Playlist
Show Playlist
Hide Playlist
Urgent Urologic Disease
-
Slides UroUrgentDiagnoses AcuteCare.pdf
-
Download Lecture Overview
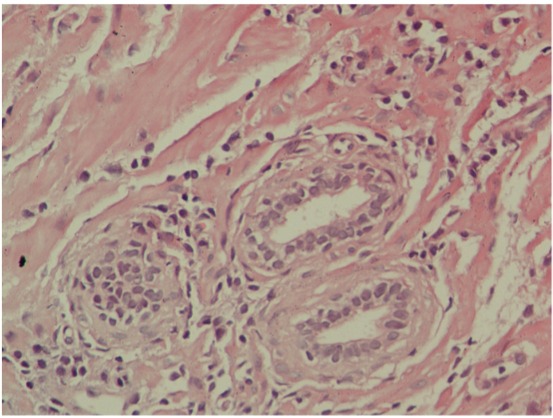
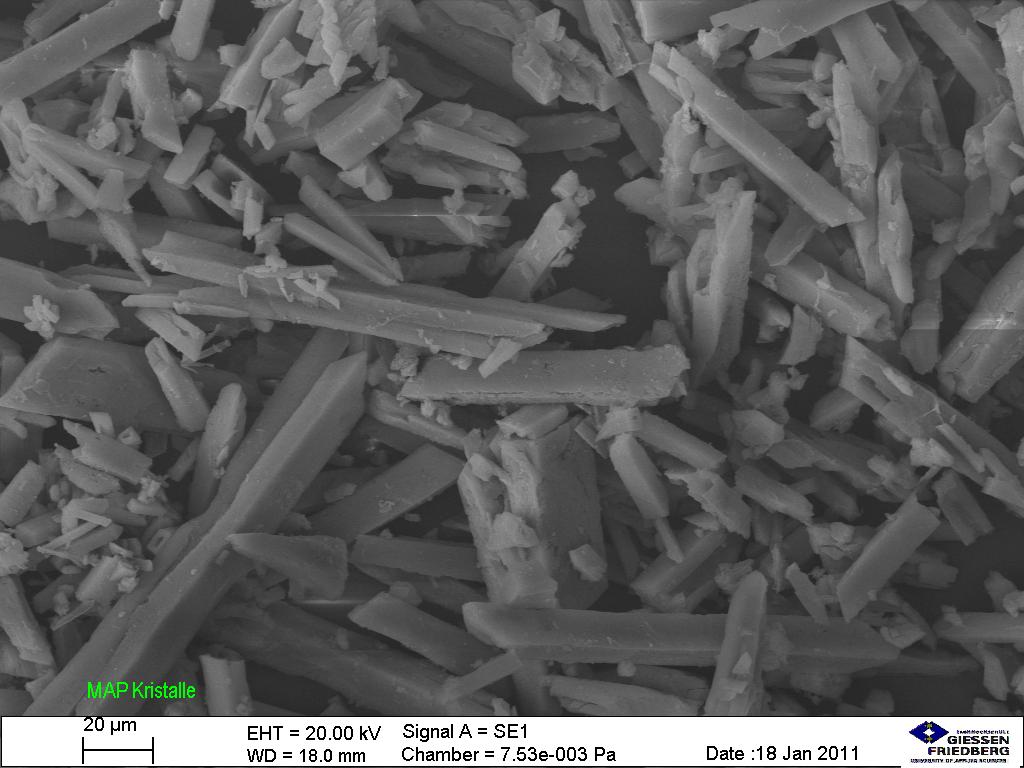
00:01 So, let's discuss urgent urologic issues. 00:05 And I'm going to highlight a couple that are important for your exam, but also very pertinent to direct patient care that I do in my practice. 00:13 And the first is going to be kidney stones, nephrolithiasis. 00:17 So, the lifetime prevalence of getting a kidney stone is 10 to 15%. 00:21 This is a really common disorder. 00:23 Good exam question, what's the most common type of stone found by far. 00:28 It's calcium oxalate. 00:30 But you can also see stones made of cystine or struvite if the patient has a history of recurrent urinary tract infection. 00:37 Or uric acid if they have a history of gout. 00:39 And just remember that kidney stones I think to me are the great pretender. 00:44 They can produce a flank pain that radiates down into the groin. 00:48 That’s kind of a classic. 00:50 But they can also present as a vague abdominal pain, an inguinal pain. 00:54 Therefore, they can mimic a bunch of other conditions. 00:56 So, stone is on the differential for a lot of different types of pain and patient problems. 01:03 But the workup is fairly straightforward. 01:05 Get a urinalysis. Of course, looking for blood. 01:08 But do remember that about 10% of cases of nephrolithiasis have a negative urinalysis for blood. 01:16 And that's why we get imaging. 01:18 And an ultrasound can be effective. 01:20 A lot times, I order a CT urogram which doesn't require contrast. 01:25 But both of these tests can help diagnose a patient with nephrolithiasis even regardless of what their urinalysis may show. 01:35 Do understand as well that sometimes the things that we do as physicians can promote stone formation, one of which is treatment with antibiotics. 01:44 So, those are sulfamethoxazole, amoxicillin, quinolones are all associated with a higher risk of stone formation. 01:51 For patients with diabetes, sulfonylureas can promote stones. 01:55 So can potassium-sparing diuretics. 01:57 Might be – use those in cases of heart failure. 02:00 And then laxatives which is, of course, a favorite among some of my older adults, can also be associated with stone formation. 02:06 Just something to keep in mind, particularly after that first stone is passed, maybe worthwhile to think about changing some of these drugs to prevent another stone from forming. 02:16 What do you do with the management of nephrolithiasis? Well, a smaller stone among patients who aren't pregnant, it’s usually just managed by hydration alone. 02:25 So, two liters or more than two liters every 24 hours, along with pain management with opiates. 02:32 Using calcium channel blockers or alpha antagonists may help the stone pass a little bit earlier. 02:38 So, if patients can tolerate that, particularly if they're really uncomfortable, that can be a good idea. 02:43 Not a role for corticosteroids among these patients with small stones. 02:47 And they usually do pass on their own. 02:49 After it's passed, make sure that you check basic metabolic panel. 02:54 You’re really looking for the creatinine and renal function, but really also at levels of potassium, levels of calcium, and make sure those are normal. 03:05 And then, in terms of preventing the next stone for patients, particularly for calcium oxalate stones, you shouldn’t be avoiding calcium. 03:14 Calcium supplements might actually help prevent stone and thiazide diuretics definitely can lower the risk of recurrence because they are actually taking back, within the nephron, calcium and re-absorbing that into the circulation. 03:28 For larger stones, stones that aren’t passing, more complicated stones, really beyond the scope of what we’re going to discuss today, but requires urological management. 03:37 So, you need a specialist on-board. 03:41 For prostatitis, this is a picture of the prostate. 03:44 Normal on the left, enlarged on the right, and that can be due to infection, but you could see just the scope of how big that gland can get. 03:52 It has a lot of room to grow. 03:54 And, obviously, when it does, it’s going to cause obstructive urinary symptoms. 03:58 And prostatitis is different from benign prostatic hypertrophy. 04:04 And it often is associated with pain as well. 04:07 So, I think the keys to understanding prostatitis, both for your knowledge and for the exam, is there are two prevalence peaks. 04:14 One during young adulthood and one during older age. 04:18 That said, E. coli is the most common organism. 04:21 But you see other organisms that are commonly implicated in urinary tract infection, also involved in causing prostatitis. 04:29 And this is another one that’s kind of hard to pin down because the pain is very difficult for patients to describe. 04:39 It's usually more dull, but then it can become sharp. 04:42 And the location is really tricky. 04:44 So, think about pain in any of those areas – superpubic, rectal, perineal can all represent prostatitis. 04:51 When you do the exam, this is one of the exams where a digital rectal examination is necessary. 04:57 I don't believe in the digital rectal examination for asymptomatic patients. 05:01 Doesn't really have the sensitivity to detect prostate cancer or colorectal cancer. 05:06 But if you have a patient with potential prostatitis, they absolutely need to have their prostate checked with a DRE. 05:12 But, however, in doing so, avoid vigorous prostate massage. 05:16 That can actually seed the bloodstream and therefore promote sepsis, so a really bad idea. 05:22 Just remember that the – even though the infection that may be there in the prostate doesn’t necessarily spread into the urine if it’s localized. 05:31 So, in about a third of cases, the urine culture is going to be negative. 05:35 And also, I'm pretty liberal in testing my patients for sexually transmitted diseases. 05:41 It's classically among patients who are a little bit younger, but people have sex their whole lives it turns out. 05:47 So, therefore, I'm always thinking, it doesn't hurt to get a culture or a DNA specimen for gonorrhea and chlamydia as well. 05:58 So, just to – again, a demonstration that the prostate can be large. 06:02 It looks painful from here. 06:04 Now, how do you treat it? For outpatients, usually giving a shot of ceftriaxone and doxycycline for 10 days is enough. 06:12 The other option is treat it like a urinary tract infection. 06:15 But again, I think the key difference between prostatitis and most urinary tract infections is the duration of treatment. 06:22 So, if you see that there, we think about – well, we’ll treat a urinary tract infection in a man for seven days. 06:31 For prostatitis, it’s 10 to 14 days because that infection is kept in the prostate. 06:37 It’s harder for the antibiotics to penetrate and, therefore, need more time with the antibiotics. 06:42 For inpatient treatment, don't treat a lot of inpatients for prostatitis. 06:45 But, say, they did develop sepsis related to their prostatitis, they should definitely come in. 06:50 You can still use a quinolone. 06:51 It doesn't – and oral and IV are really equivalent with quinolones. 06:56 But for more severe – some severely ill patients, broad coverage, piperacillin, tazobactam and probably adding in aminoglycoside. 07:05 If they are that sick to come into the hospital and receive piperacillin, tazobactam, I would add aminoglycoside, if I could. 07:13 And then again, think about a longer treatment duration, particularly if they’re really sick. 07:17 You’re going to treat for up to four weeks. 07:22 So, that covers nephrolithiasis and prostatitis, two important conditions that usually respond to therapy. 07:31 But you also can use your help of your urologic colleagues for those cases that break through. 07:37 Thanks.
About the Lecture
The lecture Urgent Urologic Disease by Charles Vega, MD is from the course Acute Care. It contains the following chapters:
- Urgent Urologic Disease
- Prostatitis
Included Quiz Questions
What is the most common type of kidney stone found in the general population?
- Calcium oxalate
- Calcium phosphate
- Uric acid
- Struvite
- Cysteine
Which of the following types of stones is most commonly seen in patients with gout?
- Uric acid
- Calcium phosphate
- Calcium oxalate
- Struvite
- Cysteine
Which of the following is the most common cause of struvite kidney stones?
- Urinary tract infections
- Gout
- Obesity
- Dietary calcium
- Thiazide diuretics
Which of the following medications is NOT associated with an increased risk of kidney stone formation?
- Thiazide diuretics
- Phenytoin
- Ceftriaxone
- Sulfonamides
- Ciprofloxacin
Which of the following medications is most appropriate in the prevention of recurrent calcium oxalate stones in patients with elevated urinary calcium?
- Thiazide diuretics
- Allopurinol
- Steroids
- Amoxicillin
- Laxatives
What is the most common pathogen associated with prostatitis?
- Escherichia coli
- Pseudomonas aeruginosa
- Neisseria gonorrheae
- Klebsiella
- Enterococcus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |