Playlist
Show Playlist
Hide Playlist
Undescended Testicle in Children and Painful Testicle Syndrome
-
Slides UndescendedTests Pediatrics.pdf
-
Download Lecture Overview
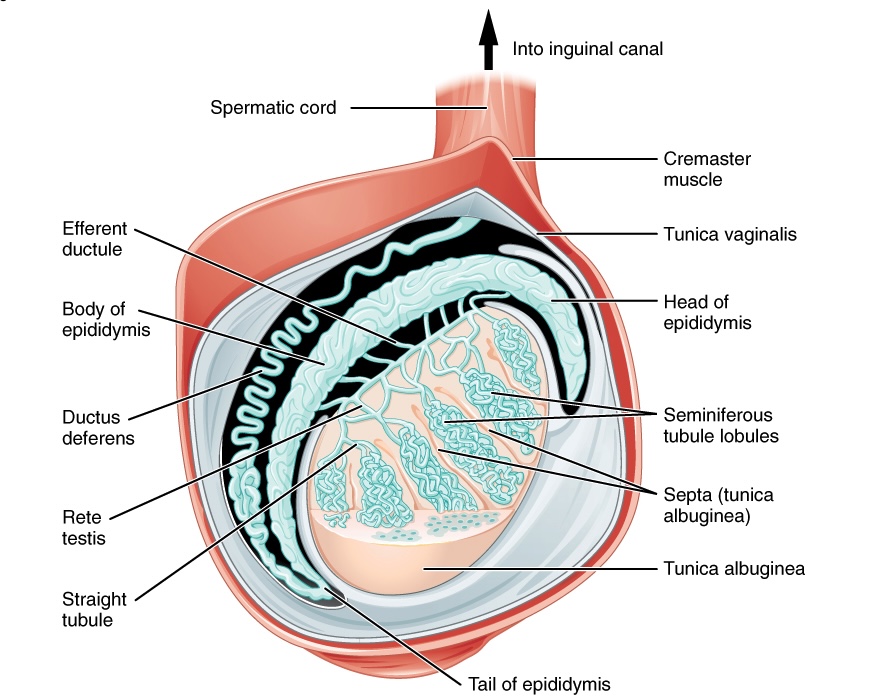
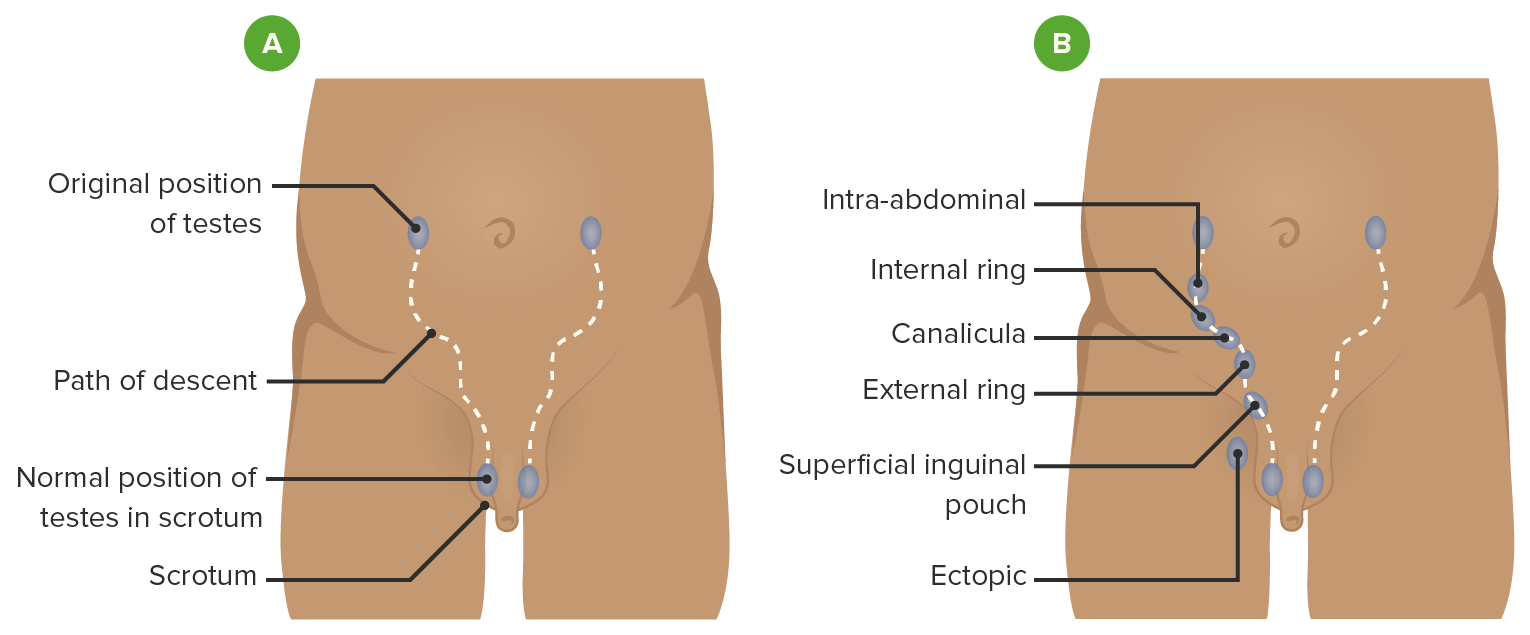
00:01 In this lecture, we’re going to review, very briefly, testicular problems in children. 00:07 So let’s start with undescended testes. 00:10 This is probably the most common problem we’ll encounter. 00:12 It’s also called cryptorchidism. 00:15 This is when a testis is not palpable in a baby’s scrotum. 00:19 It’s fairly common. 00:21 Ten percent of the time, the impalpability of the testes is bilateral. 00:26 In other words, both testes have failed to descend. 00:30 It’s important when you see this in a child to distinguish an undescended testis from a testicle that is still just high up in the canal because those usually will descend on their own. 00:40 So really feel all the way up to the beginning of the canal to try and feel that testis. 00:46 Also occasionally retractile testes, for example if the child was cold, are high up and could be missed. 00:52 Those can be generally milked down into the sac. 00:56 This is very common, like I said, and happens between 2 and 5% to the time in full term babies. 01:03 It’s even more common in premature infants with fairly one-third of infants who are premature suffering from an undescended testicle. 01:12 If the patient has bilateral undescended testes or hypospadias, consider a disorder of sexual development. 01:19 There are many such disorders. 01:21 Generally, we’ll get an ultrasound, both to look for gonads and to exclude uterus in a phenotypical male. 01:28 So these are all many different genes that can cause this. 01:31 One example would be an SRY mutation variant. 01:36 So in patients where we have undescended testes, we may obtain labs as well especially if there is unclear sexual development. 01:45 We often get electrolytes and a 17-hydroxyprogesterone if we’re concerned about congenital adrenal hyperplasia. 01:53 You can hear about more of that in one of our endocrine lectures. 01:57 In patients where there is inefficient masculinization, we may get LH and FSH to see if there is central lack of development or we may also check for a Mullerian-inhibiting substance. 02:10 We may also get karyotyping if we’re unclear as to which gender this baby is. 02:18 However, most of undescended testes are unilateral and most descend on their own within the first 6 months of age in phenotypically and genetically normal males. 02:30 If this testis has not descended, we may need to move on to an orchiopexy. 02:38 In an orchiopexy, the viable testicle is manipulated into the scrotum and sutured in place. 02:46 The non-viable testicle, which can happen sometimes, would be removed and often times later, a prosthesis may be placed for cosmetic appearance. 02:57 HCG can be injected intramuscularly and that may help with the descent of testicles into the scrotum in a small percentage of patients. 03:06 This is not commonly done, but it is sometimes done. 03:11 So why do we do orchiopexy? Well one of it is simply because spermatogenesis is more efficient in the outside of the body. 03:20 But also, an undescended testis is at risk for neoplasm. 03:25 This tends to happen after puberty. 03:27 In patients where there is a delay or they simply don’t get around to doing an orchiopexy, these infants are at increased risk once they had puberty of developing testicular cancer. 03:41 Additionally, we like to bring them down after one year and not with too much more delay because this may affect decreased fertility. 03:52 If the patient is not repaired, they may also be at increased risk for testicular torsion and a hernia. 04:01 Again, non-viable testes are typically just removed. 04:06 So let’s move now to three common causes of a painful testicle in a child who has essentially normal testicles. 04:15 So this person has come in and they are now having testicular pain. 04:19 What could cause it? One emergency is testicular torsion. 04:25 Testicular torsion is a surgical emergency. 04:28 It’s caused by a twisting of the testicle on itself inside the scrotum. 04:34 This results in interruption of blood supply, results in acute necrosis and potentially loss of the testicle. 04:41 It is exquisitely painful. 04:44 The hydatid torsion, also known as a torsed appendix testis is painful but is benign. 04:52 This is treated with NSAIDs. 04:54 This is a torsion of just the appendix of the testis and may appear quite appropriately as a little blue dot on the scrotal wall. 05:04 Last is epididymitis. 05:07 Epididymitis may cause pain in the testis, but this is an infection. 05:12 In younger children, it can be caused by viruses or bacteriuria type organisms such as E. coli. 05:20 In adolescents, this is more likely to be caused by sexually transmitted diseases like gonorrhea and chlamydia. 05:28 So if we look at the age when these three things typically happen, epididymitis is actually more common very early in childhood and that’s from E. coli like organisms and then later on you may get as a result of being infected with a sexually transmitted disease. 05:46 Hydatid torsion or a torsed appendix testis tends to happen around 10 years of age or so and testicular torsion is usually seen in adolescent males. 05:58 So let’s look at testicular torsion carefully. 06:02 So there is a twisted epididymitis and the testis becomes black and this is testicular torsion. 06:09 Here, you can see a patient with testicular torsion. 06:12 A few things are key. 06:13 One, they will be in exquisite pain. 06:16 Two, it will start off as red and this one is perhaps starting to turn blue and if left alone, will turn black which means it is now dead and necrosed. 06:26 The patient’s testicle will have a high lie. 06:29 You can see this here. 06:30 The testis is elevated and it’s often in a lateral position. 06:34 It’s swung laterally. 06:36 Also, if you were to take the time to do this, there would be an absent cremasteric reflex. 06:41 Remember, a cremasteric reflex is noted when you stroke the inner side of the thigh preferably with a cold object and testicle will rise up. 06:51 Because the cremaster muscle in this patient has become entrapped, there is no cremasteric reflex. 06:58 For patients with testicular torsion, this is an emergency. 07:02 The first thing we should do is provide morphine and then very quickly call the urologist. 07:08 Often times, you can prevent a surgery, however, if you first try to manually reduce it. 07:15 The way this is reduced is by turning the testis outward. 07:19 We say “open the book”. 07:21 So you approach the testis and you turn it as if you were opening the cover of a book and this should relieve the torsion and allow blood to flow again. 07:31 Please provide morphine when you’re doing this procedure. 07:34 Alternatively, if that’s not going to do the trick or you’re unable to reduce the torsion, you need to call the surgeons. 07:42 They will come racing in from home to fix the problem. 07:45 So that’s my summary of these three things that cause testicular pain. 07:49 Thanks for your time.
About the Lecture
The lecture Undescended Testicle in Children and Painful Testicle Syndrome by Brian Alverson, MD is from the course Pediatric Nephrology and Urology. It contains the following chapters:
- Undescended Testes
- The Painful Testicle
Included Quiz Questions
Which of the following testicular complaints is a surgical emergency?
- Testicular torsion
- Epididymitis
- Undescended testicle
- Hydatid torsion
- Varicocele
What percentage of children with cryptorchidism have bilateral undescended testes?
- 10%
- 20%
- 30%
- 40%
- 50%
Which of the following is the most appropriate screening test for congenital adrenal hyperplasia?
- Serum 17-OH-progesterone
- Serum cortisol levels
- Serum dehydroepiandrosterone
- Serum aldosterone
- 24-hour urine metanephrines
The risk of which of the following is NOT increased in a patient with an undescended testis?
- Varicocele
- Testicular cancer
- Infertility
- Testicular trauma
- Testicular torsion
A child 10-year-old presented with pain on the scrotum. On examination, testes are tender to touch and a blue dot is seen on the scrotum. What is the probable diagnosis?
- Hydatid torsion
- Testicular torsion
- Epididymitis
- Varicocele
- Inguinal hernia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. The differential diagnosis is much better than what I've been taught so far. Thanks!