Playlist
Show Playlist
Hide Playlist
Tuberculosis: Epidemiology, Cause and Pathogenesis
-
Slides 02 InfluenzaATuberculosis RespiratoryAdvanced.pdf
-
Download Lecture Overview
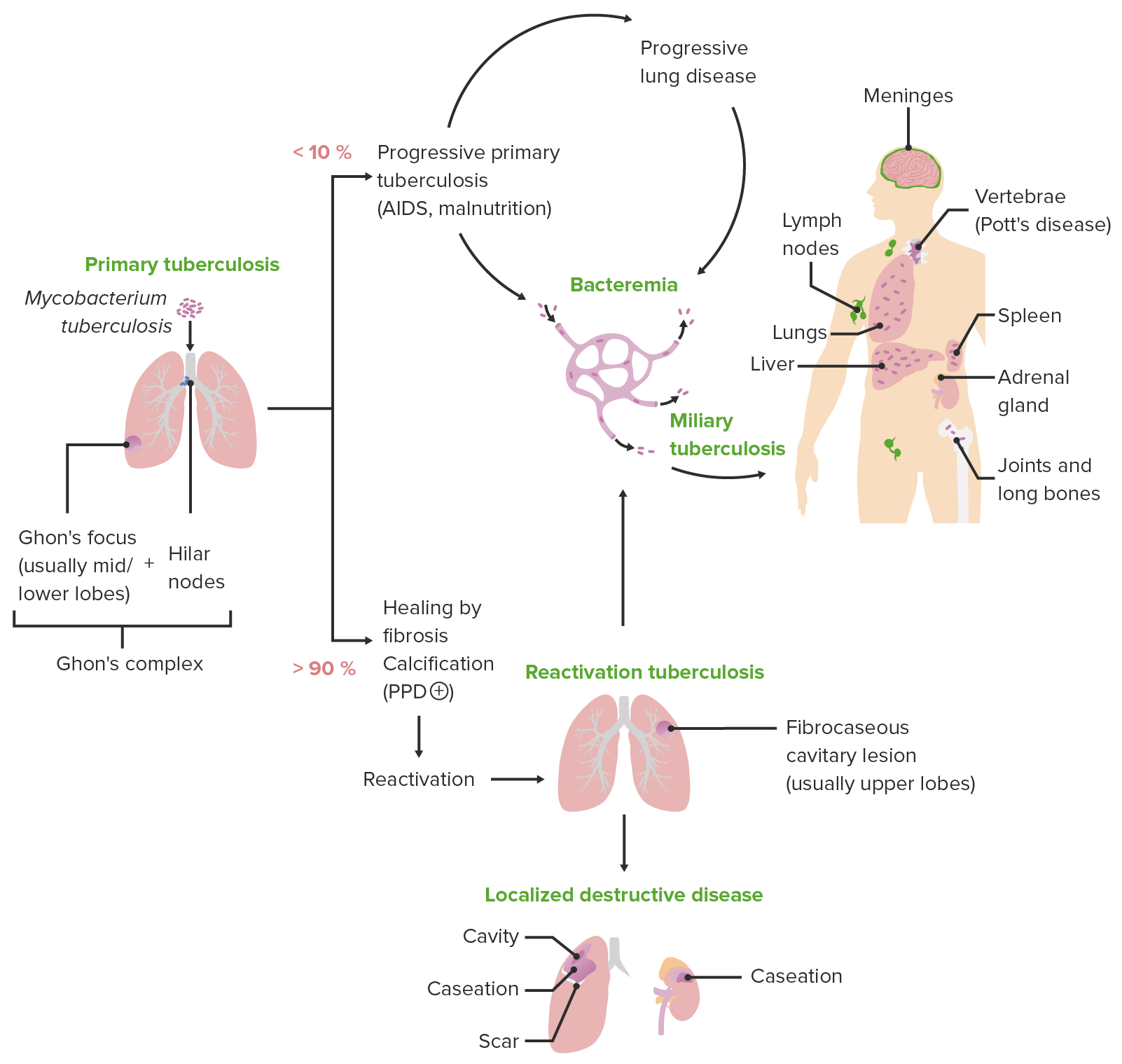
00:01 what’s the epidemiology of tuberculosis? Well, 30% of the population of the world are infected by tuberculosis. Fortunately, most of those patients have what we call as latent infection, that is the bacteria is present in the body but it’s not causing active disease. Of those 30% of the population of the world, it's estimated about 10% will actually have reactivated disease from that latent disease over a lifetime and what that means that the dormant bacteria stopped replicating and actually start to cause an infection. 00:41 At any one time there are about 10 million people across the world with active tuberculosis infection and that causes death in about 10% of them. So we are talking one million deaths per year and that makes tuberculosis the first or second commonest cause of bacterial infectious death across the globe. What’s tuberculosis caused by? It’s caused by the organism Mycobacterium tuberculosis. Now this is quite an unusual bacteria. 01:07 So unlike the bacteria that cause Pneumococcal pneumonia, it is quite slow growing, it takes several weeks to culture it in the laboratory. It has a very unusual cell wall full of lipid, and there is no environmental source, you cannot catch tuberculosis from the environment you catch it from somebody else who is already infected with the bacteria. There are a couple of sub-species of Mycobacterium tuberculosis- Mycobacterium bovis, Mycobacterium africanus, and there is also the BCG. Now that is the Mycobacterium bovis that has been cultured in the laboratory and is now not pathogenic, it doesn’t cause disease, or rarely causes disease and we use that as a vaccine to try and prevent tuberculosis infection. As I’ve already mentioned there are environmental mycobacteria which are related to M. tuberculosis and these are called the non-tuberculosis mycobacteria and there is quite a lot range of different species and they can cause a similar disease to tuberculosis, sometimes, but they are far outweighed by patients infected with M. tuberculosis. So the pathogenesis of tuberculosis, like Influenza A requires being infected by somebody with active disease. 02:19 So If somebody has active lung disease with tuberculosis they will cough and in the cough, there will be infected droplets carrying the bacteria that can be inhaled by somebody else. 02:30 Once the bacteria is inhaled, it gets into the lung, and there it actually invades your normal mechanism for protecting the lungs against bacterial infection which are the alveolar macrophages. It actively seeks out and invades these macrophages because it's able to prevent the normal macrophage killing mechanisms. So it diverts the normal phagolysosome pathways and that allows it to survive in the macrophage and it can be latent in that macrophage for decades. In addition, the macrophages because they move, will allow the bacterium to spread across the body, and this is one of the reasons why sites of immune function such as the lymph nodes often get infected with tuberculosis. Long term persistence within the macrophages is what latent disease is. In addition, there is a certain inflammatory response to this infection, which causes a very distinctive histological appearance called granulomas and that is one of the hallmarks of tuberculosis infection, is the presence of granulomas in the infected tissue. So to talk about the disease, there's two main forms- there's pulmonary tuberculosis, which is TB affecting the lungs, and there is extra-pulmonary tuberculosis which is TB affecting outside the lungs.
About the Lecture
The lecture Tuberculosis: Epidemiology, Cause and Pathogenesis by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Infections of the Respiratory Tract. It contains the following chapters:
- Epidemiology
- Cause of TB
- Pathogenesis of TB
Included Quiz Questions
Which of the following statements is most accurate regarding the epidemiology of tuberculosis?
- 25%–30% of the world population are estimated to be infected.
- Approximately 10 million people worldwide are estimated to be infected.
- Despite the high prevalence, tuberculosis comprises a minority of worldwide deaths due to bacterial infections.
- Approximately 1 million people worldwide have active tuberculosis infection.
- Annually, approximately 10 million deaths are due to tuberculosis worldwide.
Which of the following is a subspecies of Mycobacterium tuberculosis? Select all that apply
- Mycobacterium bovis
- Mycobacterium avium
- Mycobacterium leprae
- Mycobacterium africanus
Which of the following is a distinguishing feature in the cell wall of Mycobacterium tuberculosis compared to that of most other bacteria?
- Mycolic acid
- Peptidoglycan
- Cellulose
- Chitin
What is the main mode of transmission of pulmonary tuberculosis?
- Inhaled droplets
- Genital secretions
- Bloodborne
- Direct skin contact
- Vector borne
Which of the following statements about the pathogenesis of Mycobacterium tuberculosis is FALSE?
- Mycobacterium tuberculosis is an extracellular pathogen.
- Mycobacterium tuberculosis is phagocytosed by alveolar macrophages.
- The cell wall prevents fusion of the phagosome with the lysosome.
- Mycobacterium tuberculosis can maintain a latent state for a prolonged period.
- Caseating granulomas are seen.
When Mycobacterium tuberculosis enters the body, which cells initially respond?
- Macrophages
- Neutrophils
- Eosinophils
- Lymphocytes
- Monocytes
Which of the following is the primary mechanism by which Mycobacterium tuberculosis survives inside alveolar macrophages?
- Diverting the phagolysosome pathway
- Secreting cytokines that destroy the macrophage lysosomes
- Preventing opsonization
- Enhancing the maturation of the phagosome
- Producing reactive nitrogen species
Which of the following is the immunological hallmark of Mycobacterium tuberculosis infection?
- Granuloma formation
- Fibrosis of the lung
- Cavitation
- Angioinvasion
- Consolidation
Which of the following statements about Mycobacterium tuberculosis is TRUE?
- The histological hallmark of Mycobacterium tuberculosis infection is caseating granulomas.
- Mycobacterium tuberculosis is a rapidly growing bacterium.
- Most patients infected with Mycobacterium tuberculosis have active disease.
- Mycobacterium tuberculosis can be acquired through contaminated water.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
These reviews are very helpful. I appreciate the pictures and description of the bacteria