Playlist
Show Playlist
Hide Playlist
Autoimmune Hemolytic Anemia
-
Slides Autoimmune Disease.pdf
-
Reference List Immune System.pdf
-
Download Lecture Overview
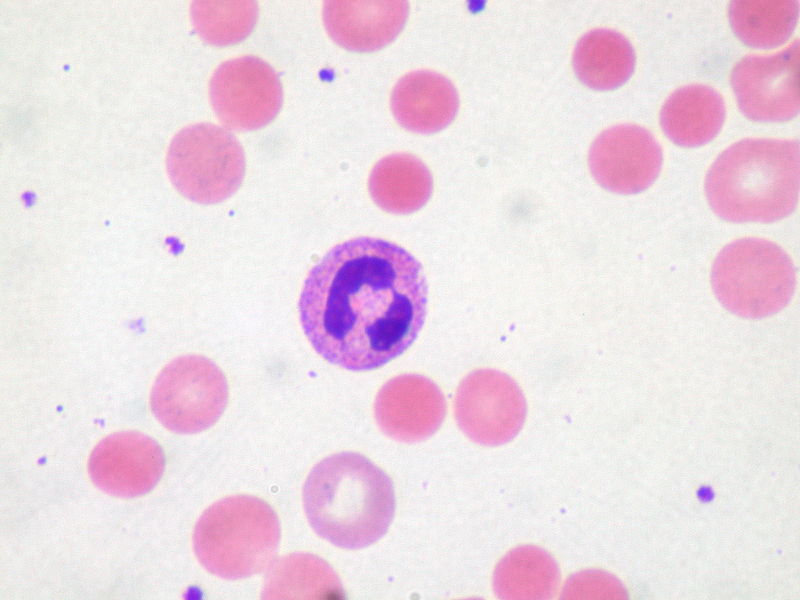
00:01 Looking at autoimmune hemolytic anemia, one can identify two types of autoantibody. 00:10 The cold antibodies are anti red blood cell autoantibodies that only bind at significantly below normal body temperature. 00:20 And therefore the extremities are particularly affected. 00:24 These antibodies are usually of the IgM class. 00:28 In contrast, the warm type antibodies found in autoimmune hemolytic anemia are anti red blood cell autoantibodies that bind at normal body temperatures. 00:39 And these are usually of the IgG class. 00:44 Following binding of IgM or IgG autoantibodies to the surface of the red blood cells, the classical pathway of complement can become activated leading to the generation of the membrane attack complex. 01:01 This will cause lysis of the red blood cells. 01:07 In addition, phagocytic cells with Fc receptors on their cell surface can take up erythrocytes that have been coated with antibody, and this again will lead to the destruction of those red blood cells. 01:26 One can test for the presence of these autoantibodies using a test called the Coombs test. 01:32 And there are two different versions of this test. 01:36 In the direct test, one takes a blood sample from the patient and looks for the presence of autoantibodies that are already coating the red blood cells. 01:50 And one detects the presence of these autoantibodies that have already coated the red blood cells, using a second antibody - an anti-human immunoglobulin. 02:02 This will cross link together the antibodies on the surface of the red blood cells causing agglutination which can be visualized by the eye. 02:15 In the indirect test, one looks for the presence of the autoantibody itself, free autoantibody that is not bound to the erythrocytes. 02:27 One can take this antibody from the serum of patients, mix it with red blood cells. 02:34 And if the autoantibody has specificity for red blood cells, this anti red blood cell autoantibody will bind to the red blood cells. 02:43 And this autoantibody can then again be detected by using a second antibody, an anti-human immunoglobulin. 02:51 So this is the indirect Coombs test. 02:54 And again, upon adding the anti-human immunoglobulin, there will be agglutination which can be visualized by simply looking at the slide on which this test is being carried out. 03:05 In pernicious anemia, there is a autoimmune attack that prevents the absorption of vitamin B12 from the gut. 03:17 So in the normal individual, ingested vitamin B12 is picked up by intrinsic factor in the stomach. 03:26 And this complex of vitamin B12 bound to intrinsic factor is then absorbed from the gut and can be used in the development of red blood cells. 03:39 However in pernicious anemia, there are autoantibodies being produced. 03:45 One of those autoantibodies is against the parietal cell H+ K+ ATPase. 03:53 This leads to a reduced production of intrinsic factor. 03:58 And there are also autoantibodies against intrinsic factor itself. 04:03 This means that vitamin B12 is not absorbed from the gut resulting in anemia. 04:10 In autoimmune thrombocytopenic purpura, platelets are affected. 04:17 There are autoantibodies to the platelet glycoproteins GPIIb-IIIa and GPIb-IX. 04:28 These are removed and destroyed by splenic macrophages and liver Kupffer cells. 04:35 So following binding of these autoantibodies to the platelets, the complex of the autoantibody together with the platelet is recognized by Fc gamma receptors on the surface of these phagocytic cells and the platelets are destroyed, resulting in autoimmune thrombocytopenic purpura.
About the Lecture
The lecture Autoimmune Hemolytic Anemia by Peter Delves, PhD is from the course Hypersensitivity and Autoimmune Disease. It contains the following chapters:
- Autoimmune Hemolytic Anemia
- Pernicious Anemia
- Autoimmune Thrombocytopenic Purpura
Included Quiz Questions
Which of the following classes of immunoglobulins (Ig) is the usual cause of ‘cold’ antibodies?
- IgM
- IgG
- IgA
- IgD
- IgE
A direct Coombs test detects which of the following?
- Antibodies on the surface of the red blood cell
- Damaged red blood cells
- Free autoantibodies in the serum
- Red blood cell self-antigens
- Transfused red blood cell antigens
Which of the following auto-antibodies is most likely present in someone suffering from pernicious anemia?
- Parietal cell antibodies
- Anti-Ro
- Anti-tissue transglutaminase
- Endomysial antibodies
- Antiphospholipid antibodies
Which of the following glycoproteins is most commonly affected in autoimmune thrombocytopenic purpura?
- IIb-IIIa
- Envelope glycoprotein GP120
- Laminin
- x-IIb
- Fibronectin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |