Playlist
Show Playlist
Hide Playlist
Accidental Hypothermia: Symptoms
-
Emergency Medicine Cold Illness.pdf
-
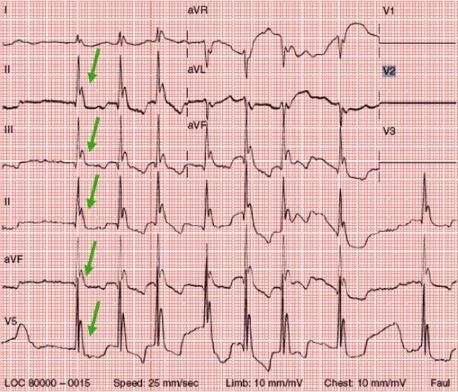
Download Lecture Overview
00:01 So, let's do a case study. 00:02 We have a 73-year-old man, he's "found down" on a park bench, it's in the middle of winter, his got a history of alcoholism and homelessness. 00:12 His temperature is 31.4, his bradycardic is 52, his respiratory rate is 8, his blood pressure is 98/40 and we're unable to obtain an oxygen saturation. 00:25 He's completely unresponsive to voice or pain, his pupils are fixed and dilated and his skin is cold and mottled. 00:34 What's the diagnosis for this unfortunate gentleman? This is a classic presentation of accidental hypothermia. 00:43 So, risk factors for hypothermia include impaired heat production. 00:48 Now, patients will make less heat if they have adrenal insufficiency, if they have hypothyroidism which down regulates the metabolic state, if they're hypoglycemic because they won't be able to produce the energy for shivering or non-shivering thermogenesis, if they're immobilize so they lose their skeletal muscle activity and lose heat production that way or if they're at extremes of age so, this is more common in neonates and the elderly. 01:15 Patients can also have increased heat loss so any kind of skin disease that decreases your ability -- the ability of the skin to sort of keep your heat inside of your body and lets you radiate more out into the world that's gonna increased your heat loss, burns by the same token will increased heat loss, also immobility. 01:35 Alcohol and this is a very, very important risk factor in hypothermia so one, you have impaired behavioral responses to cold when you're intoxicated with ethanol, you don't feel cold, you don't seek warmth, if you don't cover yourself up the way that you normally would if you were not intoxicated, it also impairs your shivering response. So, you make less heat and it causes vasodilation which allows you to radiate more heat out into the environment. 02:04 And then ethanol is actually implicated in the vast majority of accidental hypothermia that's in the United States. 02:10 Lastly we have impaired thermoregulation so if you have any kind of CNS pathology that prevents your brain from knowing when you're getting cold and affecting the appropriate physiological responses, that's gonna increased your risk of hypothermia. 02:26 There's various medications that will do it including antidepressants, antipsychotics and sedatives. 02:32 Spinal cord injuries, and dysautonomia also impairs your thermal regulation, as does polytrauma. 02:40 So as far as the cardiac manifestations of hypothermia go, there are several important ones to be aware of. 02:47 First and foremost, patients with hypothermia are almost universally bradycardic. 02:52 Hypothermia down regulates the metabolism, slows everything down and these patients will almost always have a slow heart rate. 03:00 Hypothermia also irritates the myocardium and could precipitate both atrial and ventricular dysrhythmias these are non-uncommon in severely hypothermic patients. 03:10 Patients are very often hypotensive because of the impaired cardiac output associated with hypothermia and you may see conduction disturbances on their EKG's, atrial/ventricular blocks, etc. 03:22 One important cardiac manifestation of hypothermia to be aware of is the Osborn or J-Wave and this is the classic finding in severe hypothermia. 03:33 I think it's actually bet on every board exam ever made by man. 03:37 So, what the J-Waves are, are broad deflections at the junction of the QRS complex and the T-Waves so basically their additional waves that's kinda slur the down stroke of the QRS complex as it goes into the T-wave and you can see them to note on this EKG with the green arrows. 03:56 This can be mistaken for ST segment elevations and there's been a number of case reports of people mistaking Osborn waves for a STEMI and treating the patients is though they're having a heart attack. 04:09 I wanna emphasize that the treatment for this is rewarming, not anti-ischemic treatment, so these actually have no prognostic significance whatsoever, they do not indicate cardiac ischemia and they will completely go away ones the myocardium warms back up, so treat this with warming, don't send these patients to the cath lab, please. 04:31 All right, there's other elements of clinical presentation to be aware of, so from a vascular stand point patients will have peripheral vasoconstriction and that actually leads to relative central hypervolemia so while they're constricted at the periphery, they're gonna have a lot of blood supply in the central circulation which can lead to some difficulties. 04:54 They will almost universally have some degree of CNS dysfunction, typically, coma in the case of very severe hypothermia. 05:02 The patients very commonly will present with some degree of renal dysfunction so cold diuresis is an important phenomenon to be aware of, in the cold we increased our urine output and actually can become hypovolemic as a result of putting out a large volume of very dilute urine, so you wanna always consider the possibility of hypovolemia in your patients with hypothermia because of the renal effects. 05:31 And then from a pulmonary stand point patients will commonly have respiratory depression and hypercarbia associated with that but they can also develop non-cardiogenic pulmonary edema because of that relative central hypervolemia that we talked about earlier so basically all their circulating volumes is in the central circulation and if that is more than the central circulation can manage some it can extravasate out into the lungs. 05:57 So, when we think about hypothermia clinically, we stratify it into mild, moderate, severe and profound. 06:04 So patients with mild hypothermia have temperatures in the range of 33 to 35 so relatively minimal temperature reductions. 06:13 They're gonna generally be really, really shivering so these are the people who are coming in shaking continually, they may be a little bit off from a neurologic stand point, may be a little dysarthric or ataxic and interestingly from an affect point of view they often are kinda really don't care that much about what's going on with them so they start to develop apathy and this is actually, a, one of the adverse behavioral effects of hypothermia because they don't really care that much at that point about getting to a warm location. 06:44 Patients with moderate hypothermia are those who have temperatures between 29 and 32 degrees and at this point they'll stop shivering so you're only gonna be able to maintain shivering down to a temperature of 32 or 33. 06:58 Patients will begin to develop worsening altered mental status, you'll starts to see pupillary dilation, you'll definitely see bradycardia and you might begin to see some atrial dysrhythmias and you're gonna start to see a little bit of respiratory depression at these temperatures. 07:16 As we move in to severe hypothermia these are temperatures between 22 and 28 degrees. 07:21 Patients will universally be comatose and they often are gonna completely lose their reflexes, their voluntary motion. 07:28 This is the temperature range at which you might see a ventricular dysrhythmias, you'll almost always see significant hypotension because the cardiac output will be markedly decreased and you're also gonna see non-cardiogenic pulmonary edema. 07:42 Patients with profound hypothermia are those under 22 degrees. 07:46 And these patients will appear for all intents and purposes dead, all neurologic signs of life are absent, they are very commonly apneic, they may present with asystole or such profound bradycardia, that there all for intents and purposes, asystolic, so these patients really are very difficult to distinguished from patients who are in fact dead.
About the Lecture
The lecture Accidental Hypothermia: Symptoms by Julianna Jung, MD, FACEP is from the course Toxicologic and Environmental Emergencies. It contains the following chapters:
- Accidental Hypothermia
- Symptoms of Hypothermia
Included Quiz Questions
Which of the following risk factors for hypothermia is not due to decreased heat production?
- Burns
- Adrenal insufficiency
- Hypothyroidism
- Hypoglycemia
- Immobility
What is the classical EKG finding in severe hypothermia?
- Osborn waves
- De Winter pattern
- Pathologic Q waves
- U-waves
- Peaked T waves
What is the degree of severity of hypothermia in an apathetic, shivering patient noted to have a body temperature of 35 degrees celsius?
- Mild hypothermia
- Normal
- Moderate hypothermia
- Severe hypothermia
- Profound hypothermia
At what degree of severity of hypothermia will shivering cease?
- Moderate hypothermia
- Mild hypothermia
- Profound hypothermia
- Severe hypothermia
- Shivering will be present all throughout
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |