Playlist
Show Playlist
Hide Playlist
Systemic Inflammatory Response Syndrome – Special Devices (ICU and Brain Death Determination)
-
14 -Special devices in the ICU and brain death.pdf
-
Download Lecture Overview
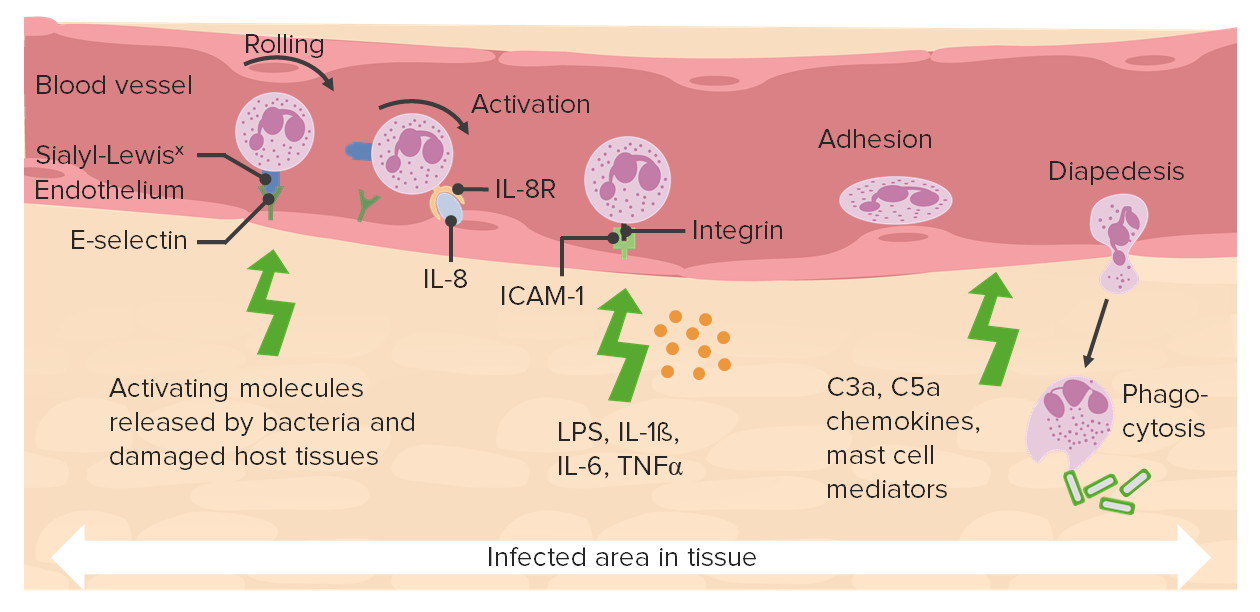
00:00 So systemic inflammatory response syndrome is a relatively new diagnosis, although it's been around for a long time and it's often but not always associated with sepsis, it's part of a syndrome that may lead to septic shock and death, but not always. 00:19 It's associated with a general breakdown of the body's immune system with the development of generalized tissue inflammation. 00:26 And we really don't understand this process. 00:29 It's not always related to infection. 00:32 But in a nonspecific response to ischemia, loss of oxygen, trauma, inflammatory processes or infection. 00:42 It's part of a continuum, and it's often seen as the presenting condition of this problem. 00:50 So the diagnostic criteria for the SIRS continuum are SIRS, sepsis and septic shock, follow this pattern. 00:59 For SIRS criteria, you need two criteria, either a temperature greater than 38 °C, a heart rate greater than 90, a respiratory rate greater than 20 or PaCO2 of less than 32. In other words, the patient's really working at breathing and a white blood count that's greater than 12,000. 01:21 So you need two of those to make the diagnosis of SIRS. To take the next step and make the diagnosis of sepsis, updated guidelines now take into account the Sequential Organ Failure Assessment, or SOFA. 01:32 This assessment scores each organ system, based on a corresponding indicator. 01:36 For example, the respiratory system is assessed by P/F ratios, coagulability is assessed by plate account, liver function is assessed by bilirubin, cardiovascular by blood pressure, brain by the Glasgow coma score and renal function by creatinine levels. 01:52 In order to meet the criteria for sepsis, patients must now have an increase of two or more points in their SOFA score. 01:59 Septic shock is the next step in this very bad condition, this is sepsis with hypotension despite adequate fluid resuscitation. 02:08 So in a situation where you're sure you have fluid resuscitated adequately and you still have hypotension, you've got severe shock criteria. 02:18 And then the final stage of this is, prior to death, in many cases, unfortunately, is multiple organ dysfunction syndrome. 02:27 So everything above, plus the evidence of more than two organs failing. So cardiac, respiratory, renal, any two organs, often liver failure, at this point. Treatment is very aggressive and starts with early antibiotic therapy. 02:45 Every delay in administering antibiotics increases mortality by eight percent. 02:52 That's an amazing statistic. 02:54 A one-hour delay in starting antibiotics increases the likelihood the patient's going to die by eight percent. 03:03 Effective hemodynamic support is essential but difficult, the current drug of choice is norepinephrine or noradrenaline is the other name for it, and it's given intravenously, obviously, but in very high doses in some of these patients. The third step is effective volume management. 03:21 This is also important to use the best fluid replacement substance and this is very controversial. 03:29 So artificial colloid, albumin, normal saline, balanced salt, high concentration saline, 3% or 5% saline, which are the right agents to use, or hypotonic solutions. 03:42 It's all extremely controversial, and it has been for 40 or 50 years. 03:46 I've read documentation from after the Second World War showing that the right fluid at the right time has been a challenge for medical people for a very long period of time. The best fluid is not known, but maintenance of normal or slightly high central venous pressure appears to be the best path, irrespective of the fluid used.
About the Lecture
The lecture Systemic Inflammatory Response Syndrome – Special Devices (ICU and Brain Death Determination) by Brian Warriner, MD, FRCPC is from the course The ICU.
Included Quiz Questions
Which of the following does multiple organ dysfunction criteria include?
- Evidence of at least 2 organs failing
- Hypotension and tachypnea only
- Hypotension, tachypnea, and source of infection only
- Lactic acidosis and hypotension only
- Organ dysfunction and hypotension only
If antibiotic therapy is delayed, by what percentage per hour is the chance of mortality increased?
- 8%
- 16%
- 22%
- 28%
- 30%
What is the drug of choice in the hemodynamic support of the SIRS continuum?
- Norepinephrine
- Epinephrine
- Dopamine
- Dobutamine
- Adenosine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |