A 35-year-old patient on immunosuppressants for autoimmune disease presents with headache, nausea, vomiting, fever, and meningismus. Physical exam demonstrates bilateral papilledema and positive Kernig and Brudzinski signs. What is the next appropriate step in management?
- Obtain immediate blood cultures and start dexamethasone, ampicillin, ceftriaxone, and vancomycin
- Obtain immediate blood cultures and start vancomycin
- Obtain immediate cerebral spinal fluid cultures and start ampicillin, ceftriaxone and vancomycin
- Obtain brain imaging before performing lumbar puncture
- Obtain cerebral spinal fluid and start appropriate antibiotic therapy based on results Gram stain results
A 14-year-old boy presents with fever, headache, nausea, vomiting, and nuchal rigidity. He recently had a cochlear implant surgery. Which of the following is the most appropriate empiric treatment for the presumed meningitis in this patient?
- Vancomycin, cefepime, and dexamethasone
- Ampicillin, ceftriaxone, dexamethasone
- Vancomycin and dexamethasone
- Ampicillin, gentamicin, dexamethasone
- Cefotaxime, meropenum, ampicillin, and dexamethasone
Cerebral spinal fluid Gram stain shows gram-negative coccobacilli. What pathogens should the patient be treated for until culture is confirmed?
- Haemophilus influenzae and Pseudomonas aeruginosa
- Pseudomonas aeruginosa and Neisseria meningitidis
- Neisseria meningitidis and Haemophilus influenzae
- Streptococcus pneumonia and Listeria monocytogenes
- Listeria monocytogenes and Escherichia coli
A 43-year-old woman had a recent neurosurgery. She now presents with fever, headache, nausea, vomiting, and nuchal rigidity. Which of the following pathogens are the major causes of meningitis in this patient?
- Staphylococci and aerobic gram-negative rods
- Streptococci and staphylococci
- Streptococci and Pseudomonas aeruginosa
- Listeria monocytogenes and group B streptococcus
- Neisseria meningitidis and staphylococci
What is the duration of treatment for Listeria monocytogenes meningitis?
- 21 days
- 10-14 days
- 7 days
- 3 months
- 5 days
Which of the following is an the most appropriate empirical treatment for meningitis in a patient with severe penicillin allergy?
- Meropenem, vancomycin, and dexamethasone
- Ampicillin, ceftriaxone, vancomycin, dexamethasone
- Meropenem, cefotaxime, vancomycin, dexamethasone
- Vancomycin, gentamycin, and dexamethasone
- Vancomycin, ceftriaxone, gentamicin, and dexamethasone
A newborn baby is confirmed to have meningococcal meningitis. Which of the following is the most appropriate antibiotic regimen?
- Cefotaxime
- Ceftriaxone
- Ampicillin and gentamicin
- Vancomycin and cetriaxone
- Carbopenem
Which of the following is the most appropriate antibiotic regimen for neonatal meningitis due to Streptococcus agalactiae?
- Penicillin + gentamicin
- Ampicilin + penicillin
- Meropenem + vancomycin
- Vancomycin + penicillin
- Gentamicin + meropenem
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |