Playlist
Show Playlist
Hide Playlist
Antimalarial Drugs – Antiprotozoal Agents
-
Slides Antimalarial Drugs Antiprotozoal Agents.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
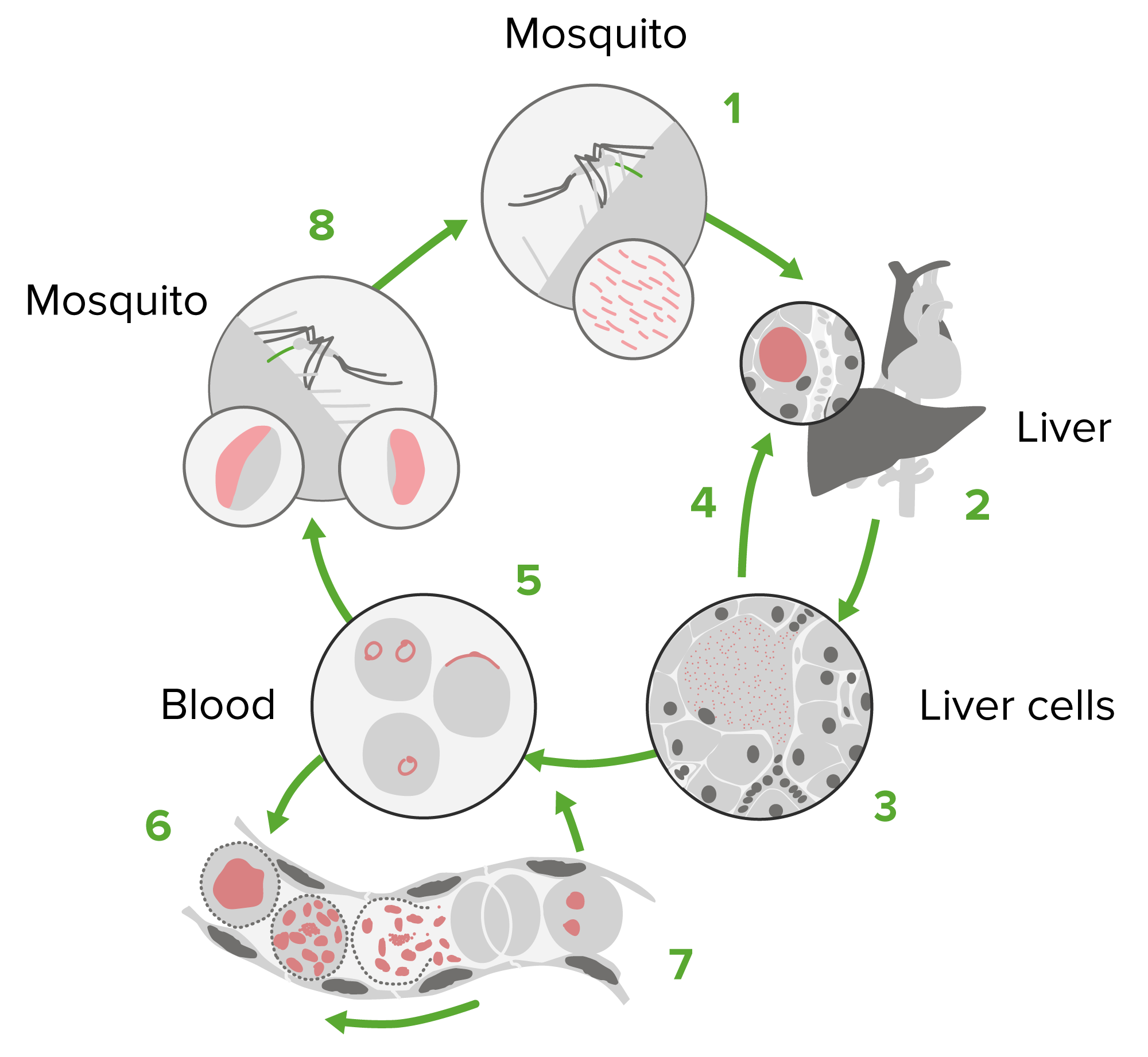
00:01 Welcome to pharmacology by Lecturio. I'm Dr. Pravin Shukle. We're going to be covering antiparasitic agents. 00:08 If you've been doing the lectures in order you will know that this is the last of the series. Congratulations on making it this far. In todays lecture we're going to be covering the agents that are used against the parasites commonly affecting patients. We're going to be talking about antimalarial agents and amebicides. We're going to be talking about those agents that works against nematodes and trematodes and cestodes. Let's start off with antimalarial agents. The most well known of the antimalarial agents is chloroquine. It was one of the first ones developed and it's still used in many countries today. Now chloroquine prevents the polymerization of heme. 00:50 which is produced when the parasite digests hemoglobin in red blood cells. Free heme inside the parasite is toxic so it normally polymerizes it into a non-toxic form called hemozoin. We do have resistance developing in many malarial strains today. Malaria organisms develop membrane transporters that actually will eject the intracellular heme. Plasmodium falciparum or P.falciparum can also develop a transporter for the chloroquine itself, which is actually quite shocking when you think about a organism actually being able to eject a drug specifically because it's toxic. Now the agent that is responsible or the gene that is responsible for the ejection protein for chloroquine is called the pfcrt gene. Side effects associated with chloroquine are usually GI disturbances. And you're going to notice that will be a general theme throughout the entire antimalarial agent lecture. Nausea, cramping, and diarrhea. You may also see some skin rashes and headaches as well. Although these are a little bit less common. At very high doses of chloroquine, we'll see severe skin reactions and we may also see peripheral neuropathies. Some patients may also develop a toxic psychosis and may also develop retinal and auditory damage. At very high doses of chloroquine we actually can see myocardial depression. And this is usually in cases of overdose. We may also precipitate porphyria attacks because remember heme is an integral part of the porphyria metabolism system. And by altering the levels of heme in the blood you can cause porphyria attack through chloroquine. Another agent or another set of agents that we talk about with respect to antimalarial treatment are those agents that are derived from artemisinin. Now, who is Artemis? Artemis was the Greek goddess of the hunt and you can see her portrayed here. She was fabled to always favor this one particular plant, and whenever she would lay down, she would lay down in this particular bed of plants, because it was particularly soft. That interesting little side note just gives us an idea of where the name comes from. And you can see that all of the names of the drugs are derived from her name. Now the mechanism of action of these drugs is that they accumulate in the food vacuoles of the parasites themselves. They form toxic free radicals. They will work against multidrug resistant strains of malaria. And so we often see them used in combination with other agents. There are rare adverse side effects of nausea, vomiting and diarrhea with these agents. Much less than, say chloroquine. 03:42 There is no increase in congenital abnormalities or stillbirths in women taking these medications. So we feel that they may be quite safe in pregnancy. Another agent that has commonly been used to treat malaria is quinine. In fact it's the oldest of the agents. It combines with double stranded DNA and prevents the strand separation from occuring. That's how they work in the blood schizont. They block replication and transcription of DNA. And it's used in chloroquine resistant Plasmodium falciparum infections as well. We're often combining this particular agent with doxycycline or clindamycin in order to shorten the duration of therapy and also limit the toxicity of all of the agents. The toxicity of quinine, it seems rather obvious and we touched on it to some extent in our cardiology lecture. You'll sometimes get cinchonism or gastrointestinal distress, headache, vertigo, blurred vision and tinnitus. Hemolysis is quite common in patients who have glucose-6-phosphatase deficiency. So it's a very important consideration and something you have to be very aware of, that you don't want to be using quinine in these patients. This is a particular problem in your East Indian patient population cause a lot of East Indians are deficient in glucose-6-phosphatase deficiency. And when they will travel from the United States back to India to visit relatives, you have to be very aware that you may not want to give these patients quinine. Blackwater fever is a special kind of a fever that involves intravascular hemolysis. It's something that we have to be particularly aware of in patients who are on quinine. Mefloquine is probably the most used antimalarial agent in patients from North America who are travelling abroad. It's chemically related to quinine and it's often considered our first line agent. 05:40 Generally speaking, for prophylaxis we give the patient four weeks of therapy prior to, and one week after with one pill once a week during the treatment. So for example, if you're travelling to say, an endemic area that's susceptible to mefloquine for three weeks, you would take it for four weeks before; once a week. During the three weeks while you're travelling; once a week. And then for one week after. Now how this particular agent work is that it creates more toxic heme particles in the food vacoules of the malaria strain. And it's quite effective in killing the malaria schizont. We classify it as a blood schizonticide because it kills that schizont form in the red blood cells. Toxicity includes GI distress, skin rash, headache, and dizziness. Nightmares is actually surprisingly common. And in children who are on mefloquine, it's exceedingly common. I myself saw it happen in my son who developed nightmares and parasitosis; the fear of being eaten up by parasites while he was taking mefloquine on a recent trip to Peru. So it's a very real problem and it's something that sometimes limits our ability to use this medication. These agents may also cause cardiac conduction defects, and seizures at very high doses. Primaquine is another tissue schizonticide and it's also a gametocide. So it actually kills the gamete form of malaria. It eliminates liver stages of P.vivax and P.ovale as well. It's used in conjunction with a blood schizont agent so that we can really do a good kill job with respect to malaria. Now how it works is that it forms quinoline and quinone metabolites that acts as oxidants for these agents, for the schizont. So that it actually becomes toxic and makes a toxic environment for both the schizont and the gamete. In terms of toxicity of primaquine, most of the patients who complain of symptoms will complain of GI distress. Most often abdominal cramping and a sense of fullness. Some patients may also develop headaches while they're on this medication. Something you have to be very aware of is you can cause methemoglobinemia. And also in patients who have glucose-6-phosphatase deficiency, you have to be aware that you can precipitate a hemolysis in this patients. With primaquine, it is contraindicated in pregnancy. We have a whole group of antifolate drugs that we use. We use them predominantly as schizonticides. Proguanil, pyrimethamine, sulfadoxine, dapsone. These are all agents that are combined in various ways to give a synergistic effect through sequential blockade and causing an antimetabolic effect which will block the folic acid synthesis within the malaria organism. Toxicity causes, it causes skin rash, and can cause gastrointestinal distress. And once again, any antimetabolite drug will be contraindicated in pregnancy. Doxycycline is also used. It's used for chemoprophylaxis for travellers through an unknown mechanism. And despite the fact that it seems like a fairly prosaic drug it's actually shockingly effective. So it's something that you should consider in your patients who can't take one of the other agents. Amodiaquine is also another agent that we use for the treatment of malaria. It's a relatively cheap drug. We use it extensively in the third world settings. It's used in fixing dosing with artesunate, which is one of those artemesinin drugs that we had talked about earlier. Toxicity includes hematological problems including agranulocytosis and aplastic anemia. So be aware that these agents can cause problems with your white count and the development of white blood cells lines. Atovaquone is another agent that we use for the prevention and treatment of malaria. We consider this an erythrocide agent. Now Malarone is atovaquone plus proguanil. It's a very very commonly sold pill in the United States. It's used as treatment and as once daily prophylaxis It is an alternative treatment for patients who have Pneumocystis jiroveci infection. Mechanism of action, we know that it acts on the mitochondrial electron transport system to somehow cause death inside the cell of the malaria organism. We're not sure much more beyond that. There are lots of interesting articles that are coming out now in the literature, taking a look at how this particular agent works. In terms of toxicity, abdominal pains and GI side effects are very common with this particular agent. Halofantrine is another erythrocide agent that are active against all erythrocytic forms of all 4 malaria strains. It is not at this point used as a chemoprophylactic agent because it has a high potential for cardiotoxicity and a prolonged QT interval. It is also contraindicated in pregnancy because it is toxic to the embryo. In terms of prevention of malaria, you should always consult local guidelines because the malaria guidelines will vary from country to country. And in fact some seasons there may be strains of say, mefloquine resistant malaria in South East Asia, whereas other seasons there may not be. So keep up to date, take a look at the guidelines. You're not going to be expected to know the exact guidelines from year to year for your exam, but you will be expected to be able to look them up when you're in clinical practice. In terms of the principles of prevention behind malaria prophylaxis, chloroquine generally remains the first line choice in areas without resistant Plasmodium falciparum. 12:03 Atovaquone-proguanil (Malarone) is the first line choice in areas with chloroquine resistant Plasmodium falciparum. 12:10 Mefloquine is chemically related to quinine and is still used for prophylaxis. However, it's no longer considered a first-line agent for most travelers due to concerns about neuropsychiatric side effects. Other second-line drugs which are used in chloroquine-resistant areas are doxycycline and tafenoquine. 12:30 Primaquine is also used in terminal prophylaxis of P. vivax and P. ovale as well. This table summarizes the CDC Guidelines for Malaria Prophylaxis, but remember that the choice of prophylaxis should always be guided by the most current regional resistance data and guidelines from health authorities such as the CDC and WHO. 12:52 I encourage you to familiarize yourself with this information, not for memorization, but as a reference for your future clinical practice.
About the Lecture
The lecture Antimalarial Drugs – Antiprotozoal Agents by Pravin Shukle, MD is from the course Antimicrobial Pharmacology. It contains the following chapters:
- Antimalarial Agents
- Chloroquine & Drugs Derived From Artemisinin
- Quinine & Mefloquine
- Primaquine & Antifolate Drugs
- Doxycycline & Amodiaquine
- Atovaquone & Halofantrin
- Prevention of Malaria
Included Quiz Questions
Which of the following drugs was the first widely used antimalarial drug; but resistance is now common due to decreased accumulation of the drug within the food vacuole?
- Chloroquine
- Artemisinin derivatives
- Doxycycline
- Clindamycin
Which drug is associated with neuropsychiatric disorders, including nightmares?
- Mefloquine
- Chloroquine
- Quinine
- Artemether
- Primaquine
Which drug can cause aplastic anemia?
- Amodiaquine
- Doxycycline
- Tetracycline
- Mefloquine
- Primaquine
What is one of the principle mechanisms of action of artesunate?
- Form free radicals (•O and O•).
- Prevents the conversion of ATP
- Destroys the cell wall
- Inhibits microtubules
- Creates double-strand breaks
What is the principal mechanism of action of chloroquine?
- Interferes with the detoxification process of heme in the parasite food vacuole
- Prevents mitosis
- Generates free radicals in the nucleus
- Crosslinks DNA
- Creates pores in the cell wall
Which drug is used as a first-line treatment for severe malaria?
- (Intravenous artesunate
- Quinine IV
- Atovaquone IV
- Primaquine IV
- Tetracyclne IV
What is the mechanism of action of chloroquine?
- Interferes with the detoxification process of heme in the food vacuole, a toxic byproduct of hemoglobin digestion.
- Prevents mitosis
- Generates free radicals in the nucleus
- Crosslinks DNA
- Creates pores in the cell wall
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |