Playlist
Show Playlist
Hide Playlist
Adaptive Immunity: B Cells and Antibodies
-
Slides Adaptive Immunity.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
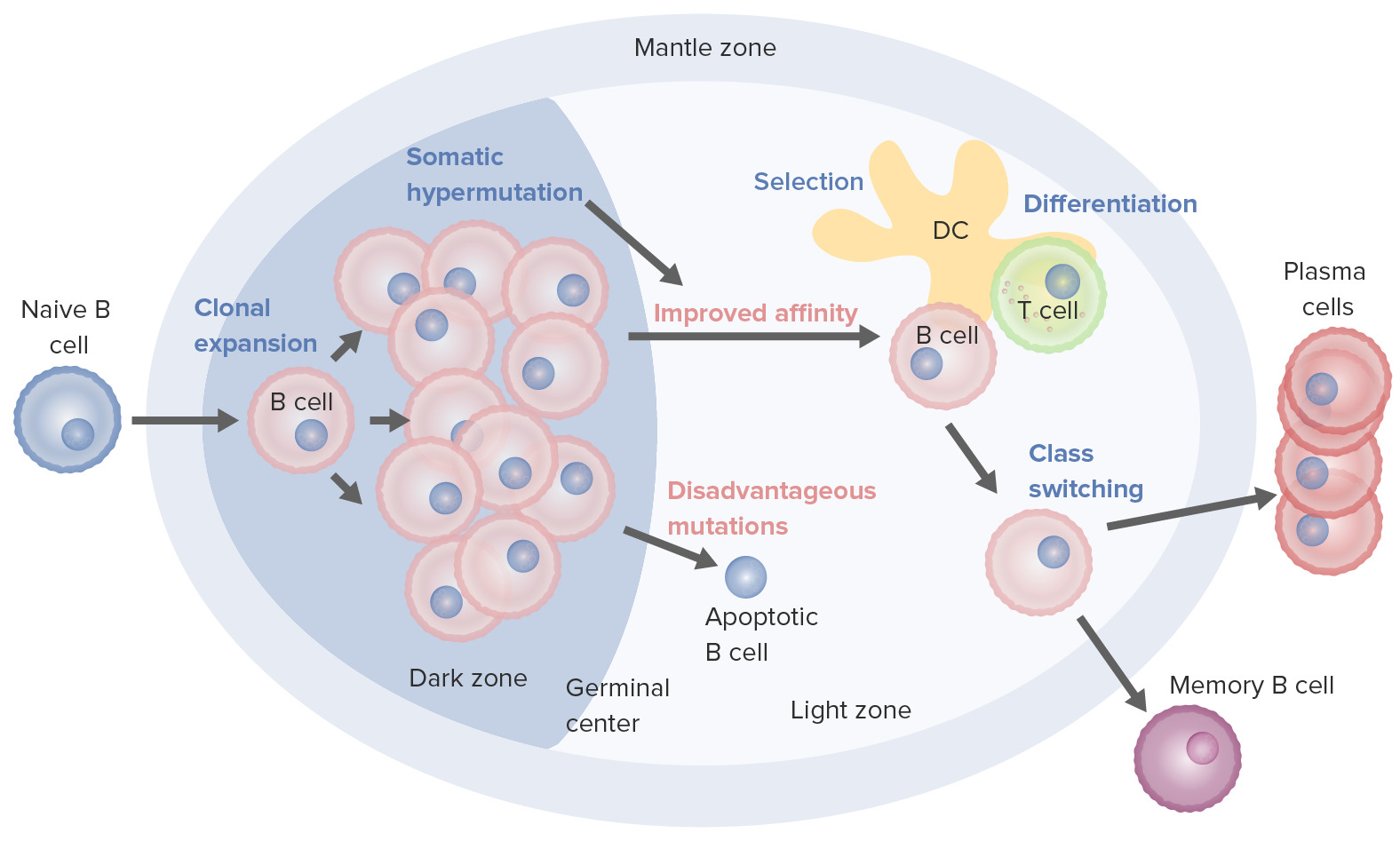
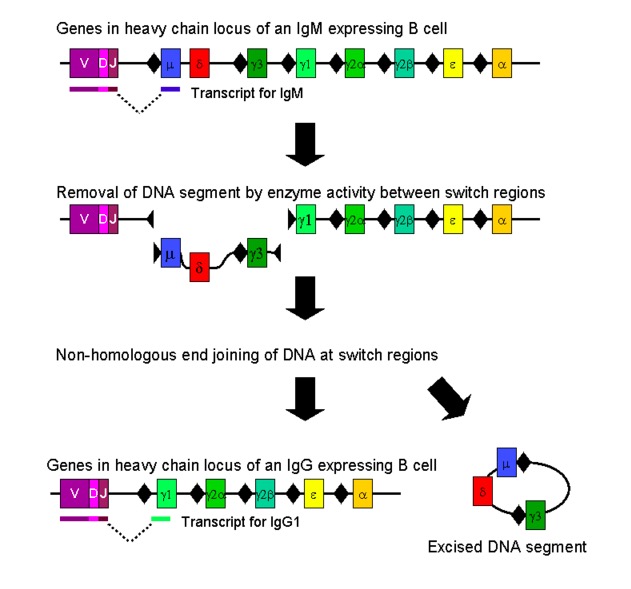
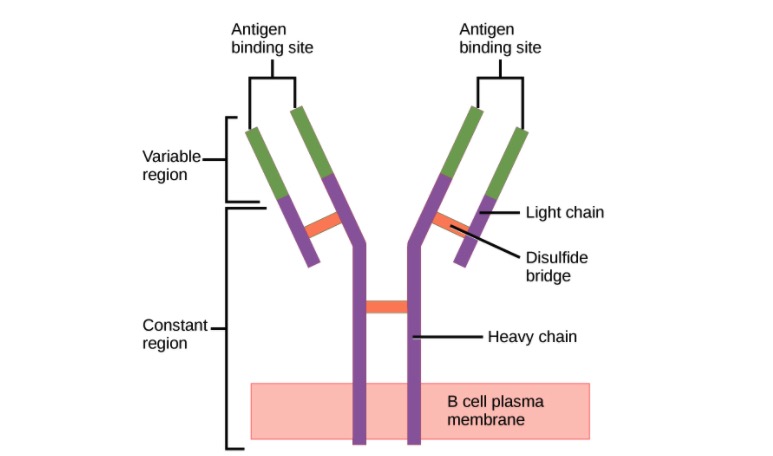
00:01 Welcome back. 00:03 We've talked about some of the cells and some of the proteins involved in innate immunity. 00:09 Let's go into a little bit more detail about the cells and components of adaptive immunity. 00:15 And this is where it gets really interesting. 00:17 This is a higher level of complexity. 00:20 This is basically an entire series of lectures that could be called immunology. 00:26 And we're going to cover it here in a very short little vignette. 00:29 There are lots and lots of important details, we'll hit the highlights however, because it can become very bewildering and complex. 00:39 So we'll try to keep it at a high level so you can kind of grasp the gist of the important concepts. 00:47 So, the first cell of adaptive immunity is the B cell and B cells will recognize particular antigens present on the surface of microbes or proteins or whatever, and will make antibodies of the same recognition motif. 01:06 So a B cell can recognize a particular molecule on a microbe and then when it binds to that microbe, it will generate antibodies that also recognize that same receptor, or the same molecule. 01:23 The antibodies are synthesized by plasma cells. 01:25 So a B cell needs to go through sequential activation steps until it becomes a plasma cell that's a terminally differentiated B cell that's going to crank out tonnes and tonnes of antibodies. 01:38 It's important to know that the antibody binds an intact antigen. 01:42 So the entire 3D conformation of a particular antigen is what the B cell receptor sees and what the antibody or the immunoglobulin sees. 01:53 And there of course, there's greater complexity. 01:56 So there are five basic isotypes of immunoglobulin, and they're in that final bullet point. 02:03 IG stands for immunoglobulin, and you can have IgG, IgM, IgA, IgE, and IgD. 02:12 It turns out that the most important circulating immunoglobulin is IgG. 02:18 IgM is also a circulating antibody for the most part. 02:22 IgA is going to be very, very important for mucosal immunity, it's going to be the dominant immunoglobulin type isotype that's present in the airways and in the GI tract. 02:37 And then IgE, as we've talked about, is going to be important for activating mast cells through the Fc epsilon receptor that the IgE binds to. 02:47 And then IgD is a kind of a minor player, but just be aware that it is part of the maturation schemes the B cells go through as they turn into plasma cells. 03:00 Okay, so... 03:01 I've also simplified it, it turns out that there are different forms of IgG, there's IgG1, IgG2, IgG3, etc. 03:11 They all have slightly different capacity to bind to macrophages, and to neutrophils. 03:20 They all have slightly different capacity to activate complement. 03:23 So all these different isoforms of the immunoglobulin to have a reason, but we're not going to get into all of those excruciating details. 03:35 So what does antibody do? Well, first of all, it can bind to a protein or to a microbe or to a cell, and so called neutralize it. 03:48 So that means that if I have a Hepatitis B virus that wants to get into an a parasite, it does so through with particular lagging receptor interaction, but I can synthesize neutralizing antibodies that bind to the component on the hepatitis B virus and coat it completely, covered up so it can no longer interact with the receptor, the potential receptor on hepatocytes. 04:16 In fact, that's the mechanism by which vaccinations work. 04:21 So neutralization. 04:22 You can also have neutralization of a protein, diphtheria toxin, for example, we used to treat it by taking extracts of antibodies from immunized horses where they had antibodies to diphtheria. 04:36 And then we would someone who had gotten a diphtheria infection, we throw in that horse serum containing those antibodies, and it would neutralize the protein before it could cause damage to cells. 04:46 So you can neutralize microbes, you can neutralize proteins. 04:50 What else do antibodies do? They do marvellous things. 04:54 What they do here is that they promote phagocytosis. 04:57 So if an antibody is bound to a particular microbe. 05:00 The Fc the constant region portion of an antibody will undergo a conformational change. 05:05 And now that antibody bound to its microbe will become tasty to macrophages or neutrophils, and they will phagocytosis that making it tasty thing that's called opsonization. 05:18 The antibody is an opsonin, coating a particular target. 05:21 And now with the rearrangement and the Fc allows binding to Fc receptors on the surface of phagocytes and they will eat it. 05:29 So another marvellous thing that antibodies do. 05:32 Remember, from one of our previous sessions together on innate immunity, we talked about the natural killer cell. 05:40 Well, it also has receptors for antibody bound to a particular target. 05:46 And when it does that, it will kill. 05:49 So that's the antibody dependent cell mediated cytotoxicity or ADCC that we talked about. 05:55 What else do antibodies do? Well, they activate complement. 05:58 Remember, complement gets activated at a very reasonably low level on microbial surfaces. 06:05 But we get a 10,000 fold better activation if we first bind antibody and that's what's being shown there, antibody being bound to a microbe. 06:14 Conformational change of the Fc portion of antibody will allow us then to have complement activation at a much better rate. 06:24 And that will cause the lysis of anything that the antibody is bound to. 06:30 As we go through the complement cascade and activation, we will make other fragments, remember we make C3a and C5a, well it turns out C3b because it very avidly binds to targets as well will allow phagocytic cells such as macrophages and neutrophils to bind via C3b receptors and to phagocytized. 06:53 So it's another way to opsonize. 06:55 Antibodies can directly opsonized and then activated complement components C3b in particular can also opsonize a target. 07:04 And it's good for both the macrophages and for the neutrophils. 07:08 Recall also as we activate complement, we generate C3a and C5a that's going to be very important for the recruitment and activation of things like neutrophils. 07:20 So that's antibodies and B cells. 07:23 What about the T cells?
About the Lecture
The lecture Adaptive Immunity: B Cells and Antibodies by Richard Mitchell, MD, PhD is from the course Immune-mediated Diseases.
Included Quiz Questions
What are terminally differentiated B lymphocytes called?
- Plasma cells
- Mast cells
- Neutrophils
- Lymphocytes
- Macrophages
What is the role of IgD?
- It is involved in the B lymphocyte maturation scheme.
- It is the most important circulating antibody.
- It is involved in complement activation.
- It is involved in mast cell activation.
- It is involved in mucosal immunity.
Which type of immunoglobulin has different subtypes?
- IgG
- IgM
- IgE
- IgF
- IgD
What are the main differences between the different IgG subtypes?
- They have different binding capacities to macrophages and neutrophils.
- They have different abilities to activate mast cells.
- Some subtypes come from B lymphocytes and others from T lymphocytes.
- Some activate complement and others deactivate it.
- They exhibit different degrees of mucosal immunity.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |