Playlist
Show Playlist
Hide Playlist
Secondary, Tertiary and Congenital Syphilis
-
Slides STD Female Repro.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
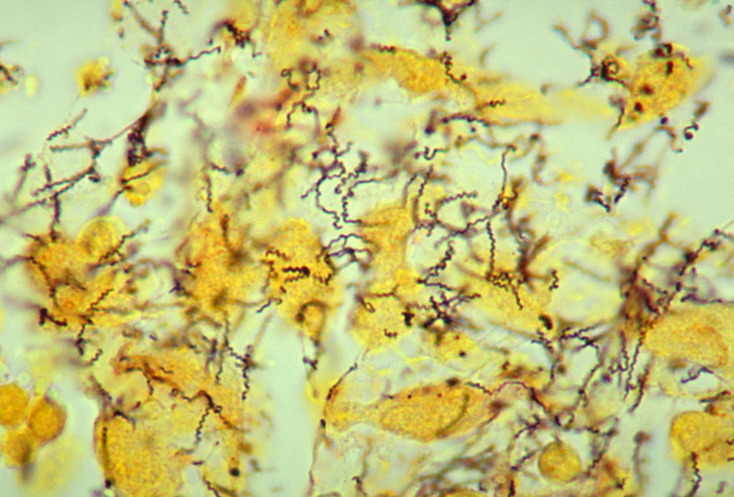
00:01 The secondary syphilis. 00:03 A couple of things that you very much want to keep in mind with secondary syphilissyphilis that you will not find with primary. 00:09 First, it’s five weeks after primary lesion. 00:14 Go in odd numbers. We have three and five. 00:18 Three weeks after the lesion will be primary. 00:20 Five weeks after the primary would be secondary. 00:23 What are you going to find in secondary? Proliferation of spirochete and the skin and the mucous membrane become involved. 00:30 Skin is huge. 00:32 And the reason I say skin is in the picture. 00:34 You’ll find these lesions on the palms and the soles. 00:40 Secondary syphilis. 00:41 You will not find this is in primary. 00:44 Most likely. 00:46 Moist areas are also where you would find these lesions. 00:50 You’re thinking about the axilla or anogenital region, and then the mucous membranes include your mouth, the throat, the vagina. 00:57 All part of your syphilitic secondary type. 01:01 Primary and secondary, keep them separate. 01:05 The tertiary would be five years or more after initial infection. 01:11 So now, the number that you want to know for sure or your area code is 3-5-5. 01:16 Three weeks for primary. 01:19 Five weeks after the primary for secondary. 01:23 Five years after, you then develop tertiary. 01:28 This is the one that you have probably seen many times in -- Well, we’ve talked about this in cardiology and you’ve also talked about this in neuroscience, with something called tabes dorsalis. 01:39 When did we talk about this in cardiology? I gave you that murmur in which you’d find the murmur by the third intercostal space, left parasternal. 01:47 What is that? Remember, please, if the small blood vessels are being involved by proliferative endarteritis and they’re obliterated, we call this what in tertiary syphilis? Endarteritis obliterans. 01:59 If you knock out the endarteries vasa vasorum of the aorta, the aorta dilates and we call this syphilitic aortitis. 02:08 This typically occurs in the ascending thoracic aorta which causes aortic valve regurgitation and a murmur. 02:16 The coronary arteries may also become involved. 02:20 What kind of murmur did I give you? I gave you an early diastolic murmur, heard best third intercostal space, left parasternal. 02:27 When you have aortitis, what kind of murmur would that be? It has to be aortic regurg. 02:32 Aortic regurg and early diastolic murmur. 02:35 In addition, neurosyphilis, what does that refer to? It refers to your tabes dorsalis. 02:41 What does tabes dorsalis mean to you? What’s the dorsum aspect of the spinal cord? What kind of column or path is that then transmitting up into the head? That’s correct. 02:51 You have your dorsal column. 02:52 And so therefore, you’re not going to have propioception. 02:55 You close your eyes, you try to stand still, but oh, you’re wobbling. 03:00 Positive Romberg. 03:02 Or you can’t -- proper touch and proper vibration, right? That’s all part of tabes dorsalis. 03:10 Remember neuroscience. 03:12 Benign tertiary syphilis. 03:14 Inflammation of what’s known as a gumma. 03:15 You might want to think of this as being a granuloma-like, okay? Inflammation of a gumma in skin and bone and mucous membrane to perhaps try to imprison your organism. 03:27 Primary, secondary, tertiary syphilis are key points that you make sure that you know before taking your boards. 03:37 Congenital syphilis. 03:38 What does this mean to you? Remember, please, that this is part of your TORCH. 03:42 Vertical transmission, occurs when an organism crosses the placenta to infect the fetus. 03:48 With congenital manifestations, you divide this into the early portion or the infantile and you turn this into what’s known as your late. 03:55 Early on, you’d expect to find skin rash, skeletal abnormalities. 04:00 You might have heard of something called your saber shin. 04:07 If you haven’t heard of it, that’s fine, because they won’t put saber shin. 04:12 What they will say or what they will describe is the anterior curvature of your tibia, okay? Think about the tibia. 04:20 It should be nice and straight obviously, but if you’d find an anterior curvature of it, you call that a saber shin. 04:26 Look for that please. 04:29 Late, tardive. 04:31 We have Hutchinson's triad. 04:33 Notched incisors, we have insterstitial keratitis with blindness, deafness from 8th cranial nerve injury. 04:42 Remember once again this is called Hutchinson's triad. 04:45 You might have even heard of Hutchinson's teeth. 04:48 Notched. What does that mean to you? Well these look like pegs of the central incisors. 04:53 Pegs of what? A fence. 04:55 If you try to build a fence, the bottom of wood looks like it’s notched so that you can dig it into the ground or literally inject it into the ground. 05:05 These are called notched incisors. 05:07 Definitely pay attention to that. 05:09 Then, we have what’s known as interstitial keratitis. 05:11 Where are you? The conjunctiva And deafness from the 8th cranial nerve injury. 05:17 This is all part of your tardive type of congenital syphilis. 05:22 You definitely want to know this and once again be able to organize it into early and late, tardive.
About the Lecture
The lecture Secondary, Tertiary and Congenital Syphilis by Carlo Raj, MD is from the course Sexually Transmitted Diseases (STDs).
Included Quiz Questions
Which of the following is the MOST likely clinical picture in a patient who has been diagnosed with secondary syphilis?
- A generalized mucocutaneous rash involving the palms and soles
- Seizures, delirium, and high-grade fever with small, red, clustered papules on the chest, arms, and legs
- Generalized tender blisters sparing the palms and soles and mucocutaneous junctions
- Ulcerated chancres both inside and outside of the vagina, with severe pruritus
- Generalized, tender, oozing and bleeding small ulcers, accompanied by a low-grade fever and a new murmur on auscultation
What length of time after exposure do primary, secondary, and tertiary syphilis present?
- Primary syphilis–3 weeks after initial exposure, secondary syphilis–5 weeks after primary lesion, tertiary syphilis–5 years after initial exposure
- Primary syphilis–one day after exposure, secondary syphilis–3 weeks after exposure, tertiary syphilis–2 years after exposure
- Primary syphilis 3 days after exposure, secondary syphilis 5 days after exposure, and tertiary syphilis 5 months after exposure
- Primary syphilis–3 hours after exposure, secondary syphilis–5 hours after primary lesions, tertiary syphilis–5 weeks after secondary syphilis
- Primary syphilis–3 days after exposure, secondary syphilis–5 months after primary syphilis, tertiary syphilis–5 months after secondary syphilis
How is Treponema pallidum transmitted from an untreated pregnant woman (with no active lesions) to her child?
- Transplacental transfer
- During passage through the birth canal
- At the time of placental detachment
- Through breastfeeding
- Through skin-to-skin contact
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |