Playlist
Show Playlist
Hide Playlist
Seronegative Spondyloarthropathies & Ankylosing Spondylitis (AS)
-
Rheumatology I 02 Seronegative Spondylarthropathies.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
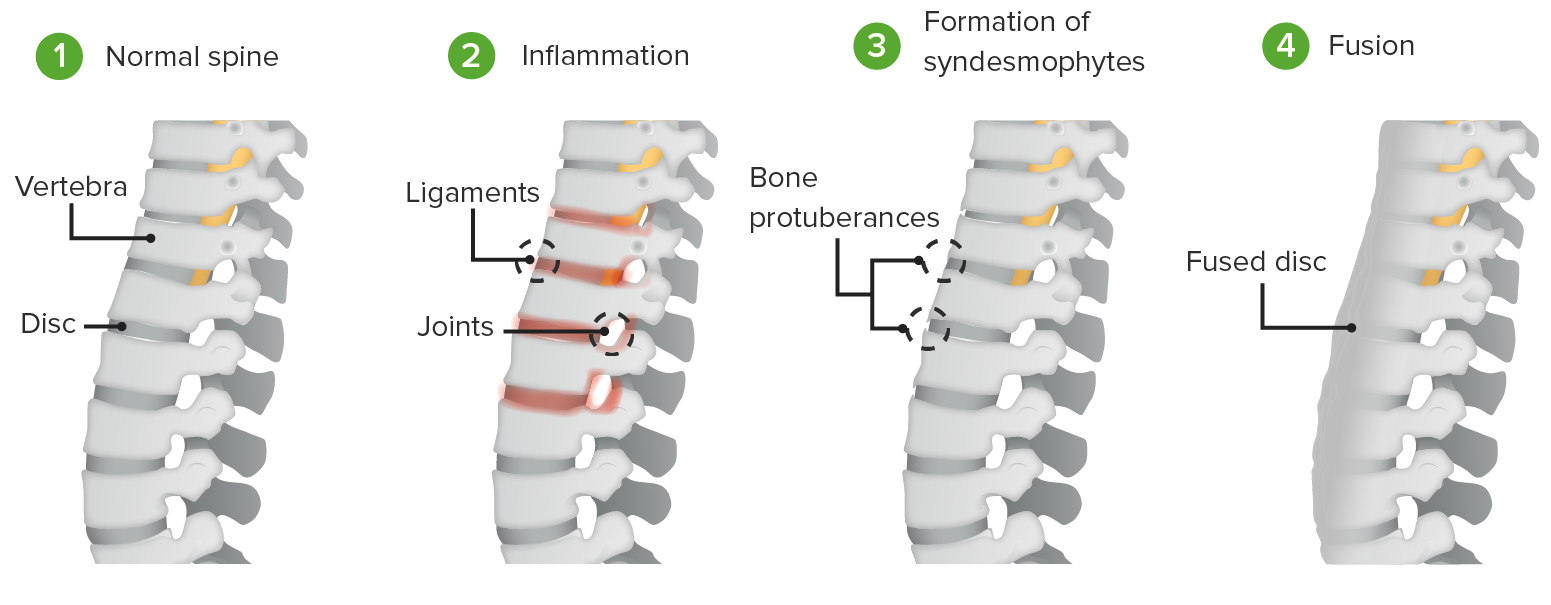
00:01 In this section, we'll take a look at seronegative spondyloarthropathies under rheumatology. 00:08 Things that you wanna keep in mind as we move forward here are the following. 00:12 Seronegative refers to the fact that well, rheumatoid factor is negative in these conditions we'll take a look at. 00:18 Next. There's a particular type of seronegative spondyloarthropathy known as -- well, you probably have heard of Reiter's syndrome. 00:26 But now we call it reactive arthritis more clinically. 00:31 And you'll be comparing this to septic arthritis that we had a discussion prior. 00:36 Under seronegative spondyloarthropathy. 00:40 The common feature that we're going to find in all of these include the fact that you'll have bone issues in the vertebrae. 00:48 You have back pain. The differentials will include ankylosing spondylitis. 00:54 Then, you'll have a young male most commonly who will then have vertebral issues. 01:00 Reactive arthritis, formally called Reiter's syndrome. 01:05 This is the one perhaps that you've come to know as being can't see, can't pee and can't climb a tree. 01:13 And I'll tell you what those mean as we move forward. 01:16 Psoriatic arthritis. Some every patients, maybe about 15 to 30% of them. 01:23 When they have the salmon colored plaques on the skin, and they also have vertebral issues, and I'll show you an x-ray of the hand, you would then call that psoriatic arthritis. 01:36 These are seronegative. 01:38 All of these patients, these four classification or differentials will have HLA-B27 to be positive. 01:46 But the rheumatoid factor will come back to be negative. And then enteropathic. 01:50 When you talk about enteropathic type of arthritis, then you're thinking about inflammatory bowel disease. 01:56 What are the two major inflammatory bowel diseases that you know of? Crohn and ulcerative colitis. I'll mention it here. Really won't have much of a discussion. 02:06 But please know that these four will then make up your seronegative spondyloarthropathies. 02:12 Before we walk into the details, let's first take a look at common extra-articular manifestations that are important that you wanna be able to identify. 02:21 Around the joint periarticular, the insertion sites of the tendon may then undergo inflammation. 02:29 This is called enthesitis. If the tendon itself undergoes inflammation, tendinitis. 02:37 And if the fingers are then undergoing pain, called dactylitis. 02:42 Remember, dactylitis could also be seen -- what if there was a patient -- there was a young African-American boy who says "Doc --" or the mother tells you that her son, after going out playing has pain in the hand. 02:55 That's sickle-cell disease, right? With something called micro occlusive crisis with dactylitis. 03:01 That's the last time you've seen that, keep that in mind. 03:04 Ocular: they might be uveitis or conjunctivitis. 03:09 The uveia is the middle layer of the eye consisting of the iris, the ciliary body and the choroid. 03:16 You might find inflammation in this area called uveitis seen in many systemic inflammatory conditions. 03:23 And the GI: painless oral ulcerations or maybe colitis. Genitourinary: urethritis. 03:32 Now, one second here. With urethritis, nongonococcal. 03:37 This will not be referring to gonococcal type infection. 03:41 Remember, the common features include the following, again, seronegative, rheumatoid factor is negative, HLA-B27. Correct? And you're looking for bone issues. 03:51 Vaginitis or maybe perhaps balanitis, involvement of the penis. 03:55 Cardiac: aortitis, valvular insufficiency, heart block. 04:00 Cutaneous: something called blennorrhagicum. 04:05 And blennorrhagicum would mean a typical or a presentation that you would find, and I'll show you a picture of a rash that you would find on the sole of the foot of your patient. 04:15 Ulcerative colitis and Crohn's disease could be part of -- or a constellation of the four that I talked to you about. 04:23 With seron -- with ankylosing spondylitis, we may begin with telling you who your patient is. 04:30 Most likely going to be a young male. 04:33 And normally you and I, when we bend over to reach something, we'll have this vertebral curvature. Correct? But what then happens in this patient is that ankylosing. 04:45 Ankylosing in medicine obviously means fusion. 04:48 So there'll be fusion taking place of the vertebrae in this young patient. 04:53 So therefore when this young male is bending over, there'll be a lack of the vertebral curvature. Look for that. 05:01 So this is seronegative spondyloarthropathy characterized by inflammation of the axial skeleton. 05:08 With HLA-B27, 90-95% of your patients will be Caucasian. 05:15 Only about 50% could be African-American. It is male predominant. 05:21 However, we're beginning to see that may be more women could also be affected, keep that in mind. 05:28 Onset: early. Like if a young male, when trying to bending over doesn't have a proper vertebral curvature. 05:36 Signs and symptoms. Patient presents with progressive low back pain. 05:45 Remember, one of the common features of all seronegative spondyloarthropathies is the back pain. 05:52 But here, you're looking at a young patient most likely male. 05:56 But as I told you, could be a lady as well. 05:58 Patients may have morning stiffness but this time you find that there is improvement with exercise. 06:05 In general, whenever you deal with other than osteoarthritis -- remember osteoarthritis, that patient -- the morning stiffness might have lasted approximately 30 minutes. 06:16 And osteoarthritis, the mechanical wear and tear of the joints. 06:21 Keep in mind though with osteoarthritis, when the patient over a period of time, it's the wear, right, that caused the tear. 06:29 So therefore any type of activity would worsen the pain in osteoarthritis. 06:34 Here, the patient feels better. So, this is then similar to not osteoarthritis, but then it would be similar to rheumatoid arthritis. 06:44 The rheumatoid arthritis remember, many of your patients will be rheumatoid factor positive. 06:49 By definition when we say seronegative, these conditions, the patient is rheumatoid factor negative. 06:57 And the patient with rheumatoid might be positive, keep that in mind. 07:01 And then discussion of rheumatoid arthritis is completely different from what we're seeing here. 07:05 What you notice here is that as the patient gets older, for example from year 1947 to 1973, you'll notice that the patient is becoming more and more and more debilitated. 07:18 Patients eventually develop limitation of the flexion of the spine. 07:23 Physical exam finding, you're gonna -- well, this condition of the lower back, you're gonna refer to it as being lumbar lordosis. 07:32 Limited spinal motion demonstrated by a test that we call Schober's test. 07:38 Now, because of the lack of vertebral curvature, guess who's having a hard time properly functioning physiologically? The lungs. So with lumbar lordosis, as you see here, as the patient's getting older that the lungs will be compromised resulting in a type of restrictive lung disease. 07:59 But for issues as such. Now it's also important as we then go on to management. 08:05 Let's shortly talk about the Schober's test. 08:09 It's a physical exam maneuver useful for evaluating for ankylosing spondylitis. 08:14 It is performed by palpating for the L5 vertebra and marking 5 cm below and 10 cm above this point. 08:23 The patient is then asked to touch their toes. 08:26 If the distance between the two points does not increase by more than 5 cm, the patient has a reduced ability of lumbar flexion. 08:34 Diagnosis. X-ray. I'm gonna show you that ankylosing -- what does ankylosing mean? It means fusion. What is the fusion that you're focusing upon? It most likely is going to be in the vertebrae or in the sacroiliac joints. 08:52 These are the two places that you're going to expect to find fusion on x-ray. 08:57 In the vertebrae when there's fusion taking place, please picture what a bamboo stick looks like or a plantation of bamboo. 09:05 It's going to be a fused stick. 09:10 So therefore, the vertebrae is oftentimes referred to as being bamboo spine. 09:16 And seronegative obviously referring to RF negative. 09:21 Management. Anti-inflammatories. NSAIDs is where you begin, conservatively. 09:29 And then maybe use the same drugs that you would be using for rheumatoid arthritis. 09:33 So, these will be the drugs for modifying anti-rheumatoid type of drugs. 09:39 So these are disease modifying, D-M, anti-rheumatologic drugs, DMARDs. 09:46 Anti-TNF therapy. Physical therapy. 09:52 And remember, a patient with ankylosing spondylitis in the long run is gonna develop what kind of lung disease? Restrictive. Now if the patient at the same time at -- that's a lot of stress. 10:02 And there's every possibility that your patient might be a smoker. 10:06 So therefore, this is what I was telling you earlier. 10:09 You're gonna use that information, but restrictive lung disease. 10:14 And if the patient was a smoker, you wanna make sure that you maintain proper lung function, hence Smoking Association programs. 10:22 Steroid's really not part of the therapy here cuz this is not a true inflammatory type of issue. 10:28 You need to have modulators. 10:31 The picture on the left that you're seeing here is of the sacroiliac joint. 10:37 And you're noticing that there's fusion taking place. 10:40 This -- there's your black arrow, if you see. 10:43 The pictures on the right represent the spine being in the shape of a bamboo. 10:50 In other words, there's ankylosing taking place. In other words, fusion. 10:53 So therefore this young male who is trying to bend over doesn't have a proper, proper vertebral curvature.
About the Lecture
The lecture Seronegative Spondyloarthropathies & Ankylosing Spondylitis (AS) by Carlo Raj, MD is from the course Seronegative Spondylarthropathies. It contains the following chapters:
- Introduction to Seronegative Spondylarthropathies
- Ankylosing Spondylitis
Included Quiz Questions
What does the "seronegative" refer to in seronegative spondyloarthropathy?
- Rheumatoid factor negative
- HLA-B27 negative
- Anti-nuclear antibody negative
- Joint fluid culture negative
- Negative family history of arthritis
Which of the following findings are sometimes seen with seronegative spondyloarthritis?
- Uveitis
- Positive serum rheumatoid factor
- Bladder wall inflammation
- Heberden's nodes in the DIP joints of the hands
- Vasculitis
Which of the following is associated with ankylosing spondylitis?
- HLA-B27
- Rheumatoid factor
- Antinuclear antibodies
- Anti-Ro antibody
- Anticardiolipin antibody
What is enthesitis?
- Inflammation of the insertion site of tendons into bones
- Inflammation of the entire length of a tendon
- Inflammation of the ligaments
- Inflammation of joint capsule
- Inflammation of joint cartilage
What is the most likely diagnosis in a young patient with chronic back pain and the finding of "bamboo spine" on X-ray?
- Ankylosing spondylitis
- Ulcerative colitis
- Reactive arthritis
- Psoriatic arthritis
- Enteropathic arthritis
Which skin lesion is characteristic of reactive arthritis?
- Keratoderma blennorhagicum
- Dermatosis papulosa nigra
- Reactional keratosis
- Necrobiotic xanthogranuloma
- Hyperkeratosis lenticularis perstans
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |