Playlist
Show Playlist
Hide Playlist
Thrombosis – Thrombosis and Anti-Thrombotic Therapy
-
Slides Thrombotic disorders.pdf
-
Download Lecture Overview
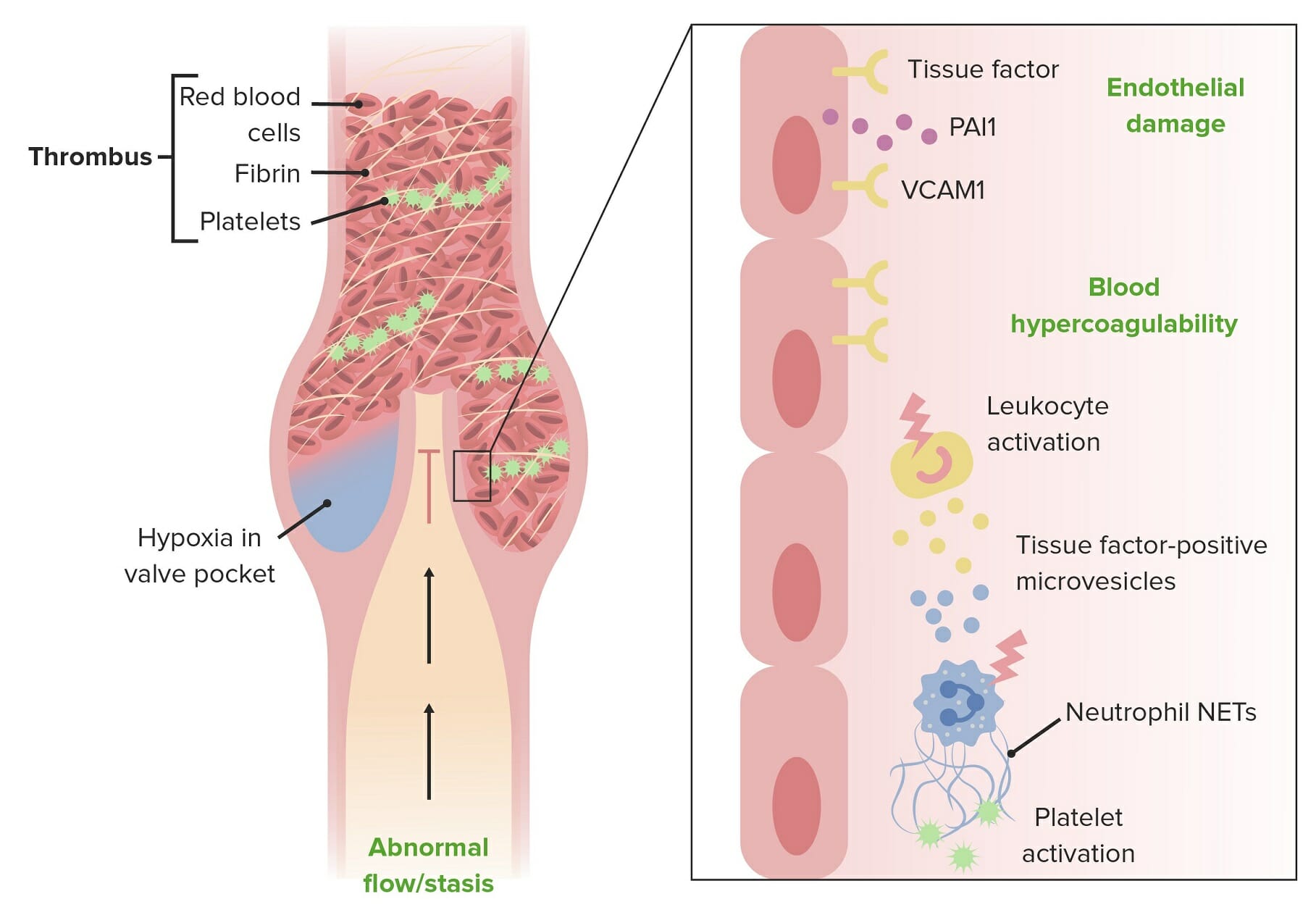
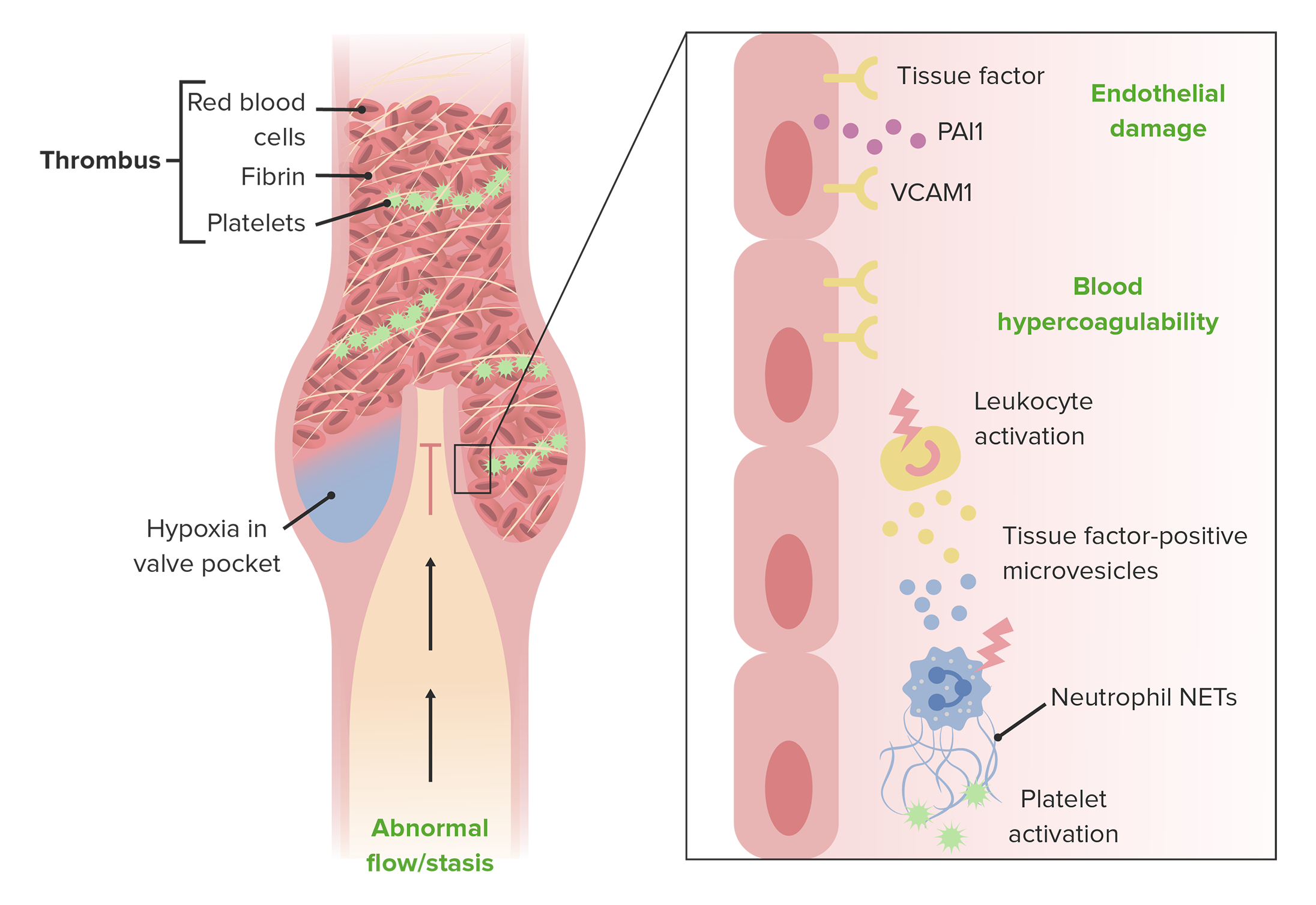
00:01 Hello, and welcome to this lecture on thrombosis and anti-thrombotic therapy. 00:07 We'll see in this lecture that thrombosis is one of the most important problems in medicine at the current time. 00:15 Some people carry an inherited predisposition to venous thrombosis, and environmental risk factors include bed rest or surgery. 00:25 Arterial thrombosis is primarily the result of atherosclerosis. 00:31 And heparin and warfarin have been mainstays of anti-thrombotic therapy, but a range of new oral agents are now available. 00:42 Let's introduce thrombosis. 00:44 Thrombi are plugs consisting primarily of platelets and fibrin. 00:52 And of course, the main clinical problem that arises from this is ischemia, lack of blood supply, that happens beyond the clot. 01:01 Now, thrombi may occur in either the arterial or the venous circulation. 01:07 An important term is thrombophilia. 01:09 That refers to the inherited predisposition to thrombosis. 01:14 Let's start by discussing arterial thrombosis. 01:17 These arise on areas of atherosclerosis, particularly when there is plaque rupture. 01:25 And the plaques formed in atherosclerosis break and platelet adhere to that site. 01:33 A platelet adhesion, aggregation, and release may actually serve to promote development of atherosclerotic lesions. 01:42 And that might be one reason why Aspirin is so effective in reducing the risk of atherosclerotic events. 01:50 But as well as ischemia, thrombosis may also lead to the release of emboli that flow to downstream vessels. 02:00 That's sometimes seen from atherosclerotic plaques in the neck, leading to emboli into the brain. 02:07 Atherosclerosis has been one of the major problems in human health over the last few decades, and we know a lot about the risk factors. 02:17 Cholesterol, hypertension, and smoking. 02:21 But there is some good news here, because the incidence and also the mortality from atherosclerotic disorders has decreased markedly in recent years as we serve to reduce those risk factors and control them. 02:37 Venous thrombosis has three classic risk factors. 02:42 It used to be known as Virchow's triad. 02:44 One is when the blood slows down. 02:48 Secondly, the blood may be hypercoagulable. 02:53 That's sometimes seen perhaps in pregnancy, or after surgery or trauma. 02:58 And finally, when the vessel wall is damaged, which can trigger the adhesion of platelets to that damage. 03:07 And you can see that those three factors often occur in patients in hospital beds after surgery. 03:14 Now, let's discuss inherited thrombophilia. 03:18 Because it's being shown that up to 30% of people who develop a venous thrombosis do have a genetic predisposition of thrombosis. 03:28 Now, to understand these disorders, we need to discuss the natural physiologic collectivity of something called protein C. 03:38 Look at that diagram on the right. On the top left, we can see thrombin. 03:45 Thrombin is a key molecule in the coagulation cascade, and it activated fibrinogen to lead to fibrin. 03:53 But as well as promoting coagulation, it also leads to inactivation of coagulation factors through a negative feedback pathway. 04:04 And the mechanism is represented there. It happens by a fascinating route. 04:10 Thrombin binds to a molecule on the surface of the endothelium called thrombomodulin. 04:16 Once it's bound, it can then activate protein C, which we can see in red. 04:24 Now, protein C needs protein S as a cofactor, but those two together can then inactivate the active forms of factor V and factor VIII, which are critical cofactors for coagulation. 04:42 So, you can see that C and S are very important in limiting the amount of active coagulation factors at the site of thrombosis. 04:53 And important inherited thrombophilia is Factor V Leiden, which we can now start to understand. 05:00 This is an inherited allele in the factor V gene, and it's very common in many populations. 05:08 Up to 3% of the population. 05:11 Perhaps, it's been selected in evolution, because it does provide a little bit more protection against bleeding problems. 05:18 But this allele at factor V makes factor V slightly more difficult to cleave by the activated protein C. 05:28 Heterozygotes have a five to eight-fold risk of thrombophilia from this disorder, whereas homozygotes have a huge 30 to 140-fold risk of thrombosis if they have a factor V Leiden from both their mother and their father. 05:48 Protein C or S can also be deficient. 05:53 These are rare disorders, and it's usually seen as an autosomal recessive inheritance from the mother or the father. 06:02 Sometimes, babies are born with protein C or S deficiency from both the mother and the father, and that's a very devastating disorder, which leads to very severe thrombosis in early life. 06:15 Antithrombin can also be deficient, and that's another thing that can be checked in test of thrombophilia. 06:25 Now, let's look at some of the risk factors in life that can put us at risk of developing thrombus. 06:33 This can be seen in a range of states. Some are listed there on the left. 06:39 Postoperatively, because of rest or increased coagulability of the blood, or indeed vessel damage. 06:47 Immobility. Many malignant disorders trigger excess blood coagulation. 06:54 Estrogen therapy and the use of the contraceptive pill can increase the risk of thrombosis. 07:01 Aging is a very important risk factor, and that is actually shown on the right, where you can see new episodes of venous thromboembolism plotted in terms of incidence on the Y axis against age on the X axis. 07:18 And you can see that very steep increase after the age of 60. 07:22 Antiphospholipid syndrome and myeloproliferative disorders also lead to an increased risk of thrombophilia. 07:31 How do we make the diagnosis of a thrombosis? Well, to investigate thrombophilia, we can look at the blood count to check the platelets, we can do clotting test, and we can also do genetic test to look for the presence of factor V Leiden or abnormalities in protein C or protein S. 07:54 A deep vein thrombosis is usually diagnosed initially by the clinical picture. 08:01 Very commonly in the lower leg. The calf may be swollen and warm. 08:06 There may be tenderness. But that's not a very reliable picture and we would need other tests before we would commit a patient to antithrombotic therapy. 08:16 D-dimers are fragments that are released off the blood clotting, and they are raised in patients with the vein thrombosis. 08:26 And imaging in the form of an ultrasound or perhaps MRI scan is also needed.
About the Lecture
The lecture Thrombosis – Thrombosis and Anti-Thrombotic Therapy by Paul Moss, PhD, OBE, FMed, FRCPath is from the course Hematologic Disorders.
Included Quiz Questions
Which of the following is a typical finding of deep vein thrombosis?
- Swelling, tenderness and warmth of the lower extremity
- Angina
- Decreased D-dimer concentrations in blood
- Sudden onset of cold and blue toes
- Purpura of the lower extremities
Which of the following is NOT a common risk factor for arterial thrombosis?
- Slowing down and stagnation of blood
- Cholesterol
- Hypertension
- Smoking
- Atherosclerosis
Which of the following inherited thrombophilias is seen in approximately 3% of the population?
- Factor V Leiden
- Protein C deficiency
- Protein S deficiency
- Antithrombin III deficiency
- Hemophilia
Which of the following is the mechanism whereby the factor V Leiden mutation causes a hypercoagulable state?
- Protein C is unable to cleave activated Factor V.
- Factor V is unable to cleave activated protein C.
- Protein C is unable to cleave activated protein S.
- Factor V is unable to cleave activated protein S.
- Factor V is unable to cleave activated antithrombin II.
Which the following tests is NOT used in the diagnosis of DVT?
- X-ray
- D-dimer
- MRI
- Ultrasound
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |