Playlist
Show Playlist
Hide Playlist
Statin Myopathy
-
Slides Toxic Myopathies.pdf
-
Download Lecture Overview
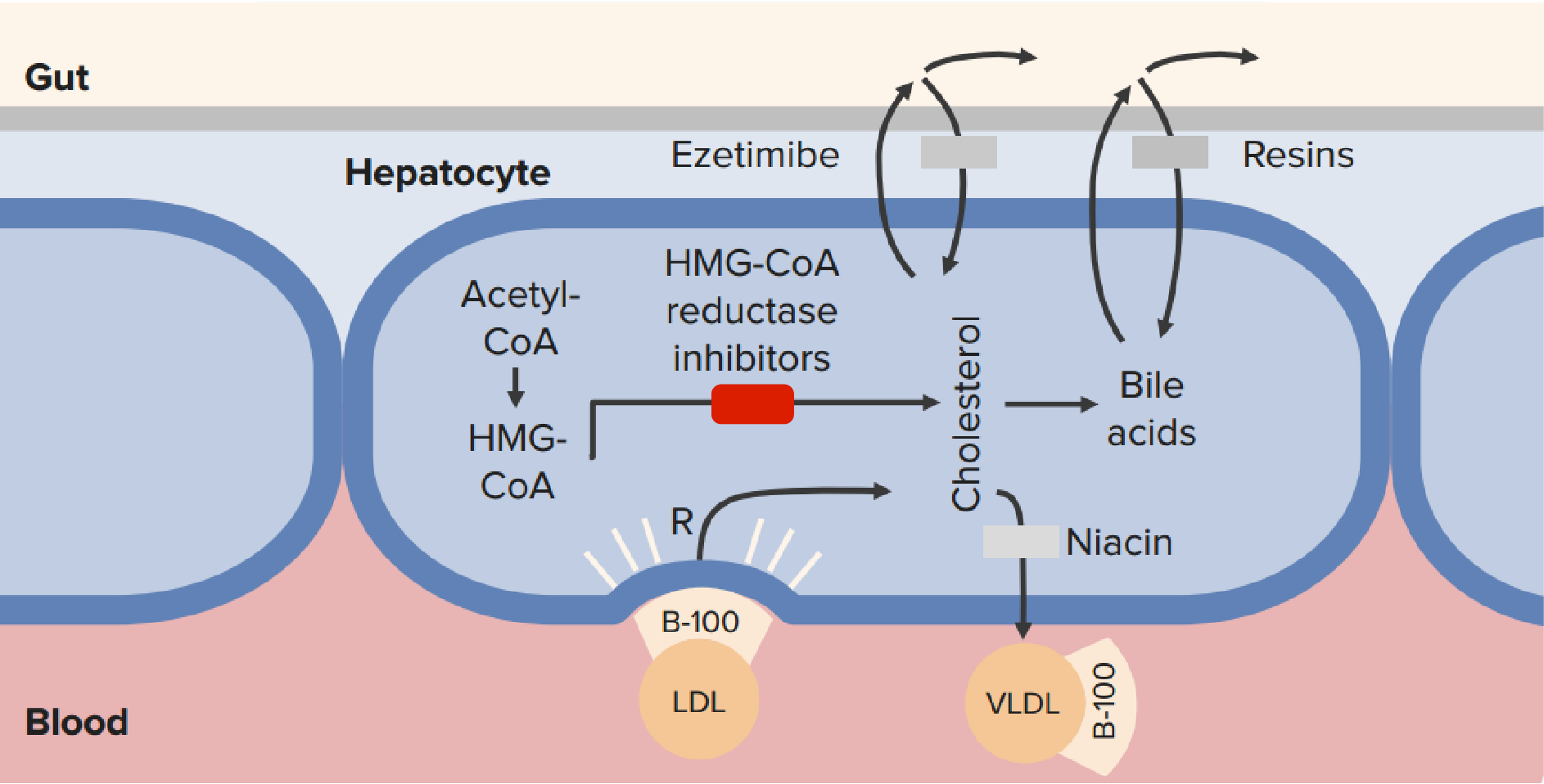
00:00 Now let's move to statin associated myopathies, are really critical cause of toxic myopathies. 00:07 Statin myositis or statin myopathy can range from mild myalgias to severe myopathy with varying degrees of inflammation in between and the goal of our testing and assessment evaluation of patients is to figure out whether this is a mild myalgia that the patient can be treated through, a more severe myositis that we need to treat or withdraw drug, or a potential autoimmune myopathy that could have been precipitated by the statin medicine and needs more prolonged treatment. And that will be the goal of our evaluation and management of these patients. What's the typical presentation of a statin associated myopathy? Well, it's a myopathy so we see that typical distribution, proximal more than distal weakness, myalgias are common and as we're seeing myalgias are more common in toxic myopathies than with the inflammatory myopathies. Typically, this occurs weeks after initiation but it can be months after initiation of the statin. It's an idiosyncratic reaction. It can occur at any point in time in that statin therapy. The workup includes assessment of CK and we do see an elevated CK. This is the second toxic myopathy that causes elevated CK, hypothyroid myopathy, and statin myopathy. Two exceptions to our general rule. We can see increased liver enzymes and typically this resolves within 4-6 weeks after discontinuation of the statin medication. So let's look at the typical presentation. We said statin myopathies fall on a spectrum from asymptomatic or mild disease to more moderate or severe disease. 01:46 What do those look like in patients? Well, asymptomatic disease is mild. It may even be asymptomatic, patients may not have any symptoms and we see elevated CK levels and we'll talk about how to manage those patients. Mild disease typically includes mild weakness, occasionally cramps, maybe myalgias and the CK is also elevated. That elevation of CK in a patient who is on a statin should tip us off that there is a myopathic process going on. 02:15 Moderate disease shows up with prominent myalgias and more significant weakness, elevation in CK which may persist even after the statin medicine is withdrawn. And severe presentations include rhabdomyolysis and we'll talk more about this later in the lecture but this is widespread generalized myonecrosis with substantial increase in CK and risk of renal dysfunction. So what's the risk of a statin associated myositis with various statin medications? You can see that here and this is not an exact science, but some good rules of thumb. Certain statins are associated with a less common risk of developing a statin associated myositis and you see that here with fluvastatin and pravastatin. Others are more commonly associated with myopathy and that would be atorvastatin and simvastatin. And so you can see fluvastatin and 5% of patients may develop myopathy, pravastatin 10%, 14% and 18% with simvastatin so varying degrees of risks associated with different medications that we use to lower cholesterol. What are some risk factors for developing a statin associated myositis? Well we group those into endogenous risks, things that are present within the patient and exogenous risks, things that can change over time. In terms of the exogenous risks, alcohol consumption increases the risk of developing a statin myopathy, heavy exercise use, surgery particularly surgery whether it's severe metabolic shifts or demands during that, certain drugs particularly those that affect the cytochrome P-450 system and you can see many of those here, as well as consuming certain amounts of grapefruit juice. Endogenous risks are things that are intrinsic to the patient. Older age, age greater than 65 is associated with a higher risk of developing a statin myopathy; decreased body mass index; multisystem disease particularly renal or hepatic dysfunction; certain metabolic diseases can increase the likelihood of a myopathy particularly in the setting of statins; hypertriglyceridemia; family history of muscular symptoms; past medical history of increased CK which may indicate risk of inflammation within the muscle; and then thyroid disorders. So some of these we can prevent and mitigate and manage, others we cannot and we need to understand the patient's risks as we start these medicines. How do we evaluate statin myopathy? In this series of schematic diagrams is really important for understanding how we approach patients and a clinical vignette and manage a patient who has developed a statin associated myopathy. The first thing we look at is what's the degree of elevation of the CK. Is the CK normal or is it less than 4 times the upper limit of normal? In cases where it is where there is milder muscle inflammation, the presence of myalgias is key. As we saw in symptomatic patients we see myalgias, in asymptomatic patients we don't. So if the patient doesn't have myalgias, we continue the statin medicine with close monitoring of the CK level and usually liver enzymes. 05:23 When myalgias are present, the statin should be stopped for around 2-4 weeks to see if the condition resolves, if the CK goes back to normal and the patient has improvement of symptoms and resolution of the myalgias. Those patients can be rechallenged either with a dose reduction or switching agents to one of those drugs that is less commonly associated with myopathy. Or we can move to a different drug class, another agent that will lower cholesterol but in a different way, an agent that's not a statin. Other patients may present with substantial elevations in CK greater than 4 times the upper limit of normal. And we need to be careful here to differentiate between a statin associated myopathy and uncovering an underlying necrotizing autoimmune myopathy. In patients who have CK greater than 4 times the upper limit of normal, the first question is "Is there evidence of rhabdomyolysis? Is there elevation in kidney values, elevation in creatinine? Is there hematuria? Is there prominent muscle breakdown that would suggest that the patient's developing rhabdo?" If that's the case, we need to proceed to early antibody testing which we'll talk about in just a minute. If there's no evidence of rhabdomyolysis, the statin medicine should be stopped for about 6-8 weeks and then reevaluate. Patients who still have a deficit, weakness, or some other deficit at the end of 6 weeks should undergo additional testing. At the end of 6 weeks, we want to see if the patient has returned to normal and if the patient has returned to normal, they can be rechallenged. If not, again, additional testing is required and the testing that we perform is looking for anti-HMG-CoA reductase antibodies. We talked about this briefly in the lecture on inflammatory myopathies. These enzymes, these antibodies are seen in patients with necrotizing inflammatory myopathy. This is an autoimmune myopathy where the antibodies cause and contribute to muscle damage. If the antibodies are negative, we continue to watch the patient, look for resolution of the CK and symptoms. If there is persistent increase in CK or ongoing symptoms, the patient needs a biopsy. In patients who have positive anti-HMG-CoA reductate antibodies, biopsy should be performed to evaluate for underlying necrotizing myopathy. So this is a very important diagram for evaluating patients who present with statin associated myopathies. Let's talk about HMG-CoA reductase associated myopathy again. As you recall, this is an immune-mediated myositis or necrotizing autoimmune myopathy. This results from autoreactive HMG-CoA reductase antibodies and it may be precipitated by statin use. And as you saw on the last slide, statin initiation is then withdrawn and when the inflammation within the muscle continues, we start to worry about this condition. How does it present? Patients present with prominent myalgias, CK is elevated, it's an inflammatory myopathy and immune mediated myopathy. Proximal weakness is common. 08:35 You can see that in the figure here. Proximal shoulder girdle as well as proximal leg muscle weakness and the key is that this persists after discontinuation of statin use.
About the Lecture
The lecture Statin Myopathy by Roy Strowd, MD is from the course Acquired Neuromuscular Diseases.
Included Quiz Questions
Which statin drug is associated with the highest risk of myopathy?
- Simvastatin
- Pravastatin
- Fluvastatin
- Atorvastatin
- Rosuvastatin
Which antibody is associated with statin-induced necrotizing autoimmune myositis?
- Anti-HMG-CoA reductase antibody
- Anti-Jo-1 antibody
- Anti-double-stranded DNA antibody
- Anti-Mi-2 antibody
- Anti-nuclear antibody
What is the first step in the management of statin-induced myopathy in a patient whose creatine kinase value is more than four times the upper limit of normal?
- Ruling out rhabdomyolysis
- Ruling out necrotizing autoimmune myositis
- Lowering the drug dose
- Changing to another lipid-lowering agent
- Stopping the drug for 6–8 weeks
Which of the following clinical features is associated with mild statin myopathy?
- Myalgia
- Myxedema
- Persistence of muscle weakness after statin withdrawal
- Renal impairment
- Metabolic acidosis and electrolyte abnormalities
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |