Playlist
Show Playlist
Hide Playlist
Uterine Tube – Female Reproductive System
-
Slides 09 Human Organ Systems Meyer.pdf
-
Reference List Histology.pdf
-
Download Lecture Overview
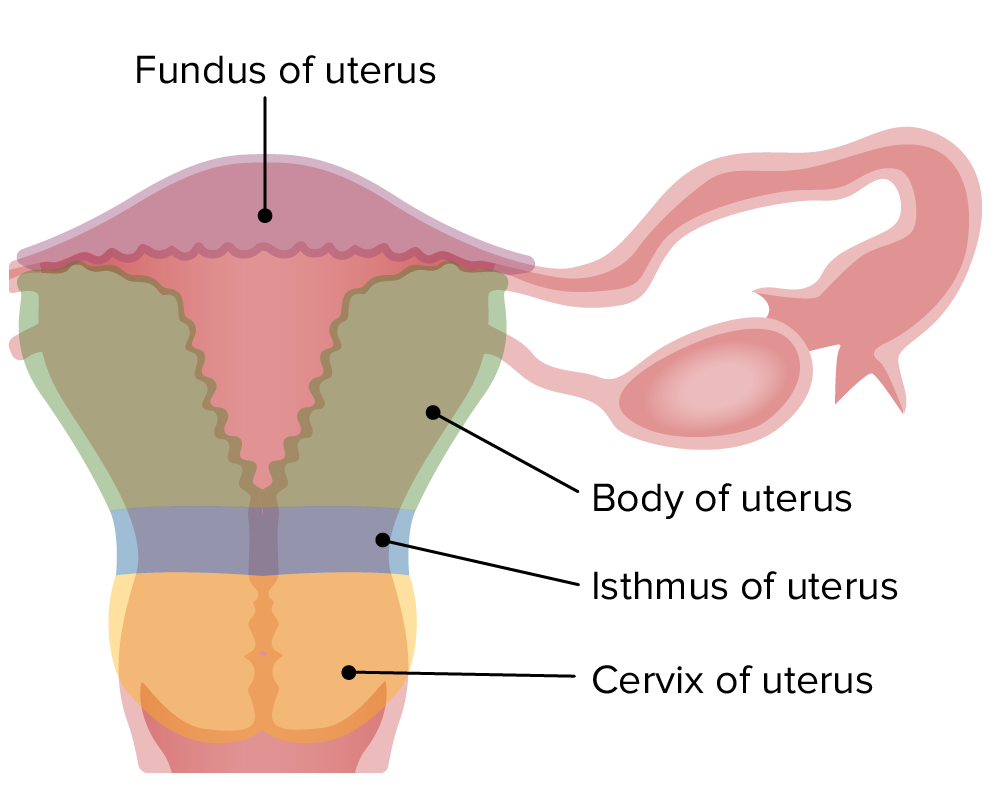
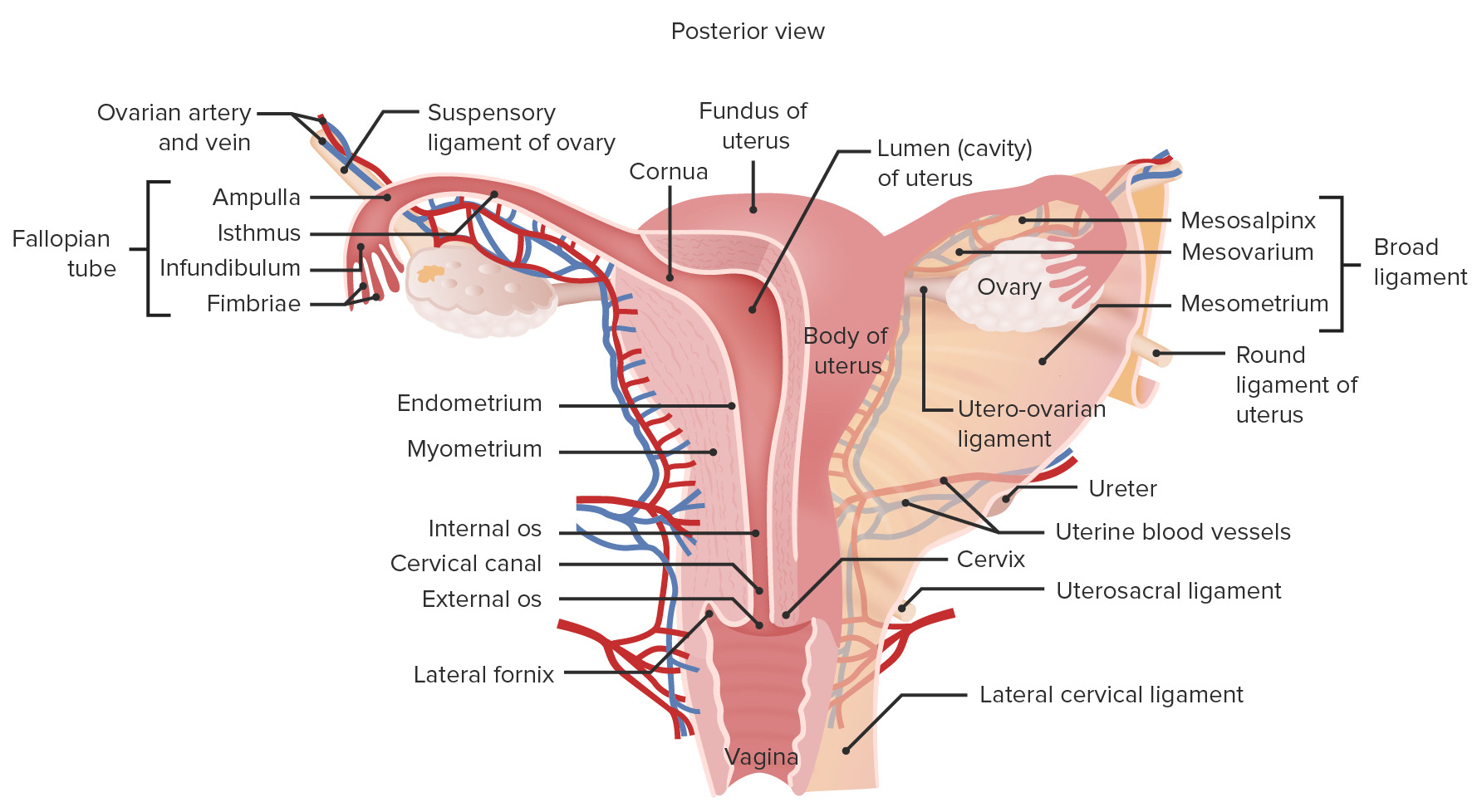
00:00 start off first with looking at the uterine tube. Just to remind you of the structures associated with the female reproductive system, cast your eyes on this diagram here. 00:15 Try to focus on, first of all, the orientation. At the base of the diagram is the bladder, the large round yellow structure in this diagram. And on the right-hand side of the bladder, or I should say on the posterior part of the bladder, is the vagina. And you can see the vagina is continuous with the cervix, and then the uterus, a large pear-shaped organ. And then you can see the lumen, colored in bright red of the vagina and the cervix and also the uterus, being continuous with the lumen of the uterine tube, which is going to be the topic of our first organ in this lecture. That uterine tube lies very close to the ovary. 01:03 The ovary is colored in blue here. Now, the anterior portion of the body is on the left-hand side. The posterior part of the body is on the right hand side. And not shown in this slide, but right next to the vaginal passage will be the rectum. So make sure you can orientate yourself and make sure you’re now aware of the location and continuity of each of the organs that we’re going to discuss in this lecture. The uterine tube is shown here on the diagram. It’s between 10, 12 centimeters long. Focus on the diagram, and then I will talk more about the histological structures of the uterine tube on the histological sections also contained on this slide. The uterine tube is divided into four different components. 01:58 They’re named there, the infundibulum, which is the end part of the uterine tube, which has these very numerous branches of mucosa called fimbria. The fimbriae are actually extensions of the mucosa, and they become almost like erectile tissue at the time of ovulation. And they are going to actually wrap around the ovary, or very close to the ovary, to optimize the chance that the ovulated oocyte will pass into the uterine tube. 02:34 The next part of the uterine tube is the ampulla. This is by far the longest part of the uterine tube, and it is the site where fertilization occurs. And then there’s a very small portion, the isthmus, which is very close to the entry into the uterus, and then a small interuterine component or segment also labelled. So make sure you now understand that there are these four components to the uterine tube. And before we go any further, let us just recall that at ovulation when the oocyte is released, it is still yet to complete its second meiotic division. It has been sitting in the ovary possibly for 50 years because, as you may know, these oocytes develop from oogonia prior to fetal life. And although there is a lot of atresia, at the time of birth, you may have only 400,000 to 500,000 of these oogonia remaining in the ovary. And they sit there for a very very long time during the reproductive life of the female, which can last until the age of about 47 to 55. So really, one of these oocytes that is ovulated may be 50 years old. And because of that, and because it’s arrested in the second meiotic division, during that long time, there is a possibility of errors in the meiotic division process. And this can give rise to anomalies, such as nondisjunction arising, for instance, in the trisomy of chromosome 21 or Down syndrome. So, it’s important to understand that there is this long arresting of the oocyte in the second meiotic division. 04:44 And it’s only after fertilization that meiosis is then completed. Well, what happens now is that the oocyte enters into the uterine tube. And on this slide, you can now see there are three sections through the uterine tube. The top left section is the uterine tube cut in very low magnification. And you can see various components in a high magnification. 05:12 The uterine tube has a very thick muscular wall. That muscular wall or the muscularis creates peristaltic contractile activity that can move fluid and content such as sperm from the uterine end of the uterine tube up towards the ampulla where fertilization may occur. 05:35 So it enhances movement of the sperm up to that region. Conversely, the peristaltic wave of this muscle can work in the opposite direction after fertilization and enhance the transport of the fertilized egg towards the uterus for implantation. At the high magnification, you can see details of the mucosa. The mucosa is a very folded epithelial surface. 06:06 Remember the term mucosa refers to an epithelial surface, and it’s supporting lamina propria in a tube that is exterior to the body, that opens exterior to the body. And if you think about the anatomy of the reproductive system I described earlier, this tube does eventually lead to the outside of the body. The epithelium has two sorts of cells. It has a ciliated cell. 06:33 You can see the cilia here. And a little dark pink line running along the surface of these cells are the basal bodies in which these cilia are attached, and they all beat together to move fluid along, and to move the oocyte along, and also the sperm along so they meet each other for fertilization. Besides being an organ for transport and providing a location for fertilization, it’s also a very important tissue for making sure there is nutrition inside the lumen for the oocyte, the sperm, and also for the possibility of the fertilized egg. And they are called secretory cells or peg cells. Now, before we move on to looking at the uterus, the uterine tube also undergoes changes during the cycle. At around the time of ovulation, these ciliated cells, and the peg cells are maximum in number, and they can be as much as 30 microns in height. And during periods of nonovulatory phases of the ovarian cycle, such as the follicular phase and the luteal phase, these various cells can be reduced to half their height and they can lose the cilia and become non-secretory. 08:02 It’s only after the influence of estrogen and progesterone that they reach their optimal state of activity at the time of ovulation. Estrogens actually create ciliogenesis in the ciliated cells, so they acquire cilia and more cilia at the time of ovulation. 08:22 And progesterone stimulates the secretion of the peg cells to produce the nutritious fluid that we spoke about earlier. I want to move on now to discuss the uterus. And again on this
About the Lecture
The lecture Uterine Tube – Female Reproductive System by Geoffrey Meyer, PhD is from the course Reproductive Histology.
Included Quiz Questions
Which of the following regarding the anatomy of the female urogenital anatomy is MOST ACCURATE?
- The rectum lies posterior to the vagina.
- The uterus is anterior to the vagina.
- The bladder is superior to the vagina.
- The lumen of the cervix leads directly into the lumen of the uterine tube.
- The uterus is inferior to the bladder.
Which of the following regarding the fallopian tube is MOST ACCURATE?
- The ampulla is the most common site for fertilization.
- Mucosal folds called fimbriae extend from the isthmus.
- The infundibulum attaches to the uterus.
- Meiosis is completed at ovulation
- The ampulla lies between the isthmus and the intramural sections.
Which of the following statements regarding the structure and function of the fallopian ("uterine") tube is INCORRECT?
- Progesterone increases the secretory activity of ciliated columnar cells.
- Estrogen stimulates ciliogenesis.
- A peg cell is a non-ciliated epithelial cell within the fallopian ("uterine") tube.
- From outer to inner, the layers of the fallopian tube are the serosa, subserosa, lamina propria and mucosa.
- Peg cells contain apical granules and produce tubular fluid.
What is the approximate length of the fallopian tube in centimeters?
- 10–12
- 8–9
- 5–7
- 14–16
- 4–6
The fimbriae extend from which of the following portions of the fallopian tube?
- Infundibulum
- Interstitial segment
- Isthmus
- Ampulla
- Intramural section
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |