Playlist
Show Playlist
Hide Playlist
Atherosclerosis: Pathogenesis
-
Slides 01 VascularMedicine advanced.pdf
-
Reference List Vascular Medicine.pdf
-
Download Lecture Overview
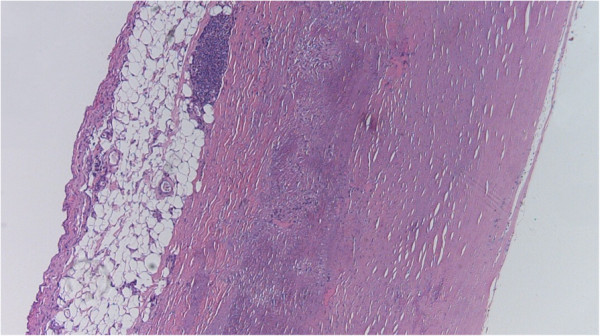
00:01 Let's talk about pathogenesis—that is, the abnormal physiology and anatomy that goes in along with this disease. So here, we see a little cartoon showing you one of these early atherosclerotic plaques that can occur even in children or in young adults and develop, eventually, into big, thick inflammatory atherosclerotic plaques. You can see that there is a thickening of the endothelial layer. You can see that there's also development of scar tissue with a necrotic core, with dead cells in the center. And these dead cells often contain lipids—that is, LDL cholesterol—that macrophages (which are a defense cell in the bloodstream, a white cell) have come to try and capture and dissolve. Unfortunately, they don't dissolve it, and in fact, what it does is it kills these macrophages, and that just increases the inflammatory process—the scar tissuing—and increases the size of the atherosclerotic lesion. 01:09 You can see that there's a fibrous cap overlying this. When the fibrous cap is thick, the lumen, or the channel of the artery, gets smaller, but it doesn't rupture. When the fibrous cap on top is very thin, it can rupture, blood clot can form, and the artery can actually occlude totally, resulting in infarction or necrosis (death of tissue) downstream. And you see, in this little cartoon, you can see that the materials that are in the fibrous cap, the infiltrating macrophages and also lymphocytes that are drawn in by the inflammation. 01:47 And you can see that the epithelium on the surface is still intact, but if the fibrous layer (as I said before) is thin, that can rupture, and a blood clot can form that can cause infarction, or death of tissue, from no blood flow getting through the obstruction. 02:06 So atherosclerosis usually starts as mild. The endothelium (the thin layer on… in… that's right on… next to the channel of the artery) gets damaged. Factors such as high blood pressure and cigarette smoke damage the endothelium, and this allows the LDL cholesterol—often, the oxidized form—to get underneath and into the wall of the artery, where it starts the inflammatory process. One advances to moderate atherosclerosis, where the inflammatory response, the white cells coming in, trying to ingest the LDL cholesterol, dying, forming a great stimulus to scar tissue formation and further arrival of LDL cholesterol in the area. Finally, in the healing process, calcium salts can occur, and actually, the artery can become rock-hard for… almost with bone formation and, of course, lots of scar tissue. The artery loses elasticity, the channel narrows, and blood flow is impaired. In the most severe form, there is severe restriction of blood flow through the artery. Often, this can lead… this can make high blood pressure even worse, and the, of course, increase in the blood pressure can promote formation of more plaques. 03:25 And eventually it's even possible for an area where the plaque ruptures and a blood clot forms and the artery is totally obstructed. And that's what happens in a heart attack, or a myocardial infarction. Here, we see three examples. You can see mild atherosclerosis in the top, moderate in the middle, and very severe at the bottom. The bottom one has lots of calcification, lots of scar tissue. You can also see the yellow color; that's from the deposition of cholesterol in the artery wall. 03:58 There are also sudden occlusions of the artery. As I mentioned, it can happen when a plaque ruptures, but it can also happen when there is an embolus—that is, a blood clot that forms somewhere in the heart. And I gave examples, during the basic lecture, of blood clots forming in the left atrium during atrial fibrillation. Blood clots can also form on prosthetic, or plastic and steel, heart valves. Sometimes, in a rare circumstance, fat can actually get into the bloodstream and embolize. Or air—particularly during procedures or during some sort of trauma—air can get in. And when any of those things block an artery, no blood flow gets through, and there is necrosis, or death of tissue. Remember the term thrombus? That's a blood clot that forms on a vessel wall: could be in the venous side, can be on the arterial side, can be in the left atrium. And when that thrombus breaks off and flows in the bloodstream and causes mischief somewhere downstream, it's called an embolus. The diagnosis is made because of signs of restricted blood flow in an area. For example, if there had been a blood clot in the left atrium that suddenly went to the brain, the patient would have sudden symptoms of a stroke. The therapy is aimed at restoring blood flow. It can be done by removing the clot, either surgically or with catheters or by giving so-called clot busters, or drugs that dissolve the blood clot.
About the Lecture
The lecture Atherosclerosis: Pathogenesis by Joseph Alpert, MD is from the course Arterial Diseases.
Included Quiz Questions
What is the leading cause of death in the world?
- Cardiovascular disease
- Alzheimer's disease
- HIV/AIDS
- Trauma
Which of the following immune cells can be found engulfing lipid molecules in an atherosclerotic plaque?
- Macrophages.
- Neutrophils.
- Lymphocytes.
- B-lymphocytes.
- T-killer cells.
Which of the following best describes an embolus?
- A free moving blood clot
- A blood clot on a prosthetic valve
- A blood clot on an arterial wall
- A blood clot in the venous system
- An occluding thrombus
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
2 customer reviews without text
2 user review without text