Playlist
Show Playlist
Hide Playlist
Abdominal Injuries
-
Slides AbdominalInjuries Surgery.pdf
-
Download Lecture Overview
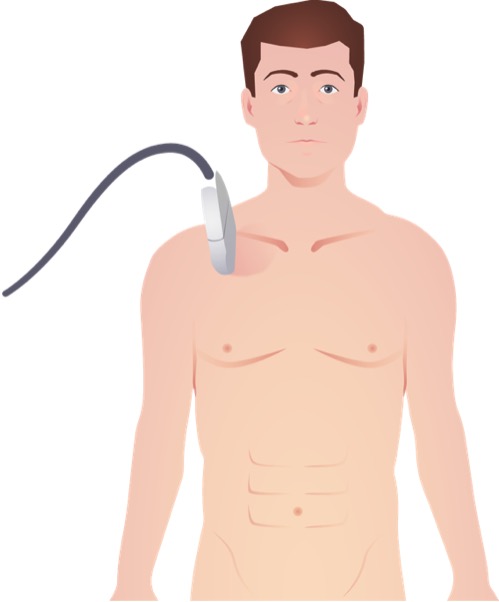
00:01 Let's begin with the discussion of abdominal injuries. 00:04 Now typically, we think of abdominal injuries as penetrating or blunt. 00:10 I'll give you a global overview of important injury patterns. 00:14 First, an examination of the patient as you disrobe the trauma in the trauma bay, what are you looking for? Sometimes a patient may have abdominal bruising. 00:24 Other times, patients may have abdominal tenderness. 00:28 Overall, however, these studies are neither very sensitive nor specific. 00:32 Hiding next to suspension is again important. 00:36 Remember, any patient suspected of hemorrhage and hypotensive like our patient, there are some general concepts to keep in mind. 00:46 Number one, replace the blood. 00:49 More and more now we're trying to reduce the amount of crystalloid fluid resuscitation and as you're giving blood, whether it's a few units or a massive transfusion, you wanna keep it as close to whole blood as possible. 01:02 In other words, a 1:1:1 ratio of blood, plasma, and platelets. 01:09 This probably has the best outcome in terms of coagulopathy. 01:12 Next, it's important to locate the source of the bleeding. 01:16 You notice that we replenish blood before knowing exactly where the source is. 01:20 I'll discuss a little bit of your options for locating the source of bleeding. 01:26 Next, after you've localized the source of bleeding, obviously stop the bleeding as much as you can. 01:32 Remember, sometimes in trauma, it's not an actual anatomic bleed and becomes coagulopathic. 01:38 These patients are in dire straights. 01:41 For the initial assessment, remember, once you've ascertained A and B, we can't go any further past C because the patient is hypotensive, which falls under the C for circulation. 01:54 Very importantly and perhaps most importantly, never take an unstable patient to the radiology suite. 02:01 Go straight to the operating room or interventional suite, depending on the scenario. 02:06 On the exam, very frequently, patients are hypotensive and you may be tempted to choose a diagnostic study but don't intervene. 02:15 What diagnostic study is the most helpful in the evaluation of hemodynamically unstable trauma patient? I'll give you a second to think about it. 02:26 That's right. It's not a CAT scan or an X-ray. 02:29 It's the eFAST, extended FAST or focused abdominal stenography of trauma. 02:34 Let's discuss eFAST in a little bit of detail. 02:37 eFAST examination has really revolutionized how we detect intra-abdominal fluid. 02:45 When we detect intra-abdominal fluid in a trauma setting, it's presumed to be blood. 02:50 On our model here, you see the ultrasound probe in five directions. 02:55 This is the aortic extended portion. 02:57 Some years back, we didn't use to do the lung portion to let you evaluate for pneumothorax. 03:02 We only did a full quadrant view. Now, the standard across the country is an eFAST. 03:08 We'll discuss each view in a little bit more in detail but basically, we're looking for a right upper quadrant, left upper quadrant, super pubic, cardiac, and lung views. 03:19 This is our cardiac view. In the cardiac view, we highlighted an area of fluid in the pericardial space. 03:29 As we've discussed in thoracic lectures, any fluid in the pericardial space in a trauma patient is presumed to be traumatic, unless, the patient has a clear history of a chronic pericardial effusion. 03:41 If you find this on the eFAST portion, the appropriate therapy especially if the patient is hypotensive, is to do a pericardiocentesis. Now, let's take a look at this lung view. 03:54 You can see the R's are standing for the ribs and there's a white line which is actually the pleura. 04:02 Remember, there's a parietal pleura and a visceral pleura. 04:05 As we normally inspire and expire, these pleura linings actually slide past each other, which is visible on the ultrasound. 04:13 The lack of lung sliding or opposition of those two layers of the pleura suggests that there may be a pneumothorax. 04:22 Lung sliding on eFAST is extremely sensitive and specific. It's a great test. 04:28 So much so that oftentimes now while we're assessing whether or not a test tube has adequately drained in pneumothorax, we go straight to the ultrasound machine. 04:36 Remember, the ultrasound machine has added benefit of no radiation. 04:40 This, however, like all ultrasound procedures, is operator dependent. 04:45 Now, let's take a look at the right upper quadrant. 04:51 Here, you noticed that there's an interface between a liver and the kidney. 04:55 Again, on ultrasound, blood looks like a black stripe. 04:59 Any blood in this hepatorenal space, also known as Morison's pouch, suggested that there may be an injury to either the kidney or the liver. 05:08 However, remember, just because blood is present in a certain quadrant of the abdomen, doesn't necessarily mean that the actual injury is in that quadrant. 05:16 Moving on, we're in the left upper quadrant. 05:18 Here, we look at the interface between the spleen and the kidney. Very similar. 05:23 eFAST is incredibly useful and that the ultrasound is now so portable that it's frequently used in Austere environments. 05:31 Here, you see the military use of ultrasound on the combat field. 05:35 Now, I'd like to challenge you with the ultrasound. 05:42 Take a look at the next eFAST image of the abdomen and tell me what you see. 05:48 I'll give you a second to take a look. 05:51 Now, let's review. 05:57 On this image, you see blood around the liver and you actually see blood in the pleural space to the left of the image. 06:05 There's usually only one way this can happen, and that's if you have a patient with a diaphragmatic injury. 06:11 Again, just like we discussed in the thoracic lecture, diaphragmatic injuries usually give us indirect information. 06:18 Clearly, we don't actually see the diaphragmatic injury here.
About the Lecture
The lecture Abdominal Injuries by Kevin Pei, MD is from the course Surgery: Trauma. It contains the following chapters:
- Abdominal Injuries
- Ultrasound
Included Quiz Questions
Which of the following diagnostic modalities is the best for assessing the thorax in hemodynamically unstable trauma patients?
- Extended Focused Assessment with Sonography for Trauma (eFAST)
- Laparoscopy
- CT scan
- Endoscopy
- MRI
Which of the following is an appropriate therapy for a trauma patient who has fluid in the pericardial space on eFAST, hypotension, and no history of chronic pericardial effusion?
- Pericardiocentesis
- Thoracentesis
- Needle decompression
- Diuretics
- Pericardiotomy
On the eFAST lung view, lack of apposition of the two layers of pleura may be suggestive of which of the following conditions?
- Pneumothorax
- Atelectasis
- Pleural effusion
- Emphysema
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |