Playlist
Show Playlist
Hide Playlist
Vessels: the Wall of an Artery and Vein
-
Slides 02 Human Organ Systems Meyer.pdf
-
Reference List Histology.pdf
-
Download Lecture Overview
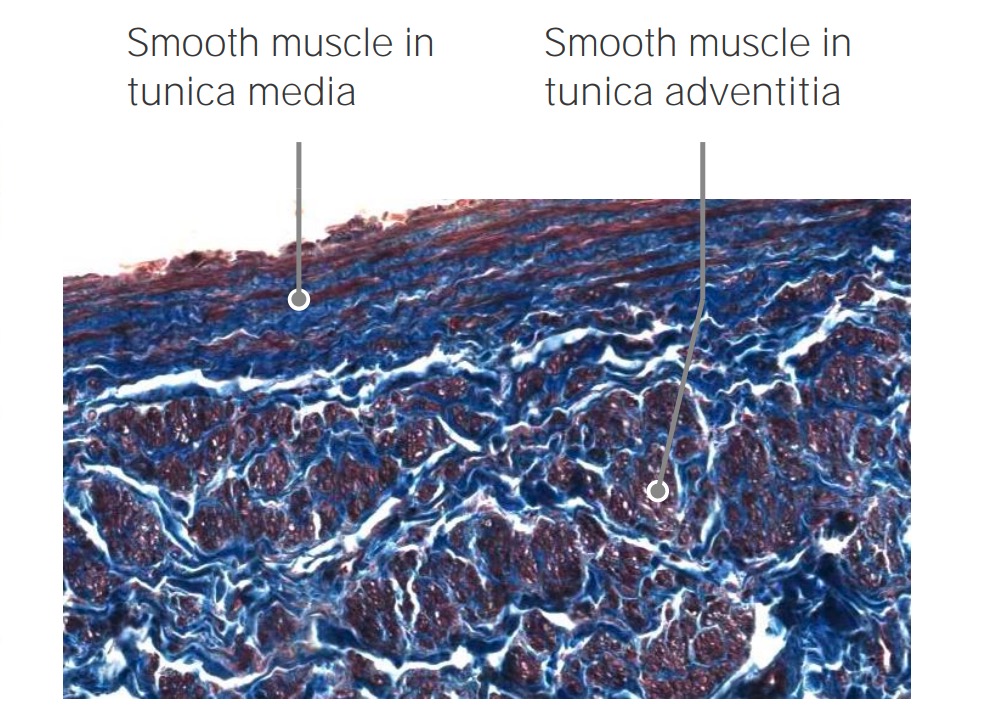
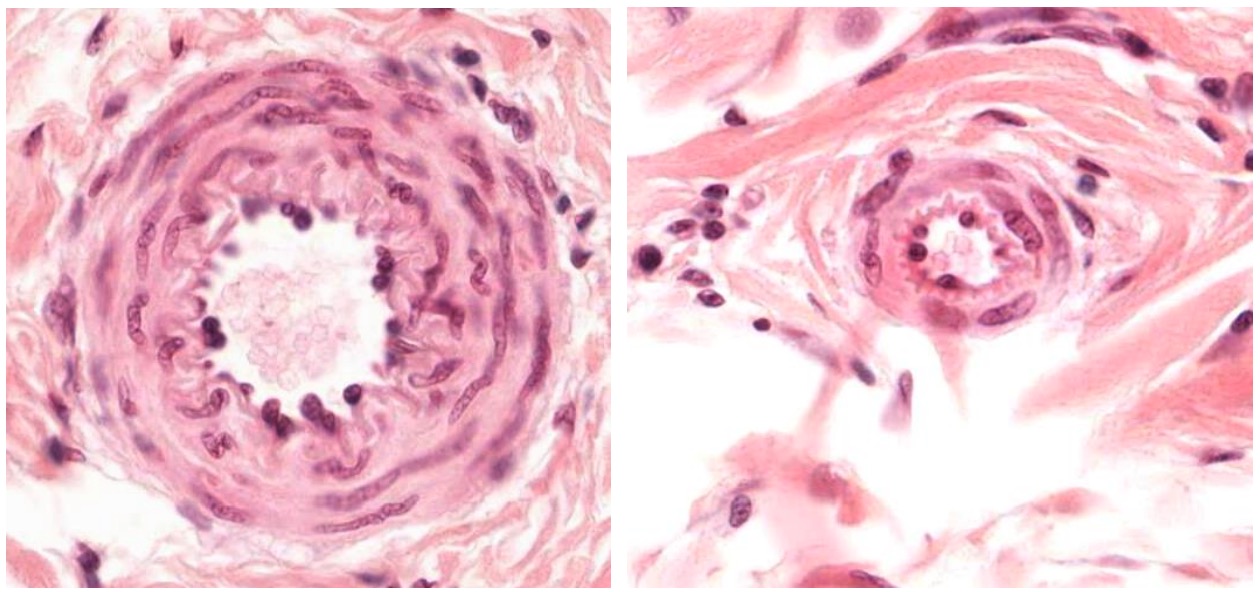
00:01 Well, when we have a look at an artery or a vein, we need to understand something about the pressure within those vessels. On the right hand side of this slide, you can see a diagram illustrating the main pressure within these vessels as they pass from the aorta and then down to a capillary bed then into small venules and then into veins to be returned to the heart. And when the heart pumps, the pressure is called the systolic pressure, and the average is around 120 millimeters of mercury. 00:44 And then when the heart goes to a resting phase or a filling phase, pressure drops in these vessels down to about 80. And that’s called the diastolic pressure. And that changes the pressure within the arteries. And as you see down the bottom, there is a section of arteries that there is classifications ranging from the aorta, arteries, arterioles, etc to the capillary beds. And what I want you to notice is that the aorta has a very thin wall relative to the size of its lumen. And I’ll explain why that occurs or why that is later on in the lecture. Within the arteries and small arterioles have a thick wall, and they’re circular in profile. That’s because they were standing or at least they have the high pressure inside them as they pass blood down to all the tissues in the organs of the body. And once the blood then gets into the capillary bed and beyond, the pressure is very low. So one way in which you can tell the difference between the artery and the vein or small veins is that, bear in mind, the pressure difference, because an artery is acting under a fairly high pressure, the lumen is going to be usually nice and circular. As you see here in the image, here is the section through the artery. It’s got a nice circular profile because the pressure of the blood inside it, passing down through the tissues. If you look at the vein, however, right next to it, the lumens collapse down because it’s acting on a very low pressure and only opens up and transmits the blood forward when it’s needed to, to return it back to the heart. Sometimes veins are mere storage units, storing blood, and then it’s returning that blood intermittently back to the heart. But because their pressure is very low, they normally collapsed. In the diagram, have a look at the luminal aspect of a vein. And usually, the lumen is larger relative to the wall of its lining, and the actual ratio or rather the comparison between the relative thickness of the wall of the aorta or an artery compared to the lumen is a lot thicker. In a vein, the relative thickness of the wall of the vein relative to the size of the lumen of the tube, is a lot smaller. 03:42 In this section, there is also a section through a nerve fascicle. This section is taken through, perhaps, part of the limb of the body, and you’re looking at a fairly large artery, a fairly large vein, and a nerve bundle. Those of you who do anatomy will understand that usually, when you’re passing down through the limbs, arteries, veins, and nerve bundles accompany each other surrounded by connective tissue, which is the green colored staining component you see in this section. That happens to be collagen. So let’s look now at the layer of a typical artery and a vein. Here, it’s easy to describe the wall of an artery, because some of the components of the wall are a little bit more obvious than you see in a thinner wall of a vein. On the right-hand side, is a diagram that you can use to then try and work out or make sure you can consolidate your understanding of the wall of a typical blood vessel. Let’s have a look at the section of the artery on the left-hand side. 05:02 It’s stained to show a number of different components that I will point out. On the top left-hand side of the section, is the lumen of the blood vessel. You can only see a very tiny bit of clear part of this lumen. Well, the layer of the blood vessel closest to the lumen is called the “tunica intima.” Tunica just means a layer or a coat. Intima, it’s the most intimate layer in relation to the lumen of the blood vessel. The middle layer is called the “tunica media.” The tunica media has a little star next to it or an asterisk. 05:47 And that is to remind you that this is the coat, this is the layer of the artery that changes significantly. And it changes because of the different roles this coat has in cardiovascular function. This layer is contractile. It can change dimensions. And that’s very important particularly in arteries because you can distribute blood to various parts of the body by opening that wall or relaxing that wall to increase the lumen diameter. If you get up and walk around or run, the blood vessels, the arteries going to your limbs, your lower limbs particularly, are going to open up so that you can perfuse your skeletal muscles with a lot more blood, so this tunica media can relax. And therefore, widen the lumen, allow more blood to flow through. Conversely, when you want to diverge blood away from certain parts of the body, then that layer can contract, smaller lumen, therefore, less flow of blood. And that contraction and relaxation can be controlled by nerves of the autonomic nervous system or other factors that again, we’ll talk about in later lectures. So it’s a very, very important layer. 07:18 On the outside, the third layer is the tunica adventitia. It’s connective tissue. 07:24 Here, it’s fairly dense connective tissue, mostly collagen. That’s an important layer for a number of reasons. Most importantly, it strengthens the wall of the artery. So on the very high blood pressure, the artery doesn’t rupture. It also blends the artery with surrounding tissues. So often, the junction between what we call the tunica adventitia and surrounding connective tissue is often hard to find and really not necessary. Think back at the slide previously where I explained the neurovascular bundle, the artery, the vein, and the nerve wrapped up by connective tissue in a component or perhaps a limb. It’s very hard there to distinguish where the tunica adventitia ends and where the connective tissue wrapping around the artery, vein, and nerve begins. Now, often inside large arteries in particular, there is a little layer of elastic tissue called the “internal elastic lamina.” If you look carefully at this slide, you can see this little wiggly line, clear wiggly line running through. That’s the internal elastic lamina. On the outside, there is also an external elastic lamina that separates the tunica media from the tunica adventitia. 09:00 And if you look very carefully in the tunica adventitia, you can make out some little pink dots. They represent elastic tissue. You can’t see them very clearly, but there is elastic tissue through most arteries. In one artery, in particular the aorta, that elastic tissue dominates for a reason I’ll explain later on. Now, this is a good stain to show you the components of an artery, and similarly, a vein, because it shows you smooth muscle. 09:34 Smooth muscle is the brownish component you see making up the wall of the tunica media. 09:41 And the other stain, the greeny colored stain is the collagen. So the important thing to understand here is that the tunica media is made up of a combination of smooth muscle and collagen. There is also elastic tissue there, but in minimal amounts. And all these three components help to enable the blood vessel wall to relax or contract because of the presence of smooth muscle that I explained earlier, but the collagen strengthens the blood vessel as well so it doesn’t rupture. And the elastic tissue allows some aspect of recoil or stretching. But this stain is a good one to show that. One important point to understand is that some of you may recall or remember from your previous studies of connective tissue, for instance, that fibroblast lay down collagen and elastic tissue. 10:45 Well, in the case of an artery and a vein, those connective tissue components, collagen and elastic tissue, is actually made by the smooth muscle cell. And as we’ll look at the other lectures later on in this histology course, you’ll realize that lots of other cells too make collagen fibers and elastic fibers. But here, importantly, it’s a smooth muscle that has that job.
About the Lecture
The lecture Vessels: the Wall of an Artery and Vein by Geoffrey Meyer, PhD is from the course Cardiovascular Histology.
Included Quiz Questions
The peak aortic pressure during the opening of the aortic valve is best known as which of the following terms and should normally be lower than which of the following values, respectively?
- Systolic pressure, 120 mm Hg
- Diastolic pressure, 80 mm Hg
- Systolic pressure, 80 mm Hg
- Diastolic pressure, 120 mm Hg
- Mean arterial pressure, 100 mm Hg
Which of the following statements regarding the histologic features of the arterial wall is MOST ACCURATE?
- The layer of tissue that forms the outermost portion of the tunica intima is the internal elastic lamina.
- It is easy to differentiate tunica adventitia from tunica media and also surrounding connective tissue that binds the artery to adjacent structures.
- The tunica intima is usually as thick as the tunica media.
- The external elastic lamina separates the tunica adventitia from surrounding connective tissue that binds the artery to adjacent structures.
- The thinnest layer is the tunica media.
Which of the following vessels has the thickest wall?
- Aorta
- Femoral vein
- Dorsalis pedis artery
- Inferior vena cava
- Renal artery
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |