Playlist
Show Playlist
Hide Playlist
Atrophy and Autophagy
-
Slides Cellular Pathology Adaptation to Injury.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
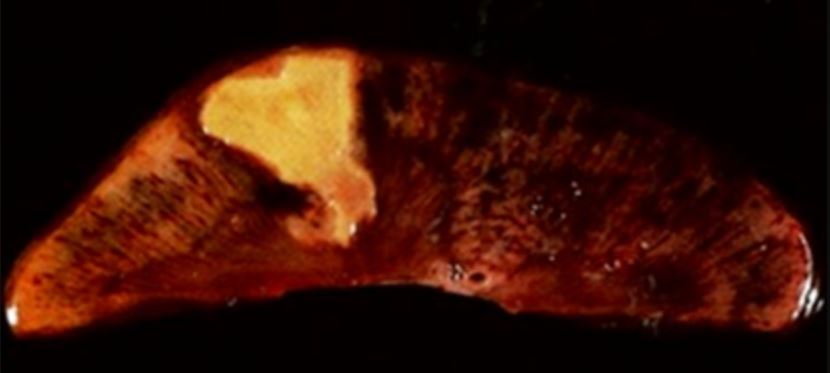
00:00 So, Atrophy, is nothing more than a decrease in cell size, as a result, the organ will decrease in size, too. 00:08 So if we look at a normal muscle on the right, we have a certain size of the individual skeletal myocytes, and that gives the muscle a certain appearance. 00:20 In the atrophy muscle, we actually haven't lost any cells. 00:23 Just each cell has become that much smaller, so just cell size will impact organ size, clearly. 00:33 The cells are smaller because they've kind of retreated to a less metabolically active state. 00:38 They're still viable, and it's potentially reversible. 00:41 If we restore blood fold, we restore mechanical activity, that atrophy muscle will come back. 00:46 And those of you who may have had a broken arm at some point know that as you were in a sling and not using that arm, you had atrophy of the muscle. 00:54 And when you took it out of the swing, you thought, Oh my God, I've lost my muscle. Well, no, it's still there. 00:59 It comes back when you use it, so that's disuse atrophy of the skeletal muscle. 01:05 Also, the same thing will happen, if we withdraw hormonal stimulation. 01:10 So we will see an example, in a minute, where you will have increased estrogen and progesterone, causing increase of smooth muscle mass in a gravit, a pregnant uterus. 01:25 And after the pregnancy, we withdraw those at hormonal stimulus and the uterus returns to normal. 01:32 So, withdraw of hormone stimulation can also give rise to atrophy or to restoration of normalcy. 01:42 It's important to note, too. 01:43 We can also get smaller organs if we have fewer cells. 01:48 So the atrophy that occurs, say, in a brain with Alzheimer's disease, there is significant loss of the the neuronal network, and that's actually because neurons have died. 02:00 As a result, we get atrophy of the organ. 02:03 So we need to distinguish, just briefly and in our own minds, when we talk about atrophy of a cell, versus atrophy of an organ. 02:12 And you can have atrophy of an organ due to individual cells getting smaller, you can have atrophy of an organ by having fewer cells. 02:21 All right, how does this happen? How do we get atrophy? Well, in fact, there a couple different mechanisms, and we're gonna discuss those very briefly. 02:29 One is Proteasome Degradation. 02:31 In a previous talk, when we talked about subcellular mechanisms of degradation, a breaking down small things. 02:39 We talked in detail about proteasome degradation of proteins. 02:43 And we have a process by which we identify a protein is something that should be targeted for destruction. 02:48 You see the target protein in the right lower corner. 02:53 We are going to load up some E ligases, E1, E2 and E3 ligases, and there are a whole bunch of these and they are going to transfer ubiquitin, the green bubble to the target protein, and put multiple ubiquitins on that protein. 03:09 And that's a label, it says, I need to be broken down. 03:13 So we can have proteasome degradation of proteins. 03:17 Once we've targeted the protein for degradation, it goes into the proteasome, whole bunch of these little miniature garbage disposals that are inside the cytosol, and we break down the big protein into little tiny peptides that subsequently get broken down into constituent amino acids. 03:33 So proteasome catabolism is a way to turn over. 03:36 We can activate this pathway. 03:39 If we need more proteins, or we need more constituents and we will break down those proteins causing atrophy. 03:49 A proteasome catabolism may involve ubiquitin targeting increasingly recognize that there are other pathways that don't involve ubiquitin. 03:56 But for the most part it's mostly through that targeting, and maybe increased in hypercatabolic states and contribute to atrophy. 04:04 Clearly, we're getting increased protein turnover by having them all break down through the proteasome. 04:10 So that's one mechanism by which we can get atrophy. 04:13 We can also get it through breakdown using the lysosomes. 04:17 That's normal cell metabolism through Heterophagy. 04:21 So it is eating of other stuff hetero.</b> So that's one way that we have lysosomal catabolism, that's the normal mechanisms by which we take up a variety of large things. 04:34 You can also have, as we've discussed previously, autophagy, so eating self-constituents. 04:41 This is actually a normal pathway for normal cellular metabolism and normal cell and organelle are turnover. 04:49 As we've discussed many times, the cells are constantly turning over, large protein aggregates, constantly turning over. 04:55 In order to degrade those we have to, those are big things. 04:59 Mitochondria are big things. 05:01 We need to identify them as being old, and then we break them down, using the autophagic or autophagy pathway, that involves encasing them into a membrane, the autophagosome, fusing it with lysosomes that contain various hydrolases. 05:18 And then we degrade everything that's in there and release it as the constituent lipids in amino acids, ect. 05:26 This pathway can be up regulated. 05:29 If we need to or up regulated in hypercatabolic states and lead to atrophy. 05:36 So autophagy, mainly used for throw over of long lived proteins and organelles, and we've talked about this many times. 05:43 What's being shown on the right hand side is electron micrograph of an autophagic vesicle, that has ensnared a senescent mitochondria and the typical autophagic vesicles, it doubled-layered membrane. 05:56 It derives from the rough endoplasmic reticulum. 06:00 We can clear damage constituents, including protein aggregates that have occurred. 06:05 If the cell is starving, it will maintain its viability by eating itself and getting down to a shrunken version that's still alive and hanging in there. 06:17 It does so through autophagy. 06:20 Interestingly enough, it's also potentially mechanism against intracellular pathogens. 06:25 So we can use the same pathway, say a bacteria, an intracellular bacteria or a virus gets into a cell, we recognize it is foreign. 06:33 We can encase it, in an autophagic vesicles and degrade it. 06:38 So it is a defense against intracellular pathogens. 06:42 It may be a mechanism by which tumors resist therapy, so it's not just important that we understand it in the context of atrophy. 06:50 But tumors... 06:51 under attack may hunker down, and say, you know what? I'm not gonna have any metabolic activity. 06:56 I'm just going to kind of eat myself here. 06:59 I'm gonna hang out in a small inactive form and wait for that nasty chemotherapy to go away and then I'll be able to come back. 07:06 So tumor resistance to therapy has actually also been related to autophagy. 07:11 It can also be too aggressive, so every now and then, actually more than every now and then, cells will do too much of this and they eat too many mitochondria, and there's not enough left to even maintain viability, and as a result of that, it can be a mechanism of cell death. 07:27 So autophagy and proteasome catabolism is a way by which we can break down salary constituents and make smaller and smaller and smaller cells. 07:35 And the cells get smaller and smaller, the whole tissue atrophies. 07:39 So that's our mechanisms for getting atrophy. 07:43 Let's get a little bit more in detail on autophagy because it's important to understand for some metabolism and some biochemistry that you're going to see as part of your medical career. 07:52 And also because it has an impact on certain drugs that we will give our patients. 07:58 So autophagy, it happens as we identify organelles that are senescent. 08:05 Again the mechanism by which this happens, not entirely clear. 08:09 We surround them with a membrane that's derived from them rough endoplasmic reticulum, that's our phagaphore. 08:16 We then take that phagaphore, the autophagasome now, that has trapped up senescent things that we want to get rid of and we take from the cytosol, LC3B, these are proteins that are kind of like ubiquitin, you can think of them as ubiquitin. 08:32 But it's basically labeling this autophagasome says, you know what? I've got stuff in here that needs to be degraded. 08:39 That is its signal for the lysosome to come along, fuse with it. 08:44 The LC3B gets recycled for the next round with another autophagasome someplace, and the lysosome dumps in its hydrolases and degrades everything that's inside the autophagasome. 08:56 And we get degradation, we get amino acids coming out, fatty acids, all of that other stuff. 09:02 So that's the normal pathway. 09:04 This is actually very tightly regulated in most cells. 09:07 So there are a number of genes, they're called Atg genes for autophagy, genes, Atg, good name. 09:13 And those products target organelles for the new ritual nucleation. 09:17 And there are, I think, eight different Atg genes and protein products that will control this process. 09:26 Okay, that's all well and good. 09:27 What does this have to do with you? Well, in fact, there is a major regulator in cells that you need to be aware of because it's a very important kind of linchpin in biochemistry is the mammalian target of rapamycin, or mTOR. 09:43 And mTOR levels, very carefully regulate the transcription and translation of Atg genes. 09:51 So the more mTOR we have, the less atrophy that we will have. 09:59 It's basically turning off this process. 10:05 So what controls mTOR? Well mTOR, things like insulin and amino acids and other gene products that say, you know what? We are in Fat City. 10:16 We've got all the nutrients we need and more, they will act on. 10:21 They will up regulate mTOR, which will then inhibit Atg. 10:25 And we'll turn off all this autophagy stuff. 10:29 Cool. 10:29 So this, in fact, this is biochemistry coming back to pathology, and it's a nice kind of intersection. 10:34 There's a drug that we give very frequently for immune suppressing patients who have had organ transplants, and that's rapamycin. 10:43 And rapamycin will inhibit mTOR. 10:47 So, it also inhibits other processes that are involved in the immune response, that's why we give it for treating patients who have received an organ transplant. 10:57 But that rapamycin inhibits mTOR. 11:00 If we're inhibiting mTOR that means we're not inhibiting Atg genes. 11:05 And now we're getting more autophagy. 11:08 So in fact, when we give patients rapamycin, we actually induce muscle, skeletal muscle, atrophy through this pathway. 11:16 Just a consequence. 11:17 So every drug has its target. 11:20 But it also has unintended targets as well, just a good example of that.
About the Lecture
The lecture Atrophy and Autophagy by Richard Mitchell, MD, PhD is from the course Cellular Injury.
Included Quiz Questions
Atrophy is...?
- ...a decrease in cell size.
- ...a reduction in cell number.
- ...the transformation of one differentiated cell type into another differentiated cell type.
- ...an increase in cell number.
- ...the replacement of normal parenchymal tissue by connective tissue.
Autophagy plays an important role in which of the following processes?
- Defense against intracellular pathogens
- Degrading extracellular molecules taken in by the cell through endocytosis
- Defense against cancer cells
- Synthesis of glycogen and long-chain fatty acids
- Packaging proteins destined to be exported from the cell
What role does mTOR play in autophagy regulation?
- Inhibition of the Atg gene products
- Inhibition of the LC3B proteins
- Labeling autophagosomes for degradation
- Activation of the Akt protein
- Activation of the starvation signaling pathways
Which of the following upregulates the mTOR signaling pathway?
- Insulin
- Starvation
- Stress
- Rapamycin
- Adenosine monophosphate
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
2 customer reviews without text
2 user review without text