Playlist
Show Playlist
Hide Playlist
Adrenal Incidentalomas – Adrenal Cortex
-
Slides AdrenalCortex EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
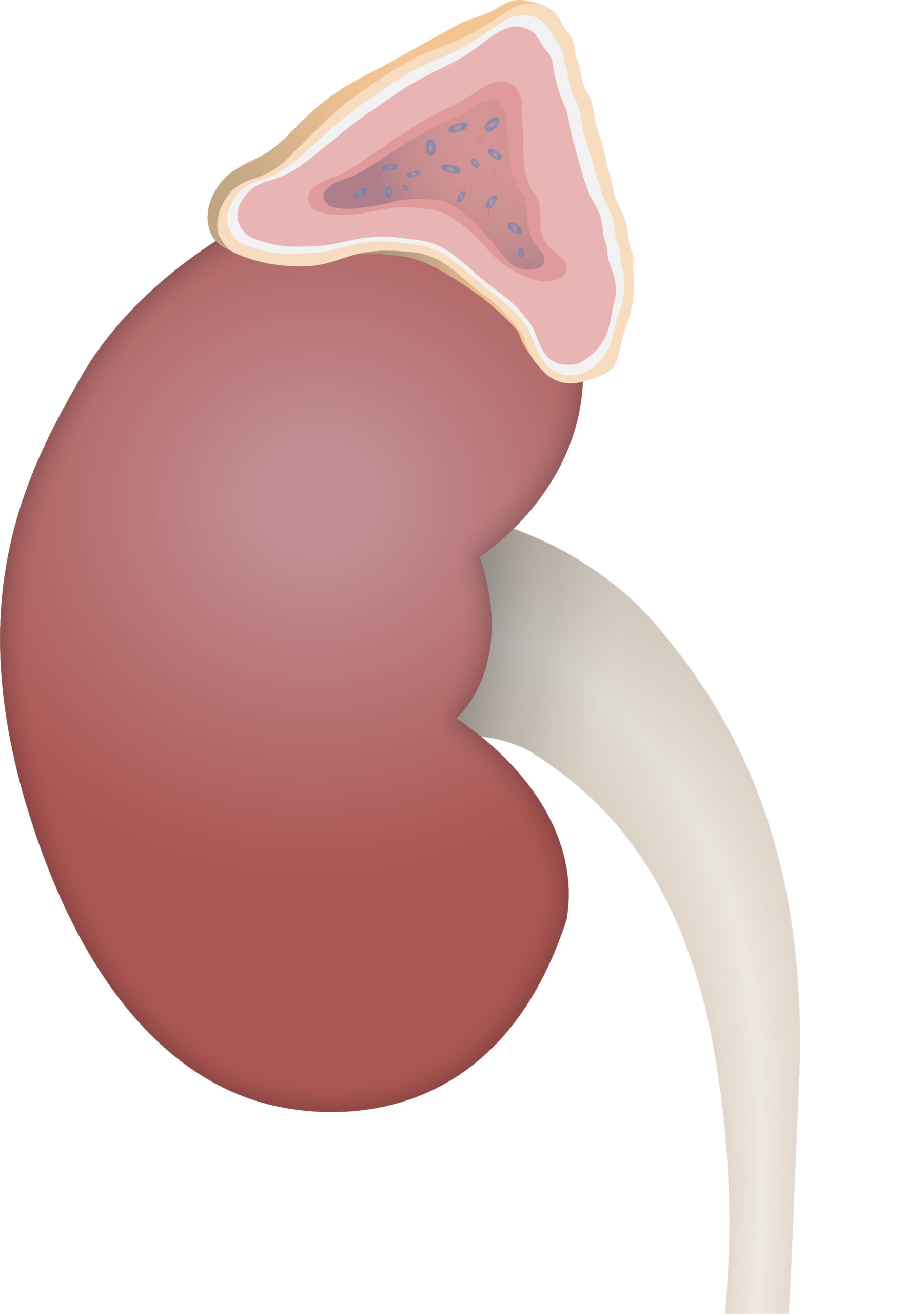
Download Lecture Overview
00:01 Let's talk about a few issues within the adrenals and we will begin by looking at incidentalomas, as the name implies. 00:08 Adrenal masses incidentally detected up to one and a half percent of your abdominal scans? incidentalomas. 00:17 Majority of these are non-functioning adrenal adenomas, but can represent hormonally active or even malignant lesions. 00:24 So, there is further workup that you're always making sure to confirm or to diagnose your patient accordingly. 00:31 Pheochromocytoma may be asymptomatic and remember, a pheochromocytoma would be a adenoma that's located inside your adrenal medulla. 00:43 It's an adenoma, a pheochromocytoma; it is not a cancer. 00:48 It's not-It's not malignant, it's not adenocarcinoma. 00:51 All Adrenal incidentaloma patients should be screened for an asymptomatic pheochromocytoma. 00:56 This is typically done with the CT, but biochemical screening can be done if the unenhanced CT attenuation is greater than or equal to 10 HU. 01:04 These patients should also be screened for Cushing's syndrome, though primary hyperaldosteronism workup is not indicated unless there are clincal symptoms present. 01:14 Biopsy cannot differentiate benign from malignant primary adrenal tumours, but has a role in evaluating possible adrenal metastases in patients with known extra-adrenal primary malignancies. 01:29 So, if you were to take a look at that adenoma, biopsy would not be your next step of management necessarily to distinguish between benign and malignant, but if it's coming from, let's say, a renal cell cancer that's metastasized to the adrenals, sure. 01:47 The biopsy will help you differentiate between the two because it will show you the histology of where the metastasis is coming from. 01:55 Adrenal imaging is important. 01:58 Lesions less than 10 Hf are noncontrast CT are almost always benign or may or may not be functional. 02:06 Greater than 50 percent washout of enhancement adrenal protocol CT also suggest benign adenoma, unless there is a very high peak enhancement which raises possibility of pheochromocytoma. 02:18 So, usually if it's less than 10, usually tends to be benign, but that is not a guarantee. 02:25 Lesions greater than four centimetres increase suspicion of malignancy and should be automatically next step of management surgically removed upon adrenal imaging. 02:37 Pheochromocytoma usually a vascular tumour, increased T2 signal on MRI and you would then find enhancement adrenal protocol CT, meaning to say that if you're doing an avid arterial phase enhancement, all of these would then help you distinguish a pheochromocytoma from others, usually, a vascular tumour. 03:00 Remember, if you have a pheochromocytoma outside of the adrenal medulla, as far as you're concerned, you would then consider that to be a paraganglion.
About the Lecture
The lecture Adrenal Incidentalomas – Adrenal Cortex by Carlo Raj, MD is from the course Adrenal Gland Disorders.
Included Quiz Questions
Which diagnosis is suspected when an adrenal incidentaloma patient is screened with plasma or 24-hour urine metanephrines?
- Pheochromocytoma
- Cushing syndrome
- Primary hyperaldosteronism
- Primary malignancy
- Pituitary adenoma
When should primary hyperaldosteronism be worked up in a patient with an adrenal incidentaloma?
- In the presence of clinical signs and symptoms
- In any adrenal incidentaloma
- After pheochromocytoma has been ruled out
- After an inconclusive biopsy
- In a patient under the age of 50
What is the size threshold for adrenal incidentaloma removal?
- Greater than 4 cm
- Greater than 1.5 cm
- Greater than 8 cm
- Greater than 10 cm
- Greater than 0.5 cm
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |