Playlist
Show Playlist
Hide Playlist
Varicella Zoster Virus Infection (Chickenpox and Herpes Zoster) in Darker Skin
-
Slides Varicella Zoster Virus Infection in Darker Skin.pdf
-
Download Lecture Overview
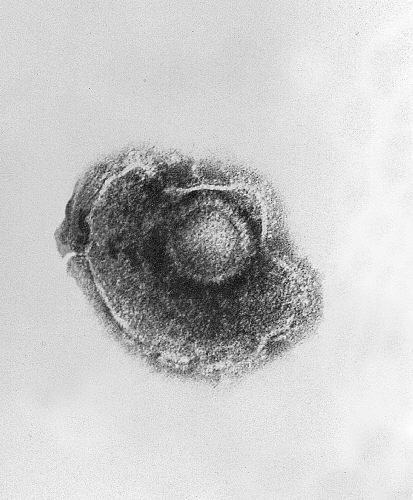
00:01 Welcome to our lecture on varicella zoster virus. 00:08 Varicella zoster virus causes two clinically distinct diseases. 00:13 First one is varicella or chicken pox. 00:16 It's primary infection with the varicella zoster virus. 00:20 It's relatively mild, self-limited, and is a childhood illness. The second one is herpes zoster, which we call shingles and results from reactivation of the latent varicella zoster virus. 00:36 The incidence of chicken pox is in decline since the introduction of widespread pediatric immunization. 00:45 Herpes zoster incidence increases with advancing age. 00:49 As a consequence of declining immunity, older black adults are up to 75% less likely to develop herpes zoster compared to older white adults. 01:03 So let's talk about the pathophysiology of varicella zoster virus. 01:08 We will start with the first exposure to varicella zoster virus which usually occurs in early childhood. Varicella zoster virus is usually transmitted via respiratory route through droplet spreads for example coughing. 01:22 It can also be transmitted via direct contact with lesions, but this route of transmission is far less common. 01:31 Initially, the virus infects T cells, which are located in the nasopharyngeal lymphoid tissue. 01:38 Replication time within the lymphoid tissue or incubation period lasts about 10 to 21 days. With increasing viral particles, they spread throughout the body and the skin starts developing the rash. This is what we call chicken pox. 01:57 As I already mentioned, this only happens with first contact with varicella zoster virus, which is usually seen in childhood. 02:06 During this time, ZV virus also infects nerve endings and moves retrograde along sensory axons to establish lifelong latency in neurons within the original ganglia. 02:22 In an immunocompetent child, there is a rapid response to the virus, thus resulting in inhibition of viral replication and further spreading. Clinically, the rash resolves. 02:34 However, the virus remains dormant in the ganglia. 02:40 Subsequently, triggers like illness, stress, etc. can cause reactivation of the virus. 02:48 Then the virus starts replicating in the peripheral neurons. 02:54 Viral particles then start to migrate alongside sensory nerves, infecting skin in the specific dermatomes, and that is how herpes zoster or shingles develops. 03:06 I hope you understand that pathogenic mechanism. 03:10 Right. We spoke about the etiology. 03:12 Now we're going to speak about the clinical manifestations. 03:15 It commonly occurs during childhood usually benign and self-limiting illness. Varicella presents as vesicular eruption consisting of delicate teardrop vesicles on an erythematous base. 03:29 Do remember, though, that in skin of color this may be more dusky than erythematous. These lesions have central distribution. 03:37 They are denser on the trunk and face. 03:40 There's less lesions peripherally, and it can also affect the conjunctiva in the mouth. There may be low grade fever, malaise, and headache, but these are generally present but tends to be very mild. Now let's take a look at shingles. 03:59 The usual problem is pain, which occurs one to several days before the skin eruption. These symptoms can also appear simultaneously or even after the skin eruption initially presents as papules and plaques of erythema in the affected dermatome. 04:20 Within hours, the blisters develop over erythematous plaques. What are some of the complications? Chronic pain (post-herpetic neuralgia_, that's a term that we use for the pain. Cranial nerve palsies, zoster paresis, meningoencephalitis and varicella gangrenosa, which is quite rare. So how do you make a diagnosis of varicella zoster infections? The clinical examination and history are usually enough for diagnosis. 05:01 Laboratory testing is also used in cases of uncertain clinical presentations, more so if it's hemorrhagic and it's a presentation that is not typical, which usually occurs in immunocompromised individuals. 05:18 PCR testing is the gold standard. 05:21 Viral cultures are used for testing resistance to antiviral drugs. 05:28 So what is the differential diagnosis? Herpes simplex is usually more limited and often crosses the midline. 05:36 Bullous impetigo is also another differential, tends to be more superficial with vesicles and bullae that break and form desquamating edges, as well as honey colored crusted lesions. 05:49 So how do we manage these patients? We use antivirals as listed over there. 05:54 And sometimes we use varicella zoster immune globulin. 05:58 And this is indicated for administration to high-risk individuals within ten days, ideally within four days of chickenpox.
About the Lecture
The lecture Varicella Zoster Virus Infection (Chickenpox and Herpes Zoster) in Darker Skin by Ncoza Dlova is from the course Viral Skin Infections in Patients with Darker Skin.
Included Quiz Questions
What are the two distinct clinical diseases caused by the varicella zoster virus?
- Varicella (chickenpox) and herpes zoster (shingles)
- Herpes labialis and herpes genitalis
- Roseola infantum and erythema infectiosum
- Molluscum contagiosum and warts
- Hand-foot-mouth disease and herpangina
What is the correct sequence of events in varicella zoster virus infection from initial exposure to reactivation?
- Infection of T cells in nasopharyngeal lymphoid tissue → viral spread to skin → infection of nerve endings → establishment of latency in dorsal root ganglia → reactivation in specific dermatomes
- Direct infection of skin cells → systemic viremia → immune response → clearance from body → reinfection years later
- Infection of respiratory epithelium → spread to lymph nodes → viremia → clearance by antibodies → reinfection with different strain
- Ingestion of virus → gastrointestinal replication → hematogenous spread to skin → complete viral clearance → new infection in adulthood
- Conjunctival inoculation → spread to cranial nerves → generalized rash → development of immunity → loss of immunity with age
Which of the following best describes the characteristic distribution pattern of varicella (chickenpox) lesions?
- Denser on the trunk and face with fewer lesions peripherally (centripetal distribution)
- Limited to a single unilateral dermatome that rarely crosses the midline
- Generalized with equal distribution across all body surfaces
- Primarily affecting the extremities with sparing of the trunk
- Concentrated in flexural areas such as axillae, groin, and antecubital fossae
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |