Playlist
Show Playlist
Hide Playlist
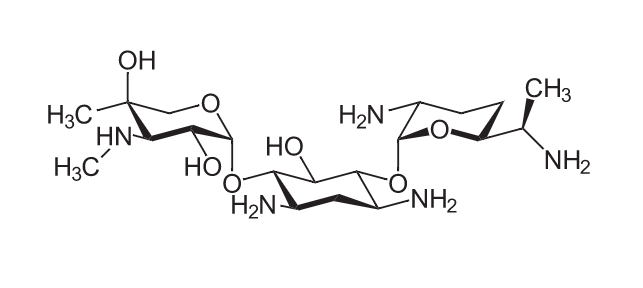
Aminoglycosides – Bacterial Protein Synthesis Inhibitors (Antibiotics)
-
Slides Aminoglycosides Antibiotics.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
00:00 Let's move on to the aminoglycoside antibiotics. 00:04 So the aminoglycoside antibiotics are incorporated into the bacteria through an oxygen dependent process. 00:10 Therefore, these medications don't work that well against anaerobic bacteria. 00:16 The aminoglycoside seen in the red triangle there, binds to the 30S subunit of the ribosome. 00:23 Now how it works is it inteferes with protein synthesis by preventing the initiations complex from forming. 00:31 So that's when the bottom of the ham burger bun, the top of the ham burger bun and the cheese which is the mRNA which all come together. 00:38 The aminoglycosides prevent that entire initiation complex from coming together. 00:43 It can also cause misread errors on the messengerRNA. 00:49 So the messengerRNA is now prone to making mistakes. 00:53 So instead of putting in amino acid number 5, it will put in amino acid number 11 for example. 00:59 The other thing that happens as well is that it does cause some inhibition of translocation which is another potential mechanism that these drugs use. 01:09 They are highly dependent upon concentration. 01:13 So aminoglycosides are concentration dependent antibiotics. 01:19 These medications actually work better when given intermittently. 01:24 So your better off having a high peak and a trough then you're having steady state level. 01:30 This is what makes these medications unique. 01:33 They are concentration killers as opposed to time killers. 01:36 So we like to have an intermittent on off exposure to these medications. 01:43 As I said before concentration dependent killing action. 01:46 They also have a very strong post antibiotic activity. 01:50 Which is why we can afford to have low levels or trough levels when we give these medications. 01:55 Remember that aminoglycosides are really polar so they must be given IV or IM. 02:02 They are not given orally. 02:03 They are excreted through the kidney or renally. 02:07 So renal function will determine the dose. 02:11 So a lot times in patients with renal failure, will actually do what's called "Peak and Trough Levels." So monitoring drug levels is a big issue. 02:19 The other thing I want to mention is that these drugs do not cross the blood brain barrier. 02:25 They do better as large, single doses than as multidose regimens. 02:31 Because like I said like the peak and trough. 02:33 And the toxicity of these medications limits the peak concentration. 02:38 So that's what limits our top level. 02:42 Now the broad spectrum agent active across many classes of bacteria is very typical of aminoglycoside activity whether it's gentamicin or whatever. 02:54 E.coli, Haemophilus influenzae, Klebsiella, Moraxella species, Proteus species, Serratia species, Shigella species. 03:03 These are all very susceptible to this class of drugs. 03:07 They are almost always used in combination with the penicillin. 03:11 So there's kind of like this pairing, this husband and wife kind of team that we like. 03:16 So ampicillin always seems to go with gentamicin. 03:19 And piperacillin seems to go with tobramycin. 03:21 They work very well together. 03:23 Ampicillin is more about broad spectrum. 03:26 Gentamicin is more broad spectrum. 03:28 So we use that in more of a broad spectrum kind of situation. 03:33 Pip/Tobra is used more in gram negative disease. 03:36 And the reason why these two combinations work so well is because of something called antibacterial synergy. 03:45 So what's that mean? If you think about it, the ampicillin or the piperacillin their job is to open up the cell wall. 03:55 That allows the gentamicin or the tobramicin to get into the cell. 04:00 And now their concentration near the ribosome is much greater. 04:04 So the ampicillin knocks down the door. 04:08 And the gentamicin goes through in the door and does the job. 04:11 So that's why these two drugs seem to work so well together. 04:15 Whether they are Amp/Gent or Pip/Tobra. 04:20 Gentamicin is the prototypical drug. 04:23 Tobramicin also has activity against Pseudomonas and it's used more in gram-negative disease. 04:29 There are whole list of those gentamycin antibiotics. 04:32 And streptomycin is one of them and it's certainly a very effective class. 04:38 Now toxicity is going to be a big concern with aminoglycosides. 04:43 Ototoxicity. 04:45 So a lot of people get ototoxicity. 04:46 This is on exams. 04:48 And it is also something important for clinical practice. 04:51 You need to be aware of this; auditory symptoms, or amikacin, vestibular symptoms or gentamycin and tobramycin. 04:58 So, although both are working on the inner ear, there's a slight difference between the two. 05:03 So vestibular symptoms are gent and tobra, auditory symptoms are amikacin. 05:10 Other toxicity includes neuromuscular blockade. 05:13 There's a curare like illness and you treat it with calcium and neostigmine. 05:18 Finally, there are some skin reactions, mostly with neomycin that you have to be aware of.
About the Lecture
The lecture Aminoglycosides – Bacterial Protein Synthesis Inhibitors (Antibiotics) by Pravin Shukle, MD is from the course Antimicrobial Pharmacology.
Included Quiz Questions
What is NOT part of the mechanism by which aminoglycosides interfere with protein synthesis in bacterial organisms?
- Blocks transcription on the 50S subunit
- Prevents the initiation complex from forming
- Incorporated into the bacteria through an oxygen-dependent process
- Inhibits translocation
- Causes misreading errors in the mRNA
What statement about aminoglycosides is INCORRECT?
- Vestibular toxicity is commonly associated with amikacin.
- They must be given intravenously or intramuscularly.
- They exhibit strong post-antibiotic activity allowing low trough levels.
- Drug levels must be monitored using peak/trough levels to ensure concentration-dependent killing action.
- Dosing depends on renal function
Which statement about aminoglycoside toxicity is INCORRECT?
- Neomycin is the treatment for aminoglycoside-induced neuromuscular blockade.
- Tobramycin is associated with vestibular ototoxicity.
- Amikacin is responsible for the auditory deficit.
- Gentamicin is associated with ototoxicity.
- Skin reactions are usually associated with the use of neomycin.
What class of antibiotics are frequently co-administered with aminoglycosides?
- Penicillins
- Cephalosporins
- Vancomycin
- Macrolides
- Tetracyclines
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This actually was an amazing lecture. Made me understand a lot of issues around Gentamycin.