Playlist
Show Playlist
Hide Playlist
Antiplatelets
-
Slides Antiplatelets.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
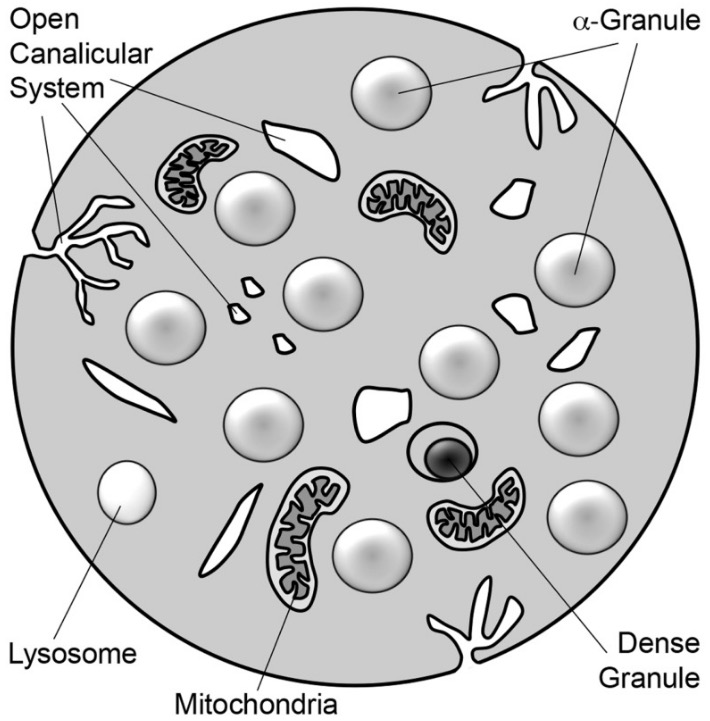
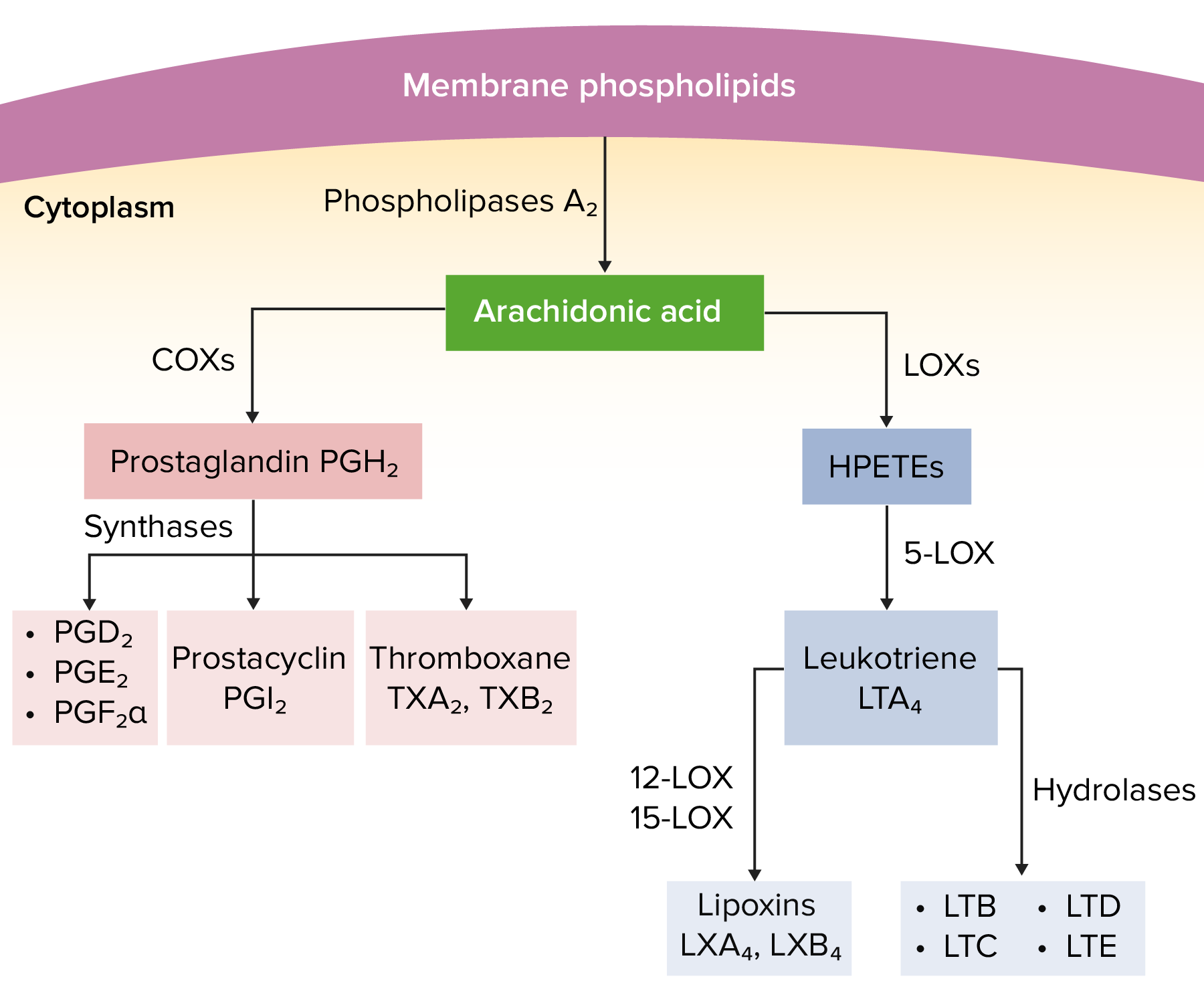
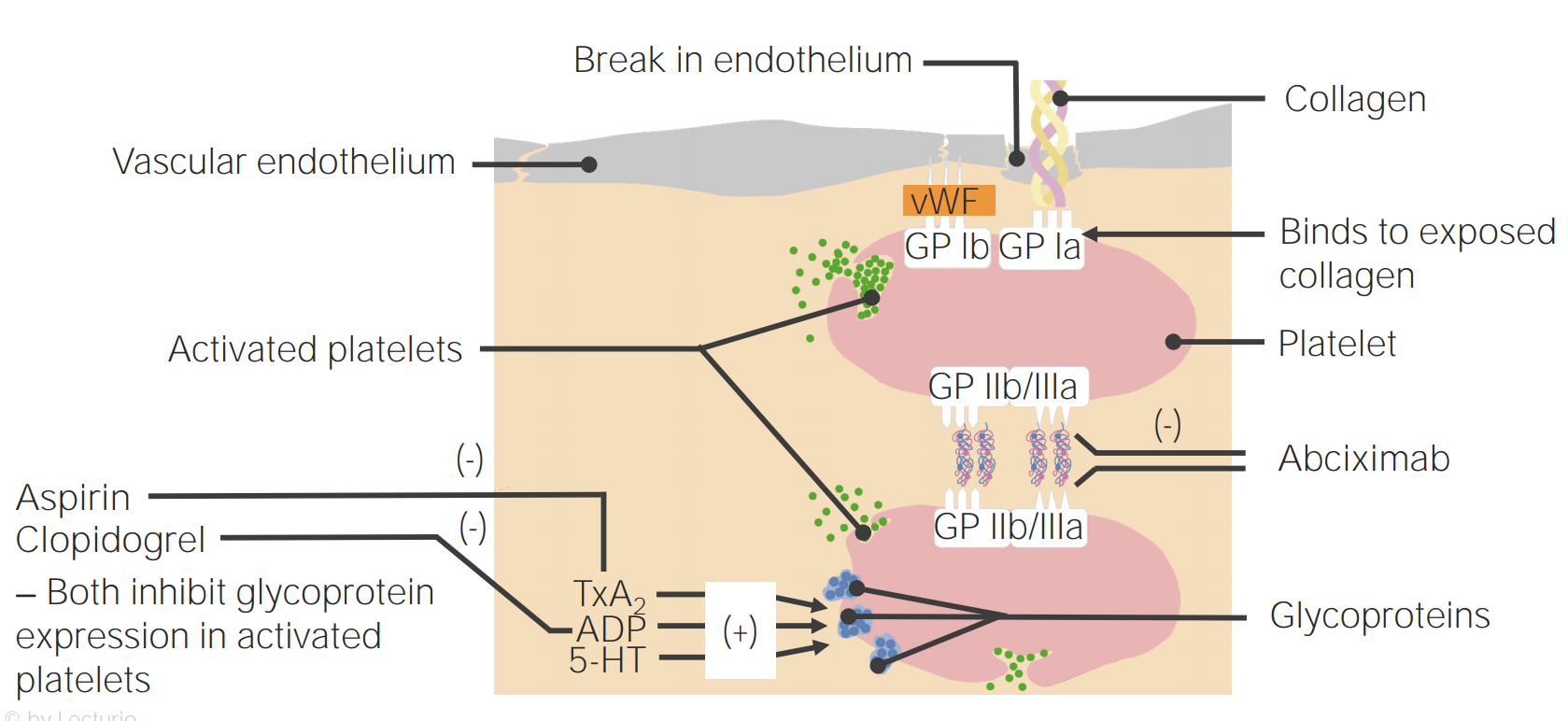
00:01 Let's start off, with looking at a platelet. 00:04 So, a platelet is a very important part of the blood clot, it's like the brick in a wall, and platelets, if they don't adhere to each other, aren't going to form very good clots for us. 00:14 So, the GPIIB/IIIa molecule is central, to the function of a platelet. 00:20 You can see here, I have a picture of a platelet next to me, and you can see in blue, the GPIIB/IIIa molecule, which is also called the αIIb/βIII molecule in Europe, allows that platelet to adhere to the collagen substrate, of any particular tissue. 00:38 The other thing that this GPIIB/IIIa molecule allows us to do, is adhere to other platelets, so, you can see that there's another platelet attaching to the first platelet, through fibrinogen. 00:49 This cross-linking and activation of platelet adhesion and aggregation, are important components of the GPIIB/IIIa molecule. 00:58 The third component of platelet function is, its release function. 01:03 Now, thromboxane A2, plays a very important component in the release function, ADP is released when platelets bind to damaged tissue, and ADP is another important component in platelet function. 01:16 This brings us to our first drug, “Aspirin.” Aspirin is an irreversible inhibitor of cyclooxygenase, it is used to manufacture thromboxane A2, and platelets, when you inhibit cyclooxygenase with aspirin, actually, are permanently inhibited. 01:33 That means, that the anti-platelet function of aspirin, is going to last for the entire life of this platelet, and that means, that only replacement platelets will be functional, and that means, that the aspirin effect is going to last anywhere, between three and seven days. 01:49 Interactions of aspirin are very important, because the aspirin is going to interact with, non-steroidal anti-inflammatory pain agents. 01:58 They impair platelet function on their own, and when combined with aspirin, you actually have an enhanced anti-platelet effect. 02:08 The next group of drugs that I want to talk about are the GPIIB/IIIa inhibitors, we've already spoken about GPIIB/IIIa before, and we've illustrated how important it is in platelet adhesion and aggregation. 02:22 So, we have reduced adhesion with the IIB/IIIa inhibitors, and we have reduced platelet aggregation. 02:28 These are the drugs that are commonly used in this drug class, you don't need to know them so much, as you need to know that they're used in the cath lab, to inhibit platelet aggregation, after catheterization. 02:40 The ADP inhibitors are another drug class, you need to know this, for your exam. 02:45 So, pay close attention. 02:46 Clopidogrel and prasugrel are the two drugs that we're using right now, in clinical practice. 02:53 They require hepatic conversion to be active, so, they don't act right away, they take some time to actually work, they are also irreversibly inhibitive of platelet function. 03:04 Ticagrelor or Brilinta, is a very commonly used drug in the cath lab, it does not require hepatic activation, and it is a reversible inhibitor of ADP receptors. 03:15 So, ticagrelor is a reversible inhibitor, clopidogrel and prasugrel, are not reversible, they are irreversible drugs. 03:25 It's really important, I want you to remember the distinction between the two, because guaranteed, I'm going to put it on an exam. 03:33 Let's talk about the next class of drugs. 03:36 Dipyridamole is a very commonly used agent, that has a dual mechanism of action, the first action is that it inhibits phosphodiesterase, that reduces cyclic AMP mediated degradation, and cyclic AMP is an inhibitor of platelet aggregation, so, there's a double negative there, pay attention, more cyclic AMP means less platelet aggregation, so, in other words these drugs inhibit platelet aggregation. 04:03 The second effect of this class of drugs is that it inhibits the uptake of adenosine, so, it increases your plasma concentration of adenosine, adenosine acts through that A2 receptor on the platelet surface, and the A2 receptor activation causes increases in plasma cyclic AMP levels, once again, more cyclic AMP, means less platelet aggregation, so, we have less platelet aggregation through adenosine-mediated action. 04:30 So, this brings us to the actual uses in clinical practice. 04:34 Aspirin is the most commonly used antiplatelet that we have, it reduces heart attacks, an aspirin a day keeps the cardiologist away. 04:42 It also reduces stroke, so, we use it all the time in preventing stroke activity, and it reduces peripheral arterial ischemia. 04:49 So, the three areas are: Heart, brain and the legs, our peripheral arterial supply. 04:55 The American College of Cardiology and the American Heart Association guidelines recommend that low-dose aspirin should not be given on a routine basis for primary prevention of cardiovascular disease in those over 70 years of age, or among adults of any age who are at increased risk of bleeding. 05:14 The direct inhibitors also prevent restenosis after angioplasty, it's used in acute coronary syndrome. 05:22 We spoke about clopidogrel, remember that it's an irreversible inhibitor, it prevents TIA’s or mini strokes, it prevents strokes, and it reduces restenosis of stents, so, a lot of time we will use clopidogrel or prasugrel, for about a year, after we put in a drug-eluting stent. 05:41 Dipyridamole is often used in combination, we sometimes use this as in combination with aspirin, for secondary prevention of stroke. 05:49 So, the thing that you want to remember is that, if a person has a stroke, we give them aspirin, if a person on aspirin, has a stroke, we give them aspirin + dipyridamole, or we switch them to one of the other drugs, and finally, cilostazol is used to treat intermittent claudication. 06:08 In terms of the toxicity of these drugs, they're not insignificant, so, aspirin has a bleeding of rate of about 0.3% or 3 per 1000. 06:19 Ticlopidine has a bleeding rate of about 5%, but a 1% rate of severe neutropenia. 06:26 Ticlopidine is a drug that you only need to know, because we don't use it anymore. 06:31 So, thrombocytopenic thrombotic purpura, is a rare complication, severe neutropenia is a common complication at 1%, On your exams they're going to talk about the side effects of this drug, but in real world clinical practice, we don't use this drug anymore. 06:49 We spoke a bit about the direct inhibitors, the side effects of course are bleeding and thrombocytopenia with chronic use, we only use these drugs short term, so, it's not as much of an issue with it. 07:00 Clopidogrel the bleeding rate is less than 1%, it is certainly present, and when you combine clopidogrel and aspirin together, the bleeding rate increases. 07:13 Dipyridamole is that adjunctive drug that we were talking about, it adds between 1-2% bleeding risk to your drug, that already has a bleeding risk. 07:22 And then in terms of the peripheral drugs, they are contraindicated in heart failure. 07:29 This is going to be on your exams, know this. 07:31 This particular drug it is contraindicated in heart failure.
About the Lecture
The lecture Antiplatelets by Pravin Shukle, MD is from the course Pharmacology of Blood Coagulation. It contains the following chapters:
- Antiplatelets: Looking at a Platelet
- Antiplatelets: Aspirin
- Antiplatelets: Glycoprotein Inhibitors
- Antiplatelets: ADP Inhibitors
- Antiplatelets: PDE/Adenosine Uptake Inhibitors
- Antiplatelets: Uses
- Antiplatelets: Toxicity
Included Quiz Questions
When platelets bind damaged tissue, they release a substance responsible for augmenting platelet aggregation. What substance (along with thromboxane A2) is released?
- Adenosine diphosphate (ADP)
- GPIIb/IIIa
- Alpha granule
- Dense granule
- Fibrinogen
Which anti-platelet drug is contraindicated in heart failure?
- Cilostazol (Pletal)
- Dipyridamole (Persantine)
- Aspirin
- Eptifibatide (Integrilin)
- Clopidogrel (Plavix)
How long does the anti-platelet function of aspirin last?
- 3 - 7 days
- 3 -7 hours
- 3 - 7 weeks
- 1 day
- 14 days
Which change is likely with the administration of dipyridamole (Persantine)?
- All changes listed are likely.
- Increase in platelet cAMP levels
- Inhibition of phosphodiesterase
- Inhibition of adenosine deaminase
- Inhibition of the cellular reuptake of adenosine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Really good and concise. You will really learn a lot.