Playlist
Show Playlist
Hide Playlist
Treatment: Curable and Incurable NSCLC
-
Slides 07 LungCancer Tumors and Metastases Neoplasias RespiratoryAdvanced.pdf
-
Download Lecture Overview
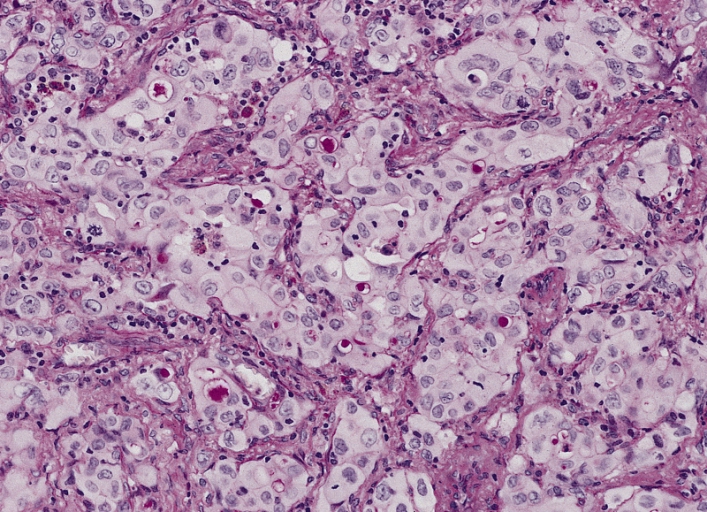
00:00 So localized disease is not invading mediastinal structures of the chest wall excessively can be cured by resection. But that is only about 15% of the patients and if a patient, one of these lucky 1 in 6, 1 in 7 patients has a resection, their 5 year survival is about 70%. So not bad. However they have a 85% have inoperable disease and their 5 years survival is very poor indeed. But having a localized tumour is not the only thing a patient requires before they can have curative surgery. 00:40 They need to be out of cope with a surgery and that depends on their function and status. 00:45 So for example if you got a patient who is out walking around looking after themselves has a good functional status then surgery would be a reasonable option. 00:54 However if you got somebody presenting with resectable cancer who is unable to walk due to very severe COPD etc. Then they are not really going to be candidate for surgery. 01:05 Not only as a low functional status, but we needed to think about what their lung function is like. So the example about the patient who was out walking about maybe they are walking a 100 yards before they get breathless because of COPD. However if you do a lung resection that ability to walk a 100 yards is going to fall because you have lost lung volume. So you need to consider whether the lung resection itself may make the patient unable to breathe adequately for normal life and then there is general comorbidities. Somebody who has got extensive cardiac disease, renal disease, and existing tumour elsewhere in the body then surgery is a much less attractive option. There are essentially two types of tumour resection. One is a lobectomy and that's if the cancer is confined to one lobe and the other is the pneumonectomy. So if a tumour has crossed the oblique fissure and therefore affecting the upper and the lower lobe then the patient will have to have the total whole lung removed. 02:07 The survival from lobectomy, the risk from the lobectomy operation is less than from a pneumonectomy. Actually the lung function lost from lobectomy is a lot less than a lung function lost from pneumonectomy. And these considerations need to be taking for count when identifying patients for surgery.There is a another option which is what we called a wedge resection where just the cancer and the tissue near to the cancer is removed but is known that the chance of recurrence after wedge resection is higher. So wedge resection are kept in reserve for patients who really cannot tolerate more than that small amount of lung being removed. 02:48 If you have tumour which is extensive, the higher stages but still resectable ones of hilar lymph nodes for example then the patient is quite likely to get chemotherapy or radiotherapy after the operation as that seems to reduce the chance of recurrence. 03:03 If a patient has a localized tumour that can be enclosed in one radiotherapy field but cannot survive, he's not fit enough to have surgery and radical radio therapy is another alternative method of potentially curing that cancer. But the cure rate from radical radiotherapy is a lot lower than it is from resection. So it's the second best option. 03:34 Now, unfortunately they said 80-85% of patients presenting with lung cancer do not have curable disease. The stage has gone to mediastinal invasion, chest wall invasion, distal metastases and therefore you cannot cure the tumour by resection. There 5 years of survival is less than 5%. We know that chemotherapy is helpful and that it delays the deterioration in the patient’s condition on average by about 6 months extends a life expectancy of about 6 months. But it is not aimed to curing. It is a palliative treatment. If the patient has specific symptoms, some of these are very susceptible, very easily treatable with radiotherapy. First so for example, pain due to invasion of the chest wall, pain due to metastases in the bone, obstruction of the bronchus due to a large tumour, haemoptysis, and brain metastases are all situations where you'll consider giving the patient what we call palliative radio therapy. This is not aimed to cure the patients but it is aimed to alleviate the problems of that specific issue it's causing. Stopping haemoptysis, reducing the pain, opening at the bronchus so the patient so the patient's breathing improves slowing down the growth for brain metastases. In patient with brain metastases, alot of the problems that they have are due to the edema around the growing tumour. So if you give the patients steroids that reduces that edema. It is actually quite striking, the improvement in somebody’s neurological conditions that could be given just by giving them high dose corticosteroids. Quite often somebody would come into the hospital with dense left hemiplegia, unable to move the left hand side of the body because of the large brain metastases in the right side. But if you give them corticosteroids what will happen is that the edema will shrink down and the movement will come back. So that is the useful therapy at least acutely. 05:36 Recently there have been developments in the chemotherapy which are very exciting and potentially very important for the future. So for example, there are specific mutations that affect patients with adenocarcinoma of the lung which affects surface receptor called the EGFR and there are now inhibitors of the EGFR function which are used in these patients with that type of mutation, have got a marked effects on tumour growth quite often causing a large decrease in the tumour growth at least temporarily.
About the Lecture
The lecture Treatment: Curable and Incurable NSCLC by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Lung Cancer.
Included Quiz Questions
In non–small cell lung carcinoma (NSCLC), which of the following is NOT a factor in the decision towards patient fit for curative surgery?
- Age of the patient
- Residual lung function
- Functional status of the patient
- Presence of comorbidities
- Blood tests without abnormalities
Which of the following are conditions for which palliative radiotherapy is effective?
- All the options are conditions for which palliative radiotherapy is effective.
- Treatment of pain due to local invasion of the tumor
- Treatment of pain due to bone metastasis
- Treatment of bronchial obstruction due to the tumor
- Treatment of hemoptysis
What is the purpose of giving high-dose corticosteroids with lung cancer metastases to the brain?
- Decreases edema and pressure on the brain
- Augments the effect of chemotherapy on the tumor
- Augments the effect of radiotherapy on the tumor
- Reduces the tumor burden before surgery
- Decreases the potential for future infections
Which targeted therapy agent is useful for the treatment of lung cancer?
- EGFR inhibitors
- RET inhibitors
- ER/PR receptor agonists
- p53 gene modifiers
- Her2/neu inhibitors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This lecture provides a good, general overview of deciding if a patient is a candidate for surgery. Though brief, it is much better explained than in review books.
He answers the question right away , and explains everything amazingly