Playlist
Show Playlist
Hide Playlist
Anticoagulants
-
Slides Anticoagulants.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
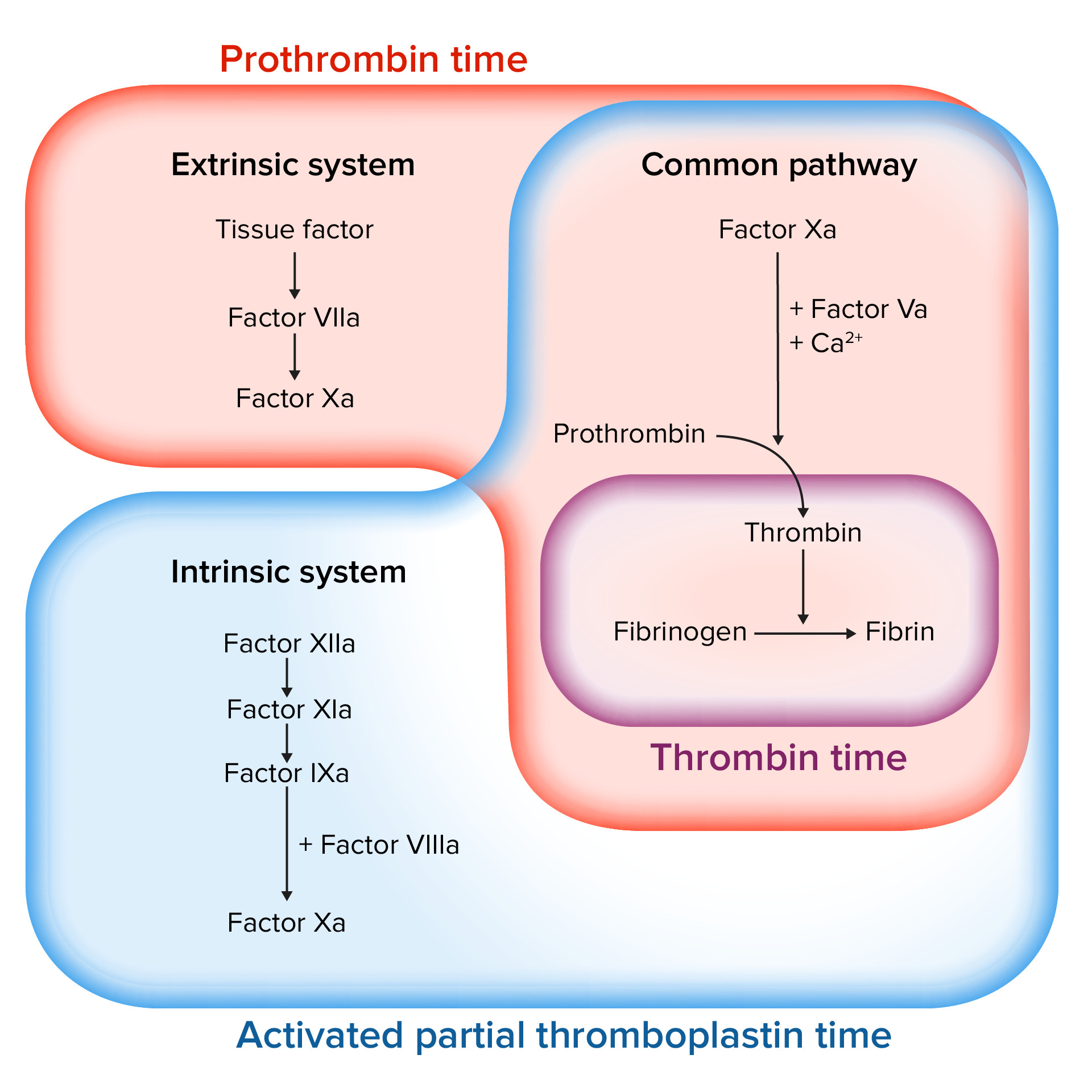
00:01 Let's move on to “Heparin.” So, heparin is a huge molecule, you can see the chemical structure here, obviously, you don't need to know the chemical structure, just know that unfractionated heparin, can have a multiplicity of molecular weight. 00:15 Some of the heparin molecules are 3,000 Da in weight, some of the molecular weights are 25,000, we call that unfractionated heparin, it's old school. 00:26 It is highly acidic so it's neutralized by a base, and that base can be protamine, so, protamine zinc is commonly used as an antidote to heparin. 00:37 Now, heparin binds to antithrombin III, and it forms a complex, and that complex inactivates thrombin, and it also inhibits factor Xa, and other factors that we won't get into right now. 00:49 The important point is, is that unfractionated heparin has a multiplicity of molecular weights, and it's a large molecule. 00:57 It's always given subcutaneously, we never ever want to give this drug intramuscularly. 01:03 It may cause a moderate transient throvermbocytopenia, and the thing that we always bring up in exams, is heparin-induced thrombocytopenia and thrombosis, it's a potentially fatal complication, I've had a few patients actually with HITT, and they're not fun to manage, this is something that we often ask on exams, so, when you have a patient clinical scenario on an exam, where they're starting to have thrombocytopenia, and thrombosis and perpura, and they're on heparin you should think about H-I-T-T. 01:33 Heparin, the unfractionated version, may also be linked to osteoporosis, when you use it chronically. 01:41 So, we had problems with unfractionated heparin, so, we came up with a new type of heparin called, “Low molecular weight heparin.” They don't bind to thrombin, but they do still inactivate factor Xa, therefore, the aPPT test is not a reliable test, when really using the low molecular weight heparins. 02:00 So sometimes, we will use an anti-factor Xa assay to determine, whether or not the low molecular weight heparins are working or not. 02:08 But the real-world issue is, is that because they're so predictable, we rarely use blood tests to confirm activity. 02:16 They're usually given once a day or twice a day as a sub-q injection. 02:20 The most commonly used are enoxaparin, dalteparin, and tinzaparin, there are others that are on the market, but these are the ones that you're going to see on your exam. 02:30 Just remember the suffix, and you should be able to identify the low molecular weight heparin. 02:35 The next interesting drug in the anticoagulation world, with respect to heparin is, “Fondaparinux.” Now, if you take a look at this huge heparin molecule, you can see something that I've circled in green for you, and that five-sided pentamer, is the active portion of heparin. 02:54 And what some companies have done is, they've actually isolated that pentamer, that is probably the most active portion of heparin, and it activates antithrombin III, in fact, it is so powerful, that it actually increases the anticoagulation effects of antithrombin III, by almost a thousand times, it does not inhibit thrombin and it's used daily subcutaneously. 03:19 Look at this cute little guy, this is the medical leech, the medical leech, its first name is, Hirudo, and so not surprisingly, we developed a drug that came from the toxin of the leech called, “Hirudin.” This particular direct thrombin inhibitor, binds to thrombin itself, and all of the thrombin substrates, and when it binds to the thrombin in the serum, it will cause less clotting, but what's unusual about this drug, and its unlike heparin and the other drugs, is that, it also binds to thrombin within the clot itself. 03:52 Remember that, heparin was this huge molecule, this is a small molecule that can get into clots. 03:57 So, one of the things that we like to use this drug for, are people who have had bad reactions to heparin, like HITT, we use this instead. 04:06 We can use the aPTT to monitor the effects of hirudin, there's bivalirudin, there's a bunch of other drugs that are used in this drug class. 04:16 There is a short-acting version of this drug that's used in the cath lab, and that particular agent binds to the thrombin only. 04:25 We have a new drug class called the, “Direct antithrombin inhibitors.” These drugs are generally called, “NOACs,” because they stand for, “Novel Anticoagulant Drugs.” But because they've been on the market now for five or six years, we've kind of discarded the word, NOAC. 04:43 Pradaxa or dabigatran is used as a twice daily drug, you can see that it's much smaller than the heparin molecule, it's approved for stroke prevention in atrial fibrillation, it's also used for DVT prophylaxis, in post-op hip and knee surgery. 04:59 The antidote called “Praxbind,” it is a monoclonal antibody. 05:05 Let's go to the old standby, “Warfarin.” Warfarin is the most commonly used drug in the entire lecture class. 05:14 There are several derivatives that are used in Latin America and in the European Union, but in general warfarin is the most commonly used globally. 05:22 It is a small molecule, it's lipophilic, it does interfere with vitamin K dependent factors. 05:29 It inhibits specifically the vitamin K epoxide reductase or, (VKOR). 05:34 So, VKOR or vitamin K epoxide reductase, may be a term that you see in your exam, and in your exam prep, remember that warfarin inhibits that. 05:45 Warfarin therefore inhibits vitamins: II, VII, IX, and X. 05:50 You need to know those factors, these are factors that we'd like to ask questions on. 05:56 What's interesting about warfarin, and what's fun about warfarin is that, it actually inhibits factors C and S as well. 06:02 So, although it inhibits procoagulant factors, it also inhibits inhibitory factors too. 06:09 Why is that important? Well, I'll show you. 06:12 Take a look at this graph. 06:13 You can see in blue, that factor C, is one of the first factors that's inhibited by warfarin. 06:23 So, inhibition starts with the inhibitory factors protein C and S, this actually gives a procoagulant effect, so, that means that after day one, the other factors are affected, but overall, you have initial period of hypercoagulability, followed by hypocoagulability, this makes for a real headache in the real world. 06:45 So sometimes, we have patients when we put them on warfarin, actually, form clots more, when we start them on the drug, that's why in high-risk patients, we bridge them. 06:55 So, we may bridge patients who are high risk with heparin, for a couple of days, when we first start warfarin, and then once they get past that procoagulant activity, and these other factors start to come into play, that's when we can drop the heparin and just use warfarin on its own, and then we monitor INR. 07:15 Now, there's going to be a number of interactions with warfarin, There is non-pharmacological interactions, and there is pharmacological interactions, let's talk first about non-pharmacological interactions. S Normally, vitamin K is produced in part by gut flora, or normal bacteria in the gut, if we give a patient antibiotics, we may kill off some of these bacteria, and therefore, you have lower levels of vitamin K. 07:42 When you have lower levels of vitamin K, you don't produce clotting factors as quickly. 07:47 So often, three to seven days after you start a broad spectrum antibiotic, the INRs start to climb. 07:54 So, it's very important if you have patients on warfarin, you monitor the INRs about once a month if they're stable, but as soon as they're started on an antibiotic, you have to monitor them once a week. 08:05 I have 1,200 patients on warfarin it's a real headache, it's one of the reasons why most doctors don't like to use warfarin, because it's so much work. 08:14 The inhibitors of warfarin, which are listed here, reduce the clearance of warfarin and therefore the INR will climb, so, it's really important knowing, that there are a lot of drugs that are going to interact with warfarin, as well as the antibiotics through a non-pharmacological pathway. 08:31 Due to the multiple pharmacologic and non-pharmacologic interactions, and the narrow therapeutic index of warfarin, patients should regularly monitor the prothrombin time, “PT” and “INR.” When the INR is too high, there is increased risk of hemorrhage, and when it is too low, there is increased risk for thrombosis. 08:53 The most specific antidote for warfarin toxicity is vitamin K, unfortunately, vitamin K takes several hours, in order to reverse the effects of warfarin. 09:04 So, in the case of a life-threatening hemorrhage, additional measures need to be taken. 09:09 These include: Administration of fresh frozen plasma, or prothrombin complex concentrate, which contain coagulation factors. 09:19 The new class of drugs that are factor Xa specific, directly bind to factor Xa. 09:26 The most popular drugs in this class are, "Rivaroxaban and apixaban," though there are several others that are also used around the world, importantly they all end in, “Xa-ban.” And the easy way to remember their mechanism is to think of “X-A,” being “10a” and “Ban” meaning, they “Ban 10a.” These medications have several important indications including: VTE treatment, prevention of clots in atrial fibrillation, and post-op DVT prophylaxis, usually in orthopedic procedures, where there may be prolonged periods of immobilization. 09:55 These medications can be reversed if needed, with an agent called, “Andexanet alfa.”
About the Lecture
The lecture Anticoagulants by Pravin Shukle, MD is from the course Pharmacology of Blood Coagulation. It contains the following chapters:
- Anticoagulants: Heparins and Fondaparinux
- Anticoagulants: Direct Thrombin Inhibitors
- Anticoagulants: Warfarin
- Anticoagulants: NOAC's – Factor Xa Inhibitors
Included Quiz Questions
What is a potential complication of long-term treatment with unfractionated heparin?
- Osteoporosis
- Thrombocytosis
- Thrombosis
- Vitamin K deficiency
- Injection site reaction
In the event of a life-threatening hemorrhage resulting from warfarin toxicity, which of the following interventions is most appropriate?
- Administration of fresh frozen plasma
- Oral administration of vitamin K
- Intramuscular injection of protamine sulfate
- Intravenous infusion of vitamin K
- Intravenous infusion of a direct thrombin inhibitor
What lab test is considered the gold standard for monitoring low molecular weight heparin (e.g., enoxaparin)?
- Anti-factor Xa assay
- Activated partial thromboplastin time
- Adenosine
- Fibrinogen
- International normalized ratio
Which anticoagulants is noted for being able to bind clot-bound thrombin?
- Hirudin
- Warfarin
- Phosphodiesterase (PDE) inhibitors
- Cyclooxygenase (COX) inhibitors
- Unfractionated heparin
Initial inhibition of which factor(s) by warfarin leads to its immediate procoagulant effect?
- Factors C & S
- Factor II
- Factor X
- Factor IX
- Factor VII
Customer reviews
2,5 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
2 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
2 |
my native language isn't english so i helped me reAding subtitles, but in this lecture, subtitles are not according to the speech. Please try to fix it. this is not the first time :( however the doctor explains very well , five starts for the doctor. one start to the tech support
3 customer reviews without text
3 user review without text