Playlist
Show Playlist
Hide Playlist
Treatment of GERD
-
Slides GD Esophagus.pdf
-
Download Lecture Overview
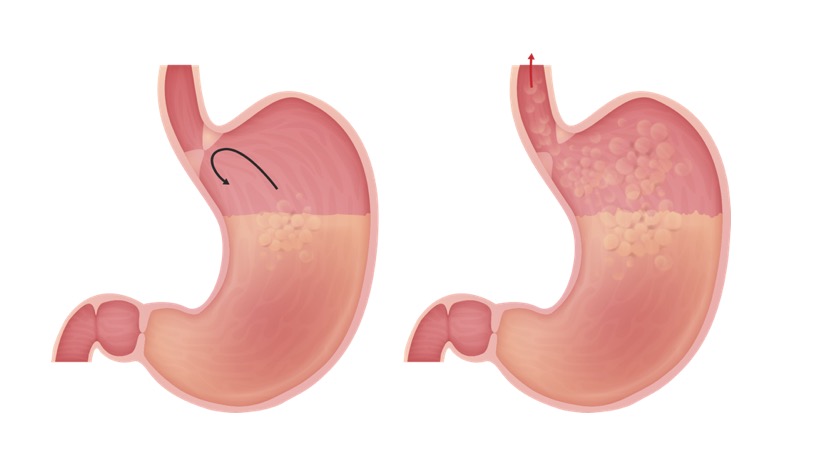
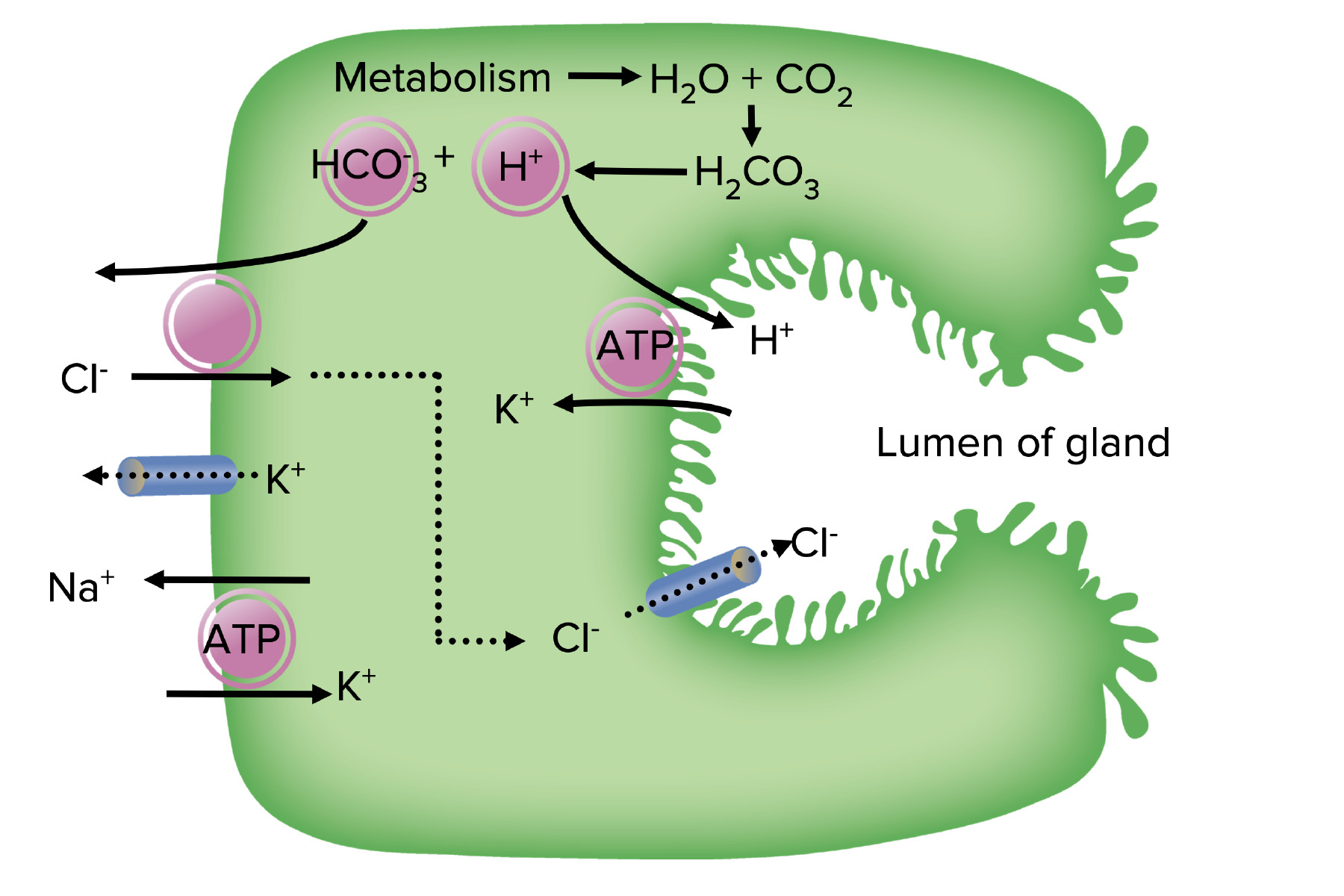
00:00 Treatment. So what is your next step of management with GERD, GERD, GERD? Do not change or do not administer medication. That is not your first step. Conservatively you check to see, in the stem of a question, in your vignette and with your patient, as to whether or not they have already started to implement lifestyle modifications. You want to try to avoid those agents that would further relax your lower esophagal sphincter. In a condition where that is indeed the pathology. For example, avoiding tobacco and alcohol. When going to bed at night, you'd recommend to keep the head elevated by approximately 6 to 8 inches so that you prevent reflux from taking place. Same concept in terms of meals. 00:56 When the stomach is full, you do not want to lie down immediately for the fact that you may then facilitate reflux. Avoiding meds that lower, lower esophageal sphincter pressure. 01:08 After lifestyle modifications, if we start getting into realm of, well more moderate type of symptoms of GERD, then you start thinking about using H2 blockers. 01:22 H2 blockers include drugs such as ranitidine, famotidine. And then PPIs would be if the symptoms of the patient were much more severe. Proton pump inhibitors. Need at least 6 weeks of therapy to find any type of decrease in the symptoms of the patient. Let's say that we have refractory cases and you have gone through the hierarchy of management of GERD; Including the fact that, once again, remember we start with lifestyle modifications. Next, start using H2 blockers if the severity is increasing. And if it's much more severe, it's frequent, and you are even worried about erosion and such, then you start thinking about using PPI. And don't forget that it may, especially in the antral region of the stomach you might have H. pylori that's involved and therefore giving rise to something called gastritis. 02:22 Chronic type b. Chronic type b type of gastritis. Therefore at that point H. pylori eradication would be recommended. Surgically, what you want to do is, if the lower esophageal sphincter is not responding, you'll take the fundus of the stomach; But before the surgery you'll notice that everthing is weak here. And then you'll take the fundus of the stomach and then you will wrap this around the lower esophageal sphincter. In other words, you're making this much more tight. And you're making it much more difficult for reflux from taking place. Not only would you then take the fundus of the stomach and wrap it around it to tighten, or in other words create a sphincter surgically. But then you would go back and re-estimate the actual lower esophageal sphincter to make sure that everything is in proper order to prevent reflux from taking place. 03:17 So there are many, many, many, many ways in which we could properly regulate and control our reflux but it begins with reflux control with lifestyle modification.
About the Lecture
The lecture Treatment of GERD by Carlo Raj, MD is from the course Esophageal Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
A patient with a prolonged history of GERD (> 2 episodes per week) comes to your clinic seeking treatment. Which of the following would be the MOST appropriate initial step in the management of this condition?
- Proton pump inhibitor trial
- Nissen fundoplication
- Lifestyle modifications only
- Famotidine trial
- Antibiotics
A 40-year-old man comes to your office asking for "better medications" for his GERD because lifestyle modification has been ineffective. What would be the MOST appropriate next step in management?
- Omeprazole
- Calcium carbonate daily
- Omeprazole and cimetidine for 6 weeks
- Drugs to fix gastroparesis
- ECG
Which of the following is NOT used in the evaluation and treatment of GERD?
- Chest X-ray
- Cessation of smoking and alcohol
- Proper diet and sleep routine
- Endoscopic evaluation
- Omeprazole and cimetidine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |