Playlist
Show Playlist
Hide Playlist
Accidental Hypothermia: Management
-
Emergency Medicine Cold Illness.pdf
-
Download Lecture Overview
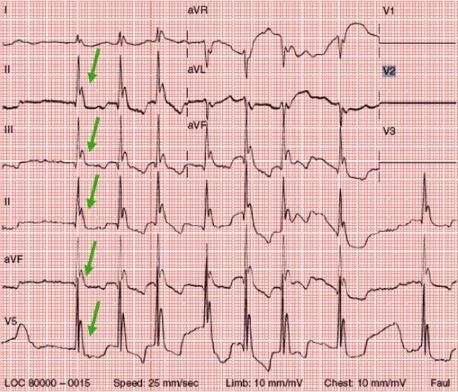
00:01 So how do we manage hypothermia? One of the really important things to remember is these very patients I was just telling you about who appear for all intents and purposes dead? They can actually survive in some cases. 00:13 So even patients who are stiff, blue, pulseless, apneic, no signs of life whatsoever. 00:21 They actually can come back to life with rewarming. 00:24 Patients have survived core temperatures as low as 14 degree celsius. 00:28 That is incredibly cold. 00:30 And the thing to remember about hypothermia is that it's neuroprotective. 00:34 So not only have patient survived from very severe levels of hypothermia, patients have survived neurologically intact which is kind of amazing. 00:43 So there’s a saying in emergency medicine that you’re not dead until you’re warm and dead. 00:48 So basically, we should never give up on a hypothermic patient until we’ve warmed them up to a reasonable physiologic temperature. 00:57 And speaking of cardiac arrest in our hypothermic patients, there are few modifications that you wanna consider in a hypothermic patient. 01:06 One is that we normally only give ourselves 10 seconds to decide if a pulse is present, but in hypothermia, we should give ourselves up to 60 seconds. 01:15 It can be much, much more difficult to detect the pulse in a hypothermic patient because it’s gonna be slow and it’s gonna be weak. 01:22 So give yourself enough time to decide if the patient has a pulse or not before initiating CPR. 01:28 You actually might wanna use a hand held doppler or an ultrasound device to verify the presence of a pulse if you’re having difficulty palpating. 01:35 Ultrasound is also very useful to look for cardiac motion before you start chest compressions. 01:41 And the reason that we wanna to be a little bit circumspect about starting chest compressions in our cardiac arrest victims is that any kind of rough handling or jostling of hypothermic patients can actually precipitate dysrhythmias. 01:54 So we really wanna be sure our patient needs CPR before we implement it. 01:58 From the airway and breathing standpoint, we should manage the airway as normal, just like we would for any other patient with coma or respiratory depression. 02:06 When we give supplemental oxygen, we wanna make sure that we warm it up. 02:10 So we wanna not give the patient cold or room temperature oxygen but wanna use oxygen to help warm their lungs and hopefully raise their core temperature. 02:20 We do wanna remember that the pulse oximeter is not typically gonna be able to detect the waveform. 02:25 So pulse oximeters rely on capillary pulsations in your fingertips and if you’re very vasoconstricted in the periphery which you are if you are profoundly hypothermic, you’re not gonna have capillary pulsations for the machine to detect. 02:39 So this is a situation where your pulse isn't really gonna help you and you might need to obtain an arterial blood gas to assess your patient’s oxygenation. 02:48 Defibrillation, if it's necessary for a ventricular dysrhythmia should be performed as normal. 02:53 But it is important to remember that it might actually not work until you get the core temperature up above 30. 02:59 The heart simply is not receptive to electrical stimulation at very low temperatures. 03:05 So as you may imagine, the treatment of hypothermia is gonna be to warm the patient back up and you’ve got three options for how you rewarm your patient. 03:16 You can do passive external rewarming, active external rewarming or active core rewarming. 03:22 And we’ll talk about each of those. 03:25 The passive external approach basically just involves getting rid of wet clothing and covering the patient up with an insulating material like a blanket. 03:33 You also wanna get him out of the cold and get him into a warm environment. 03:37 Now, this is pretty straight forward and it’s really only used in mild hypothermia or in situations where active rewarming is impossible for one reason or another. 03:46 Maybe you’re in a wilderness setting or something like that where you can’t get the patient to an active rewarming location. 03:54 For more severe hypothermia, we’re always gonna use active techniques and that’s gonna involve not just insulating the patient but actually heating them back up. 04:03 So we’re gonna use heating pads or heated blankets. 04:06 There are forced air rewarming systems, the one that’s commonly used in the US it’s called the Bair Hugger. 04:12 But there are basically different blankets that will blow warm air through the system and rewarm the patient that way. 04:18 And then you can also use radiant heat lamps. 04:22 When you use active external rewarming, one of the really important things to remember is to try to preferentially put the warming devices on the patient’s torso rather than the limbs. 04:32 And that’s because of phenomenon called core temperature afterdrop. 04:36 Remember, the periphery is very vasoconstricted and as a result of that it's very cold. 04:42 So if you warm up the extremities, you’re gonna basically start vasodilating those extremities, and you’re gonna allow an influx of cold blood from cold extremities to come back to the central circulation. 04:56 That can actually reduce your core temperature rather than bringing it up. 05:00 So you wanna make sure that you get the torso warm first and don’t worry as much about the extremities until you've reached a more reasonable core temperature. 05:11 Of course, for very severe hypothermia, we’re gonna use active core rewarming techniques. 05:16 And that basically involves any introduction of anything that’s warm inside of the body. 05:23 So something as simple as warm humidified oxygen actually counts as active core rewarming. 05:28 Use of warm IV fluids is another commonly used technique. 05:32 There have been reports of use of bladder and gastric irrigation. 05:37 These are kind of questionable techniques with a little bit of controversy around them. 05:44 It’s not clear how effective they are and there may be some morbidity associated with them. 05:49 But it is an option that's available to you if you don’t have other alternatives. 05:53 You can also use peritoneal dialysis with warm dialysate. 05:57 A common technique that's used in hypothermic cardiac arrest is closed thoracic lavage. 06:03 Where you basically put two chest tubes in the patient's two large diameter chest tubes and you use one to put warm sterile saline in and you use the other one to drain it back out, and you basically just have a continuous circuit where you introduce warm fluid into the thoracic space in order to rewarm the heart. 06:26 Really the gold standard of active core rewarming is extracorporeal blood rewarming which can be conducted on a cardiac bypass circuit. 06:34 This is obviously technically challenging and difficult but for patients with a cardiac arrest or profound hypothermia, it’s something that’s definitely worth pursuing. 06:44 So again, active core rewarming is mandatory for any patient who is unstable or has severe to profound hypothermia and the technique that you employ is gonna depend on what’s available in your local setting, and how sick the patient is. 07:00 In terms of general management for patients with hypothermia, I already mentioned this, but you wanna minimize any kind of rough handling of the patient, because there have been case reports of patients developing cardiac dysrhythmias as a result of being excessively jostled or manipulated. 07:17 You wanna make sure that you provide adequate volume resuscitation. 07:20 These patients are commonly hypovolemic because of the cold diuresis we mentioned. 07:25 All their IV fluids should be warmed. 07:28 You may need to use vasopressors for severe shock. 07:32 However, they’re often ineffective. 07:34 Really the treatment for shock is gonna be rewarming rather than medication or fluid. 07:41 Dysrhythmias also will typically respond to rewarming and you really only should treat unstable rhythms with the understanding that it may not work until you get the patient up to a more normal body temperature. 07:52 And then of course, all patients with severe hypothermia should be admitted typically to an ICU setting.
About the Lecture
The lecture Accidental Hypothermia: Management by Julianna Jung, MD, FACEP is from the course Toxicologic and Environmental Emergencies.
Included Quiz Questions
Which of the following statements regarding the management of hypothermia is INCORRECT?
- If there is no palpable pulse after 30 minutes, start CPR
- Use of a handheld doppler may be useful to determine presence of a pulse.
- Provide warmed oxygen via endotracheal tube or bag-valve-mask device.
- Defibrillation may not work until core temperature is more than 30 degrees Celsius.
- Intubate patients with hypothermia as you would someone in a coma or who has respiratory depression.
What is the gold standard of active core rewarming in severe hypothermia?
- Extracorporeal blood rewarming
- Peritoneal dialysis
- Warmed IV fluids
- Closed thoracic lavage
- Gastric irrigation
Which of the following rewarming techniques is NOT an example of active external rewarming?
- Peritoneal dialysis
- Heated blanket
- Heated pad
- Radiant heat lamps
- "Bair Hugger"™ forced air rewarming system
What is the management of stable dysrhythmias in the setting of hypothermia?
- Rewarming
- Defibrillation
- Cardioversion
- Amiodarone
- Verapamil
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |