Playlist
Show Playlist
Hide Playlist
Acute Headache: Meningitis and Temporal Arteritis
-
Slides 08 Headache Neuropathology I.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
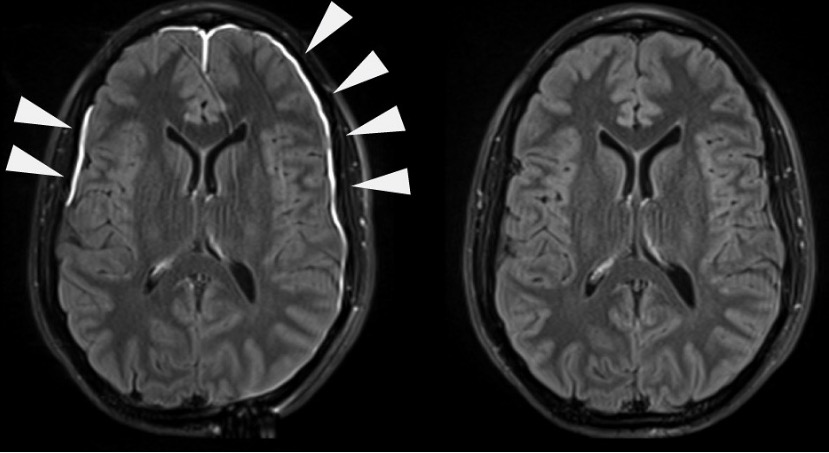
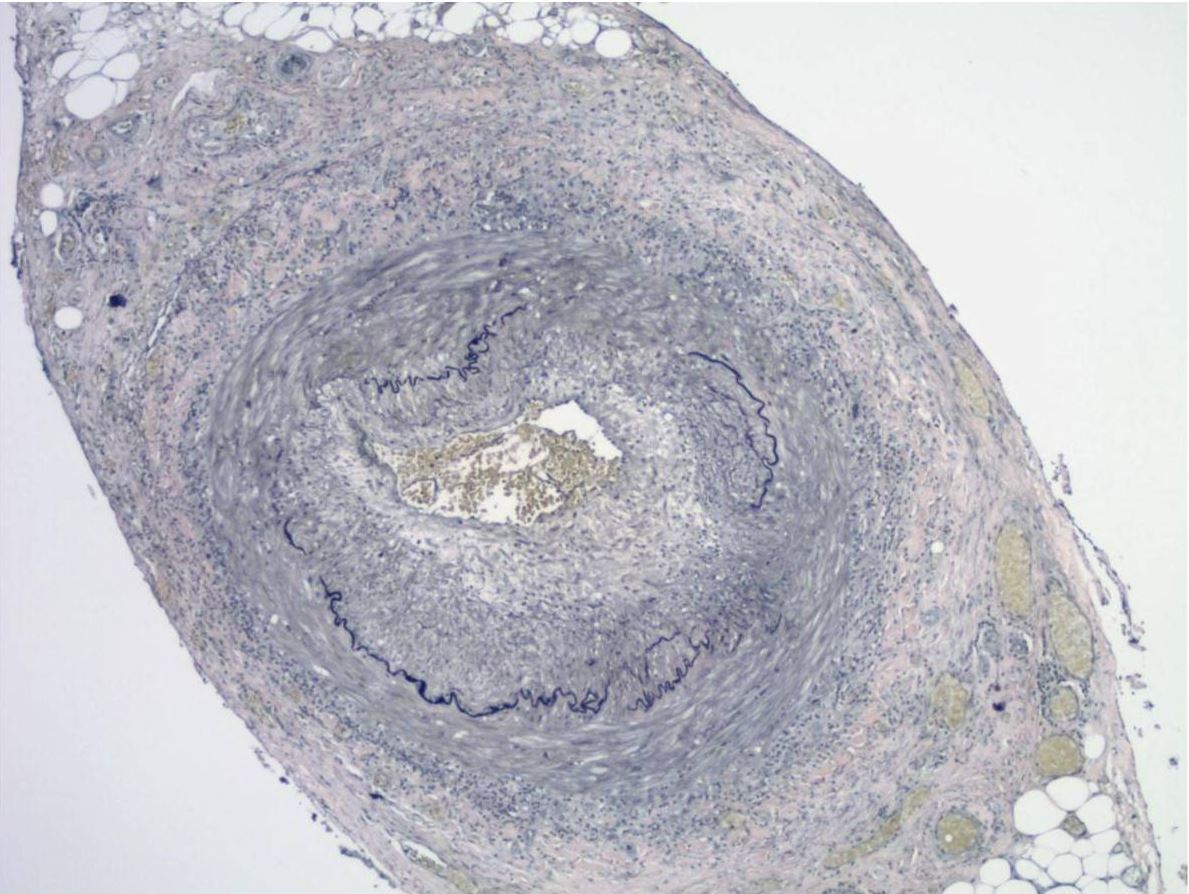
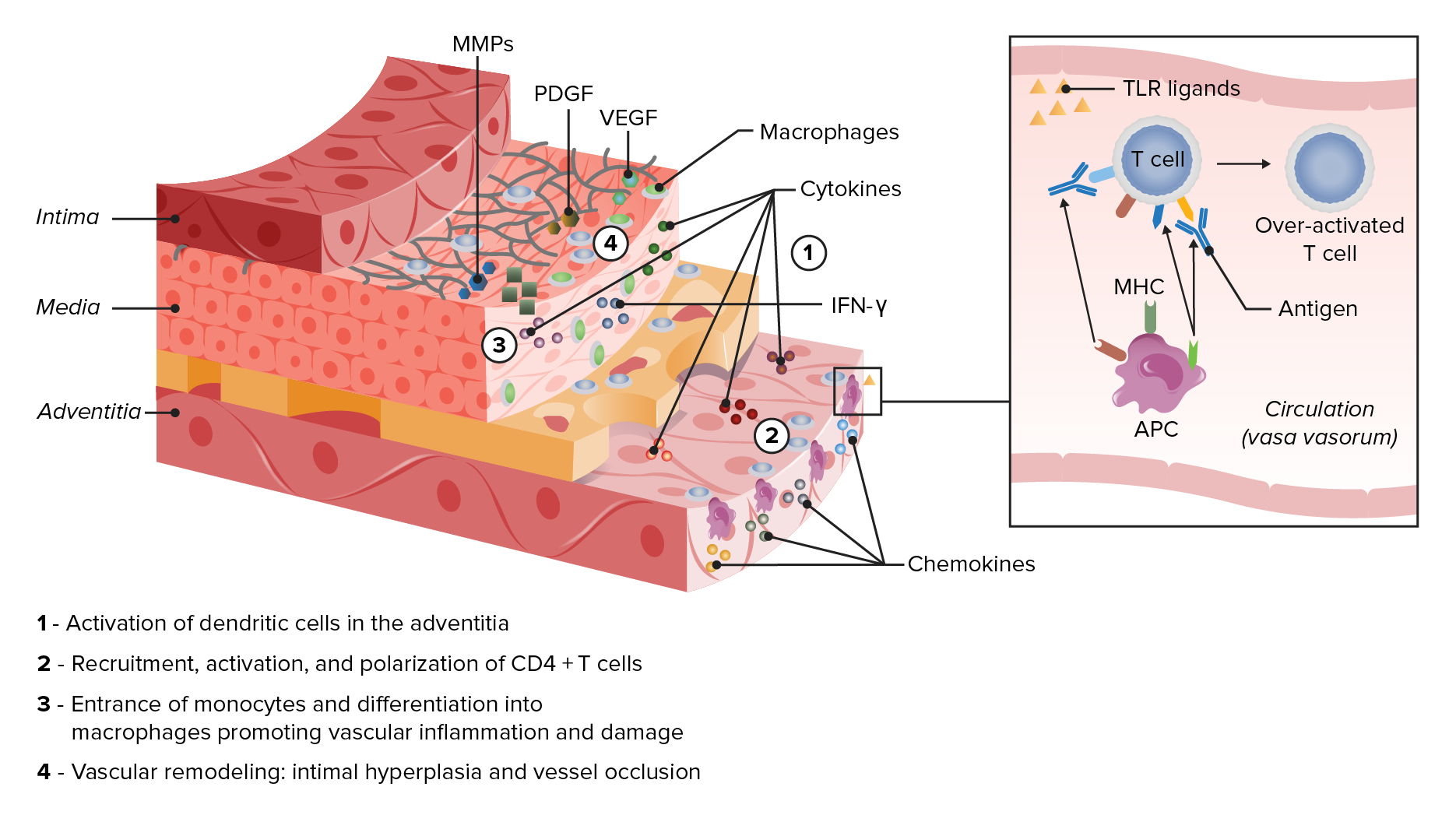
00:01 Let’s now take a look at acute severe headache. 00:05 What caused the intracerebral hemorrhage resulting in such a secondary headache? Subarachnoid, parenchymal, meningitis, temporal arteritis, hypertensive urgency, and sinus thrombosis. 00:19 Remember, with an acute severe headache, with a hypertensive urgency versus something known as your let’s say when we talked about hypertension, we had crisis and we had urgency. 00:33 We talked about the differences between the two. 00:38 Under acute headache, here once again, subarachnoid hemorrhage. 00:40 We know about the thunderclap. 00:41 We’ve talked about this being the worst headache in the patient’s life. 00:45 Severe, nausea, and vomiting, altered level of consciousness, and may present in coma worst case scenario. 00:51 We talked about the Hunt and Hess scale. 00:54 And may have a focal neurologic deficit and signs of meningismus. 00:58 Remember, we talked about if there was a berry aneurysm which was large enough and it ruptured, may result in a subarachnoid hemorrhage. 01:04 If left untreated, may also result in a, perhaps, herniation. 01:11 Intraparenchymal hemorrhage; acute in onset. 01:15 Focal deficit commonly occurs simultaneously. 01:19 Altered level of consciousness related to location and size of the bleed. 01:25 And small bleed in pons can significantly depress consciousness. 01:29 That’s important. 01:31 Do not confuse this with subarachnoid hemorrhage. 01:34 This is hemorrhage taking place of the brain structure itself. 01:39 Larger cerebral bleed can cause edema, mass effect, and perhaps even herniation. 01:48 With meningitis, we talked about this in great detail. 01:52 Let’s talk about the headaches that are associated. 01:55 In bacterial meningitis where we have glucose being decreased, neutrophils being elevated, protein being elevated. 02:03 Here, we have headache which is usually diffuse. 02:06 Fever and meningismus are typical. 02:08 May be absent in elderly or immunocompromised. 02:11 Look for that, please. Be careful. 02:12 Fever may not be necessarily seen. 02:15 Alteration in level of consciousness is frequent. 02:18 I want you to compare this with viral meningitis. 02:21 We have viral meningitis, and we have protein content, which is not so elevated. 02:27 If it's the WBC, then we’re looking at lymphocytes; and glucose tends to be normal. 02:31 A diffuse headache usually has developed over several days. 02:36 Associated symptoms of fatigue and myalgia are common. 02:39 Remember, when you have viral infection, then it’s not just restricted to the meninges. 02:45 It could also very much affect the muscle. 02:48 And we had that discussion earlier when we talked about HIV and AIDS. 02:52 Level of consciousness and neurologic exam should be normal for the most part with viral meningitis, so you don’t have this alteration on level of consciousness, as you’ve seen with bacterial. 03:04 It’s an important table for you to compare and contrast the type of headache with bacterial and viral meningitis. 03:12 With acute headache, temporal arteritis, your patient most likely, an elderly female, also known as giant cell arteritis. 03:19 Headache is typically intermittent, unilateral, temporal area at first, and then bilateral temporal when it becomes continuous. 03:29 Pain is often throbbing in nature. 03:32 “Doc, this headache that I have is throbbing.” “Where is it located?" Temporal, unilateral. 03:38 You should be thinking definitely, temporal arteritis. 03:42 Aching and burning. 03:43 Tenderness of the scalp. 03:48 With temporal arteritis, remember, this is a vasculitis of medium to large vessel diseases or blood vessels. 03:56 And if left untreated, meaning to say that you do a biopsy, remember, and you’re looking for granulomatous type of lesion in your temporal artery of approximately 2 to 3 centimeters. 04:08 And if left untreated, ophthalmic branch of the temporal artery might get affected and the patient is then left with being blind. 04:17 Usually affects people over the age of 60, women more than men. 04:21 Look for these being most common type of presentations. 04:26 Associated symptoms: jaw claudication. 04:29 Remember, temporal artery could have a branch. 04:31 We have jaw claudication, weight loss, low- grade fever, fatigue, and amaurosis fugax. 04:37 In other words, your retina for sure is going to get affected if left untreated. 04:56 Temporal arteritis associated findings: firm and tender superficial temporal artery, elevated ESR. 05:04 Obviously, ESR is non-specific. 05:06 We find this to be significantly elevated with this type of history. 05:11 High on the differential should be giant cell arteritis. Confirmation: biopsy, huh. 05:17 Biopsy. 05:18 First is negative. 05:20 You need to make sure that you do biopsy in the contralateral side because as I told you, the headache, throbbing on one side but could be both if it’s continuous. 05:29 And just because you find it to be negative on one side, you need to make sure that you rule this out. 05:34 Otherwise, as I said, your elderly patient is at risk for blindness. 05:39 Angiography of external carotid branches. 05:45 Management: steroids until biopsy is negative. 05:49 Don’t take chances. 05:51 Steroids have continued for months to years to prevent recurrence. 05:56 Unfortunately, if that vision has been compromised, very rarely does it recover. 06:04 Summary: Age: elderly. 06:08 Female. 06:09 Preventive: immunosuppressants. 06:11 Signs and symptoms: headache, acute vision loss, do not forget about jaw claudication, constitutional symptoms, low-grade fever, decreased temporal pulsations. 06:23 Your superficial temporal artery feels tender. 06:27 Differential diagnoses from this type of headaches: glaucoma, migraine, uveitis, retinal artery occlusion, amaurosis fugax. 06:36 We talked about significant, elevated levels of ESR and biopsy is confirmatory and management for sure, until that biopsy comes back to be negative empirically, you need to make sure that steroids has been started and administered.
About the Lecture
The lecture Acute Headache: Meningitis and Temporal Arteritis by Carlo Raj, MD is from the course Headache – Pathophysiology. It contains the following chapters:
- Acute Severe Headache
- Acute Headache: Meningitis
- Acute Headache: Temporal Arteritis
Included Quiz Questions
An elderly patient with a severe throbbing headache located on the left side of her scalp and temple has a tender cord-like pulsatile structure on the left side of her head. What is a potential cause of this condition?
- Temporal arteritis
- Migraine
- Tension headache
- Postcoital headache
- Subdural hematoma
Which of the following statements regarding giant cell arteritis is TRUE?
- The ESR is typically elevated, but not always.
- It is a small vessel vasculitis.
- It does not have any serious complications.
- It can be treated over a few days.
- Temporal artery biopsy is not needed if the ESR is normal.
What is the most likely diagnosis in a patient with uncontrolled hypertension who comes in with a sudden-onset "thunderclap headache" described as the worst headache of their life?
- Subarachnoid hemorrhage
- Subdural hematoma
- Encephalitis
- Cluster headache
- Temporal arteritis
Customer reviews
1,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
1 customer review without text
1 user review without text