Playlist
Show Playlist
Hide Playlist
Thoracic Cavity
-
Slides Anatomy Thoracic Cavity.pdf
-
Reference List Anatomy.pdf
-
Download Lecture Overview
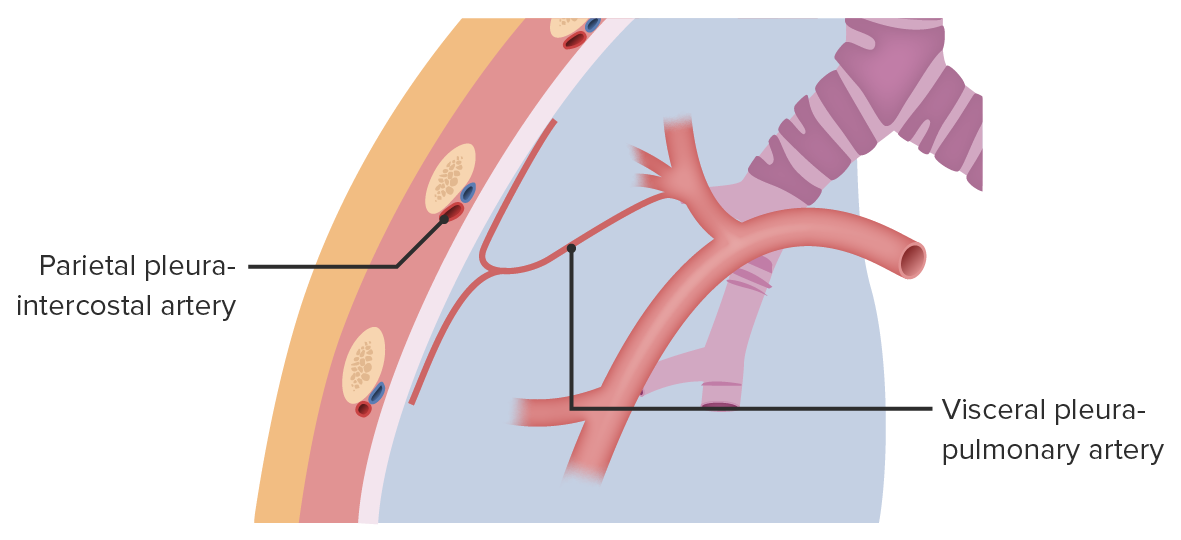
00:01 All right, now that we've seen the bones and muscles that surround the thoracic cavity, let's look at the thoracic cavity itself. 00:08 The first thing we'll notice is the diaphragm at the inferior edge. 00:14 The diaphragm is going to be pretty important because it's the primary muscle of inhalation. 00:19 And it also separates the thoracic and abdominal cavities from each other. 00:24 In fact, there was at one time, just a single large body cavity, and the diaphragm is actually what separated the thorax from the abdomen. 00:33 The next thing we'll see, coming down from the neck into the thorax is the trachea. 00:38 And it's going to branch into bronchi that supply the lungs, which are going to make up the majority of the volume of the thoracic cavity. 00:46 But there is this gap in between the two lungs in the middle called the mediastinum. 00:52 That's going to hold some pretty important structures to especially the heart. 00:57 If we turn our attention to this blue membrane, surrounding and lining the thoracic cavity, that's going to be the parietal pleura. 01:07 And if we trace it all the way to where the trachea and bronchi start to enter the lung, we see that it jumps off that area and turns green and becomes the visceral pleura. 01:19 Parietal pleura, means the pleura surrounding a cavity because parietal means wall. 01:25 So this is essentially the wall of the thoracic cavity. 01:29 Visceral refers to an organ. 01:31 So visceral means it's on the surface of the organ itself. 01:35 And these are the same terms you'll see in the abdomen when you talk about a different membrane called the peritoneum. 01:42 But otherwise, parietal and visceral mean the same thing whether you're talking about pleura, or peritoneum, in the thorax, or the abdomen. 01:49 In between the parietal and visceral pleura is a little space called the pleural cavity. 01:56 Normally, it's very small, but it's exaggerated here. 01:59 So you could actually appreciate that there is a space. 02:02 Normally, there's a very small amount of fluid called pleural fluid that exists in this cavity, which helps to reduce the friction between the two layers of pleura as the lungs expand to contract during breathing. 02:16 And then there's this area of the lung here little indentation where structures enter an exit called the hilum. 02:23 And that's a term you might hear in other organs where structures enter and exit. 02:27 For example, the kidney or the spleen, they both have a hilum. 02:32 Now, the visceral pleura, is largely insensitive to pain. 02:37 It doesn't have the right kind of innovation, but the parietal pleura does have what we call somatic innervation or innervation by regular spinal nerves. 02:44 So they are able to produce a very sharp type of pain if there's trauma or inflammation in that area. 02:53 And so different innervations affect different parts of the parietal pleura. 02:58 If we start at the area where the superior thoracic aperture is, it's relatively close to the neck, so we call that the cervical pleura. 03:07 And it's innervated by the nearby intercostal nerves. 03:11 Similarly, the parietal pleura underneath the ribs, it's called the costal pleura, and it's innervated by the surrounding intercostal nerves. 03:21 The pleura that lines the superior surface of the diaphragm is called the diaphragmatic pleura, and that's innervated by phrenic nerves. 03:29 Phrenic means diaphragm, first a diaphragm, and it's the same nerve that's going to provide the motor innervation to the diaphragm. 03:37 And then the portion of parietal pleura in the mediastinum is called the mediastinal pleura, and it's also innervated by the phrenic nerves. 03:44 And that's because we'll see that the phrenic nerves actually take a route through the mediastinum in order to reach the diaphragm. 03:51 Finally, you'll notice that there are a couple portions where the lungs don't quite fill the pleural cavity very well in the pleural almost forms a little double fold on itself. 04:02 And we call that a pleural recess. 04:07 So, if we take the lungs out in order to see the parietal pleura a little bit better, we can see how that cervical pleura is really high up. 04:17 It's right at the superior thoracic aperture. 04:20 We also see the costal pleura, as the name implies being right in the area of the ribs. 04:26 Diaphragmatic pleura, sitting over the superior surface of the diaphragm, and just were expected the mediastinal pleura right at the level of the mediastinum. 04:35 And here we see a little gap there. 04:38 That gap is where the parietal meets the visceral because that's where the lungs starting to make contact with the pleura here. 04:45 If we zoom in, we see that that gap is where something called the root of the lung is going to pass through. 04:51 And that stuff like the bronchus, the pulmonary artery, and the pulmonary veins. 04:55 All collectively called the root going through this gap. 05:00 And the parietal pleura in this area forms this little double fold that extends inferiorly to form this anatomic landmark called the pulmonary ligament. 05:11 And if the lung was there, it would line up perfectly with this opening with its hilum, because that's the indentation or depression in the lung where these structures are going to enter an exit. 05:24 So let's put some of those things in so you can actually see the root of the lung a little bit better. 05:29 First, we see the trachea. 05:31 Coming down before branching into the right and left mainstem bronchi. 05:36 We have the pulmonary trunk coming from the heart, divided into the right and left pulmonary arteries. 05:44 And coming back from the lungs to the heart, we have the right and left pulmonary veins. 05:51 And after it's wrapped around this route of the lung, the pleura here forms that double fold inferiorly that we call the pulmonary ligament. 06:01 So, there's a few other quirks that are worth talking about when it comes to the pleura, especially when we're looking at the cervical pleura. 06:09 So, the cervical pleura is relatively exposed at the superior thoracic aperture. 06:16 It's relatively unprotected by bone here. 06:19 So, it's covered by a thick connective tissue called the suprapleural membrane to give a little more added protection. 06:27 Another term you might hear is a reflections. 06:30 So a pleural reflection is where the junctions of these different pleura meet up. 06:36 For example, we have the sternal line of reflection, where the mediastinum and costal meet anteriorly. 06:44 We have the costal line of pleural reflection, where the costal pleura meets the diaphragmatic pleura inferiorly. 06:54 And then we have the vertebral line of reflection where the costal meets the mediastinal posteriorly. 07:02 We mentioned gaps where the lungs don't completely fill as pleural recesses. 07:07 So let's look at a couple of these pleural recesses. 07:11 One prominent one is out laterally where it forms a very sharp angle called the costodiaphragmatic or costophrenic recess. 07:20 And if you have too much pleural fluid, something called a pleural effusion, and you're sitting or standing upright and you get an x ray fluids going to accumulate in this recess. 07:31 In fact, you'll hear the term from a radiologist very commonly called blunting of the costal phrenic angle, and decoding that is saying, anatomically, that recess is filled with excess pleural fluid. 07:45 There's another one more mediately, the costomediastinal recess, but it's quite a bit smaller and a lot less clinically relevant. 07:54 Finally, let's talk about those nerves briefly. 07:57 The phrenic nerves are pretty interesting and have a pretty interesting embryologic development. 08:03 And you can kind of see that in action by how long they are. 08:07 They actually originate up in the cervical area coming from cervical spine C3, 4, 5, and then descend through the mediastinum to reach the diaphragm. 08:18 So while their major job is motor innervation of the diaphragm, they actually innervate a lot of things along the way to provide sensory information. 08:26 And we already seen that with the mediastinum and diaphragmatic pleura.
About the Lecture
The lecture Thoracic Cavity by Darren Salmi, MD, MS is from the course Thorax Anatomy.
Included Quiz Questions
Where does pleural fluid reside?
- Pleural cavity
- Visceral pleura
- Parietal pleura
- Diaphragm
- Mediastinum
What is one difference between the parietal and visceral pleura?
- Only the parietal pleura has somatic innervation.
- The parietal pleura is composed of mesothelial cells and the visceral pleura is composed of epithelial cells.
- Only the parietal pleura is adjacent to the pleural cavity.
- Only the visceral pleura is derived from the lateral plate mesoderm.
- Only the visceral pleura is adjacent to the pleural cavity.
What structure innervates the diaphragm?
- Phrenic nerve
- Intercostal nerve
- Vagus nerve
- Celiac plexus
- Superior mesenteric plexus
Where does fluid from a pleural effusion collect?
- Costodiaphragmatic recess
- Pulmonary ligament
- Hilum
- Pleural fold
- Costomediastinal recess
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |