Playlist
Show Playlist
Hide Playlist
Pancreatitis
-
Slides Pancreas General Surgery.pdf
-
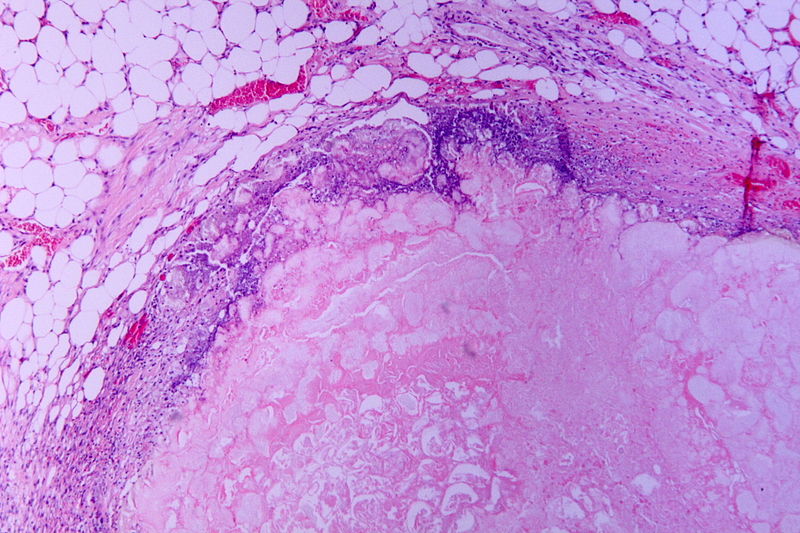
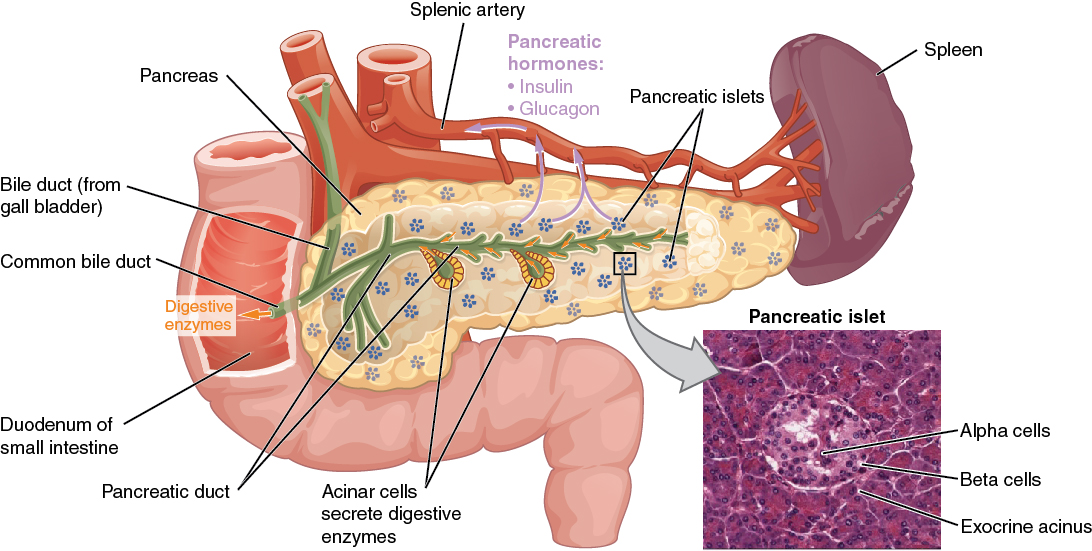
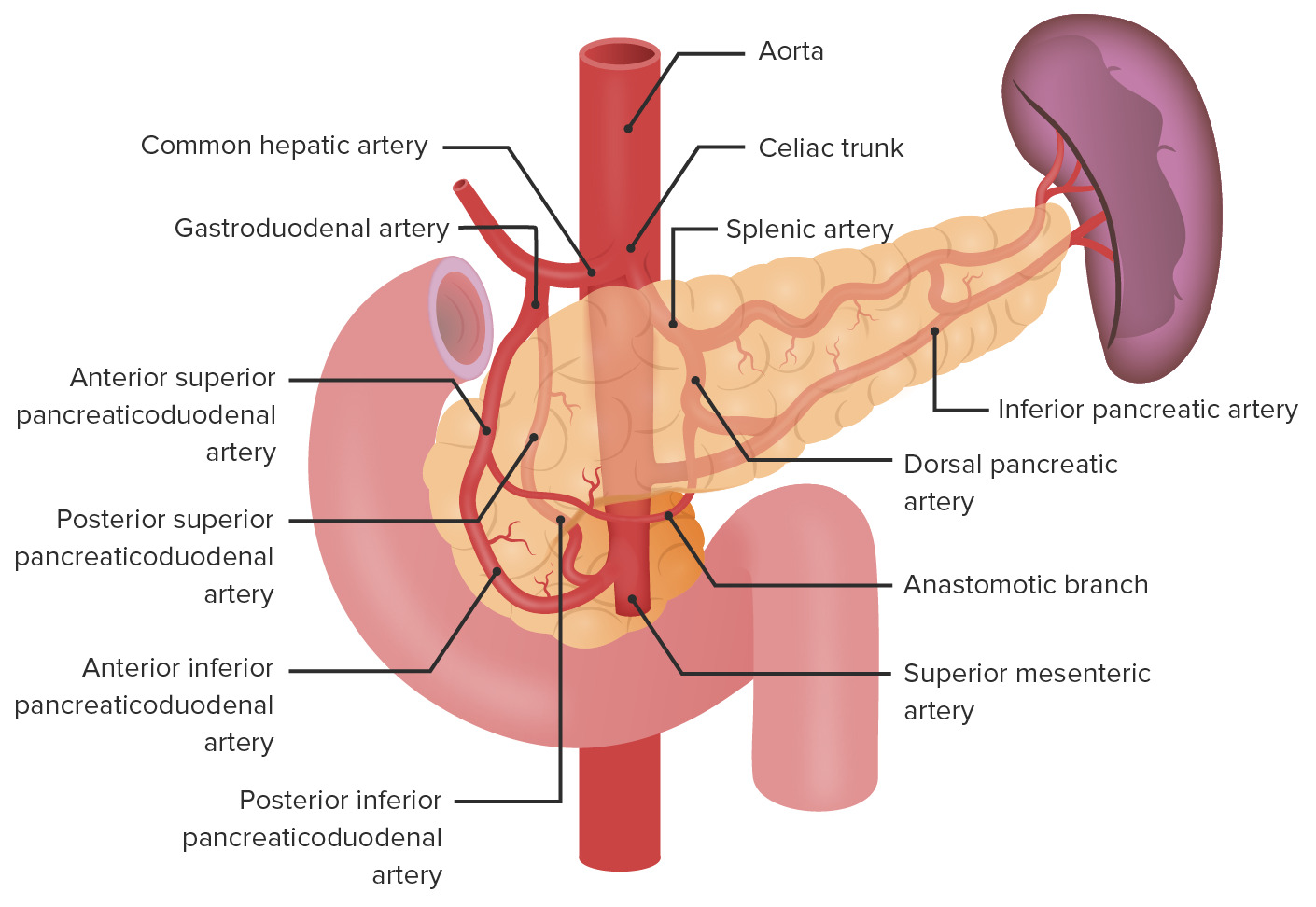
Download Lecture Overview
00:01 Welcome back. Thanks for joining me in this discussion of pancreas under the section of general surgery. 00:08 Our discussion of pancreas starts with pancreatitis. Most common etiologies of pancreatitis in the United States include alcohol and biliary diseases specifically gallstones disease. 00:23 The chronicity of pancreatitis is incredibly important. In the acute setting, pancreatitis can quickly deteriorate into something that causes severe sepsis and hemodynamic instability. Patients with chronic pancreatitis may develop chronic changes to the pancreas and destruction of the duct system. 00:45 That leads to chronic exocrine and endocrine pathologies. It is not completely understood why alcohol causes acute pancreatitis. For biliary diseases specifically gallstones, the gallstones can escape the gallbladder, obstruct the common bile duct and specifically at the confluence of the pancreatic duct and the common bile duct. This leads to obstruction of the pancreatic ducts and autodigestion and just destruction of the pancreas. There’s also an association of smoking, hypertriglyceridemia, and of course post procedural. In this image, you see an ERCP as discussed previously in other lectures. 01:31 Another risk-factor is the usage of different drugs, such as Didanosine, Tetracyclines or 5-ASA. 01:39 What are some common findings for patients who present with pancreatitis? The vast majority of patients experience abdominal pain specifically in the epigastrium and very classically described as radiating to the back. Patients may present with nausea or vomiting, although it’s not 100%. 01:57 Oftentimes, patient lack appetite. Epigastric tenderness is the classic location for pain. But remember especially with severe pancreatitis, the pain can be diffuse in nature when the entire peritoneum is irritated. 02:17 Laboratory values may be of assistance. The chemistries may actually be normal. Particularly in acute necrotizing pancreatitis, one may see an elevation of the white blood cell count or leukocytosis. 02:31 Liver function tests are commonly obtained for patients who come in with abdominal pain. 02:38 You may see a normal or elevated total bilirubin depending on whether or not the common bile duct is obstructed. Amylase and lipase are typically elevated as is alkaline phosphatase particularly in the setting of obstruction. It’s important to note Ranson's criteria as a prognostic value for how the patient will do in the hospital with acute pancreatitis. Ranson's criteria is broken down into two parts. The first set of Ranson's criteria is determined on admission. These parameters include leukocytosis greater than 16,000, age greater than 55, glucose greater than 200, AST greater than 250, and LDH greater than 350. Within 48 hours, Ranson’s criteria is reassessed on patients with acute pancreatitis. In this setting, we’re specifically looking for how much resuscitation the patient has gotten. We might see a hematocrit drop greater than 10% as a sign of fluid retention and potentially marker of more severe disease; a BUN rise greater than 5; calcium less than 8; arterial pO2 as obtained by an arterial blood gas or ABG less than 60mmHg; and lastly and very importantly, a base deficit greater than 4 or greater than 6L of fluid resuscitation. 04:13 The common thing through all of these Ranson’s criteria is to suggest to you that if a patient with acute pancreatitis receives a very aggressive resuscitation or extensive resuscitation, they may have more severe disease and may lead to complications. Are there any imaging studies that we can use to diagnose pancreatitis? Ultrasound is often used when patients present with epigastric or right upper quadrant abdominal pain specifically to evaluate for gallstones. 04:44 What’s more commonly used as you see in this image is a CT scan or cross sectional imaging of the abdomen and pelvis to evaluate for pancreas. It’s important to know however, that obtaining a CT scan of the abdomen and pelvis should not be routinely done for a diagnosis of acute pancreatitis unless there are two scenarios. One, the diagnosis of the epigastric abdominal pain is uncertain. 05:08 You’re looking for other potential etiologies of abdominal pain. Two, the patient looks quite ill and you’re concerned for severe necrotizing or severe acute pancreatitis.
About the Lecture
The lecture Pancreatitis by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following is NOT a known risk factor for pancreatitis?
- Hypercholesteremia
- Alcoholism
- Severe hypertriglyceridemia
- Common bile duct stones
- Endoscopic retrograde cholangiopancreatography (ERCP)
Which statement about the presentation of pancreatitis in a patient is FALSE?
- Abdominal pain is always localized to the left upper quadrant.
- Pancreatitis associated pain can be felt diffusely over the entire abdomen.
- Nausea and vomiting are often present.
- Loss of appetite is often present.
- Epigastric tenderness can be observed on exam.
On serum analysis of pancreatitis, which of the following elevated lab values suggest common bile duct obstruction?
- Elevated total bilirubin
- Elevated amylase
- Elevated lipase
- Elevated white blood cell count
- Elevated lactate
A 58-year-old man with a past medical history of alcoholism and previous hospital admissions for pancreatitis presents to the emergency room with severe diffuse abdominal pain that radiates to his back, nausea, and vomiting. On exam, he has tachycardia and a blood pressure of 110/60 mm Hg. He appears dehydrated and is tender all over his abdomen with maximal point tenderness in the epigastric region. Labs are as follows: lactate of 2.4 mmol/L, white blood cell count of 20,000/uL, glucose of 210 mg/dL, alanine transaminase (ALT) of 180 units/L, aspartate transaminase (AST) of 260 units/L, and lactate dehydrogenase of 380 units/L. What is this patient’s initial Ranson score on admission?
- 5
- 6
- 4
- 3
- 2
In which of the following cases of pancreatitis should a CT scan be obtained?
- Suspicion of necrotizing pancreatitis
- Pancreatitis caused by gallbladder stones
- Pancreatitis caused by alcohol intake
- Pancreatitis following scorpion bite
- All cases of pancreatitis require CT imaging to confirm diagnosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |