Playlist
Show Playlist
Hide Playlist
Subarachnoid Hemorrhage: Etiology, Clinical Manifestations, and Diagnosis
-
Slides Head Trauma Subarachnoid Hemorrhage.pdf
-
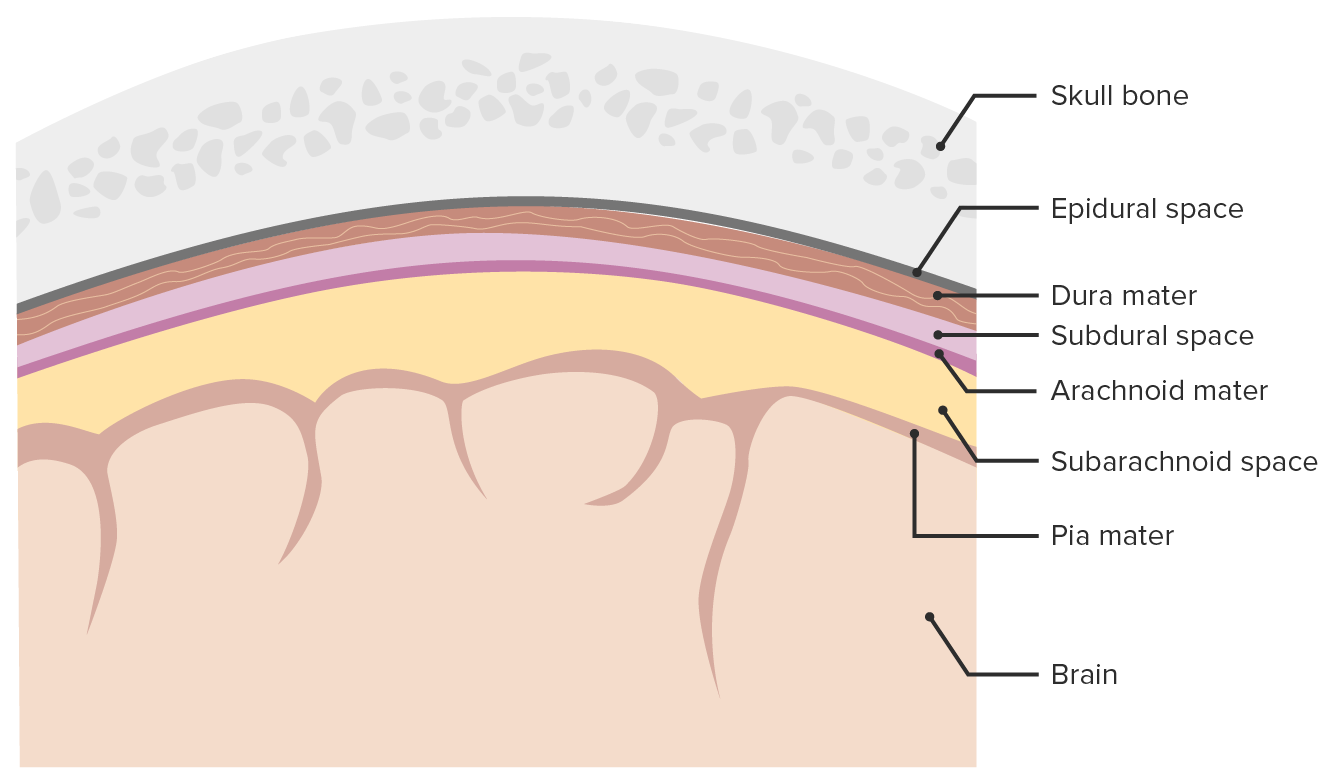
Download Lecture Overview
00:01 So let's talk a little bit more about subarachnoid hemorrhage and understand how we evaluate and manage those patients. 00:07 Subarachnoid hemorrhage is a type of stroke. 00:10 It's a type of cerebrovascular accident. 00:13 And it results from intracranial hemorrhage into the subarachnoid space between the arachnoid and the pia mater layers that are surrounding the brain. 00:22 As we look at that schematically, where is the blood and what is happening. 00:26 Again, here we see the bones out on the surface and we move down into the parenchyma inferiorly and the subarachnoid blood is developing in the subarachnoid space. 00:36 This is right out on the surface of the brain and we can see problems with increased intracranial pressure as a result of decreased CSF reabsorption and other problems as a result of location of the blood. 00:50 In terms of epidemiology, subarachnoid hemorrhage is a type of hemorrhagic stroke. 00:55 Hemorrhagic strokes account for 15-20% of the cerebrovascular accidents. 01:00 The majority of strokes are ischemic, but this small portion up to 15-20% of strokes are hemorrhagic. 01:08 50% of hemorrhagic strokes are due to subarachnoid hemorrhage. 01:11 The other 50% of hemorrhagic strokes are intraparenchymal hemorrhages. 01:17 When we think about subarachnoid hemorrhage, we want to think about trauma and aneurysms. 01:22 Saccular aneurysms or outpouching of the blood vessel increased the risk of subarachnoid hemorrhage. 01:28 Rupture of a saccular aneurysm is one of the most common causes of subarachnoid hemorrhage. 01:33 And you can see that depicted on the schema here. 01:35 We have a normal blood vessel at the bifurcation or just distal to the bifurcation. 01:40 We have this circular outpouching of the blood vessel and then extrusion of blood out of the surface of that aneurysm contributing to subarachnoid hemorrhage. 01:49 And this bifurcation area is often where we see aneurysms as a result of the flow and abnormal flow of blood that can occur and the intensity of the blood pressure around those bifurcation areas. 02:03 3-5% of the population may have radiographic evidence of an unruptured saccular aneurysm but the vast majority will not rupture. 02:12 So just because you have an aneurysm doesn't mean it will rupture. 02:15 And we use the size and the appearance and the location to guide us in terms of whether patients should undergo preventative intervention to prevent a rupture or they should be monitored. 02:26 Trauma is a trigger for potential rupture of an aneurysm in addition to being a cause of subarachnoid hemorrhage, even in patients without an aneurysm. 02:35 And 15-20% of subarachnoid hemorrhages are non-aneurysmal. 02:39 So a patient presents with a subarachnoid hemorrhage, we look for an aneurysm and don't find it. 02:43 Then we need to think about trauma or other vascular abnormalities. 02:49 What's the clinical presentation for subarachnoid hemorrhage? Well, one I want you to think about thunderclap headache. 02:55 That is the severe, sudden worst headache of my life that began rapidly and the rapidity of onset of that severe worst headache of my life is what makes it a thunderclap headache. 03:06 This is sudden in onset, it begins in seconds, and patients typically describe that the worst headache of their life really began in seconds. 03:14 And that's indicative of a thunderclap headache and should prompt evaluation for subarachnoid hemorrhage. 03:20 We can see other symptoms, neck stiffness and pain as a result of meningeal irritation. 03:25 This correlates with spreading of blood into the CSF causing meningeal irritation. 03:30 Often presents hours after the onset of headache. 03:32 We can see altered loss of consciousness from increased ICP. 03:36 Seizures as a result of blood being right on the cortical surface and nausea/vomiting from increased ICP as well. 03:44 How about the diagnosis? We diagnose subarachnoid hemorrhage the same as we do every other type of intracranial hemorrhage with a non-contrast head CT. 03:52 And this is really the cornerstone of how we evaluate hemorrhages and subarachnoid hemorrhage. 03:57 CT has a sensitivity of up to 100% if performed within the first 6 hours of presentation. 04:04 And so patients who present suddenly and we see a non-contrast head CT, if it shows subarachnoid hemorrhage, that's what it is. 04:10 If it doesn't, it's very unlikely to be that. 04:14 And that is if reviewed by a qualified neuroradiologist. 04:17 But sometimes CT can miss a subtle subarachnoid hemorrhage or a sentinel bleed, a small bleed from an aneurysm that then stops. 04:25 And in those cases, additional evaluation may be needed and we'll talk about that in just a minute. 04:31 CT scan should include cuts through the base of the brain. 04:34 We want to look at the base of the brain around the blood vessels where we can see aneurysms and subarachnoid develop. 04:40 Locations of blood in subarachnoid hemorrhages include the Basal cistern which is the most common, Sylvian fissure, the interhemispheric fissure and interpeduncular fossa and here we're looking at an image of subarachnoid blood in addition to intra ventricular blood resulting in significant increase in intracranial pressure and ventriculomegaly unlikely in a patient who is comatose. 05:04 In addition to CT, evaluation of subarachnoid hemorrhage can include a lumbar puncture and historically this was very important in the evaluation of subarachnoid hemorrhage. 05:13 As the sensitivity and specificity of CT hadn't improved, we see less spinal taps needed for evaluation of these patients. 05:21 This should be performed if there's a high index of clinical suspicion for subarachnoid hemorrhage. 05:27 And typically we see elevation and opening pressure and an elevation in the red blood cell count. 05:33 Importantly, sometimes we can see an elevated red blood cell count in the first tube as we insert the needle that clears over time. 05:41 And that's a traumatic tap, where we hit a blood vessel on the way in, we see that blood in the first tube and we see that it goes down over time. 05:49 When we see blood in the first tube and the same blood in the second and third and fourth tube as we collect the spinal fluid that suggests some intrinsic production of blood in the spinal fluid. 05:58 And that's the signature for what we see with subarachnoid hemorrhage. 06:01 Occasionally, amount of blood in the subarachnoid space and CSF is small and we may just see a xanthochromic cerebrospinal fluid which would also support concern for a sentinel bleed or subarachnoid.
About the Lecture
The lecture Subarachnoid Hemorrhage: Etiology, Clinical Manifestations, and Diagnosis by Roy Strowd, MD is from the course Head Trauma.
Included Quiz Questions
What term describes an intracranial hemorrhage between the arachnoid and the pia mater?
- Subarachnoid hemorrhage
- Subdural hematoma
- Subgaleal hematoma
- Intraventricular hemorrhage
- Epidural hematoma
What is the most common non traumatic cause of subarachnoid hemorrhage?
- Rupture of a saccular aneurysm
- Trauma
- Amyloidosis
- Cocaine use
- Hemorrhagic transformation of ischemic stroke
What symptoms should prompt concern for subarachnoid hemorrhage?
- Thunderclap headache
- Nystagmus
- Neck stiffness
- Dizziness
- Lethargy
What is the most common location of bleeding in patients with a subarachnoid hemorrhage?
- Basal cisterns
- Cerebral peduncles
- Lateral ventricles
- Fourth ventricle
- Transverse sinus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |