Playlist
Show Playlist
Hide Playlist
Spinal Muscular Atrophy (SMA) in Children
-
Slides Muscle Disorders in Children.pdf
-
Download Lecture Overview
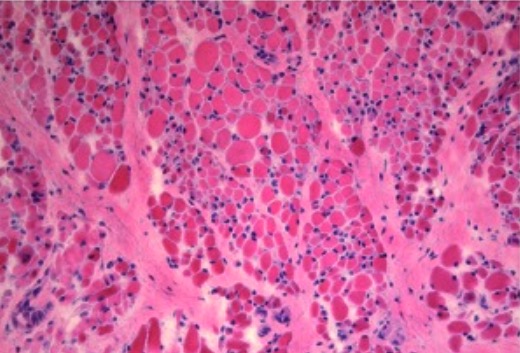
00:02 When children are weak, sometimes the problem is in the motor nerve. 00:06 In this lecture, we'll talk about specific motor nerve disorders that could occur in pediatrics. 00:13 Let's start with Spinal Muscular Atrophy or SMA. 00:18 SMA is often a very debilitating condition. 00:22 it's autosomal recessive in that it may travel in families. 00:26 and have unaffective carriers. 00:29 The defect is on the survival motor neuron gene or the SMN gene It results in a degeneration of the anterior horn cells of the spinal cord. 00:40 resulting in weakness. 00:43 There are three main types of SMA. 00:46 I, II and III. 00:47 SMA I is very severe. 00:50 It usually affects infants and is often life threatening. 00:54 SMA II is more moderate and SMA III is quite mild. 01:01 All of the SMAs, the problem is that small muscles are not innervated. 01:06 The larger ones still have innervations. 01:09 So, in muscle biopsy it will show a patchy appearance. 01:13 Much like this. 01:14 Patients will present with a progressive symmetrical proximal weakness. 01:20 Remember this is a lower motor neuron disease. 01:23 So, they will be floppy and may have absent deep tendon reflexes. 01:29 You may see muscle fasciculation as well. 01:31 And it is often seen easily in the tongue. 01:35 But remember, it is just the motor neurons. 01:37 These patients will have normal cognition. 01:41 Let's review the natural progression of disease without any effective therapy, which has only recently been discovered and instituted in the last 15 years. 01:49 Type one results in severe hypotonia in children. 01:53 Death before the age of 2 is common without therapy. 01:55 These patients will die of respiratory complications if untreated. 01:59 In Type II disease, they may have the ability to sit but often will not have the ability not walk. 02:06 This typically presents a little later around 6-18 months of age. 02:10 And it requires nutrition and respiratory support. 02:15 In Type III disease, patients may lose the ability to ambulate around 10 years of age. 02:22 It often presents after a year an a half of age and typically we will involve Physical therapy and orthopedics for braces or things like that so to they can function as long and as well as possible. 02:36 So, the diagnosis of SMA is made by a genetic test of the SMA I gene. 02:43 We'll send it for sequencing and look for deletions. 02:48 New treatments have come out for SMA including two new treatment options — a gene replacement therapy called Zolgensma and a drug called nusinersen. 02:59 SMA gene therapy is a one-time infusion that replaces the defective or missing SMN1 gene with a working copy. 03:07 This new gene increases survival motor neuron (SMN) protein levels, which improves motor neuron function and increases the likelihood of survival. 03:15 Recently, the FDA approved this treatment for children less than 2 years of age with SMA. 03:21 A child must have the SMN1 mutation that causes this disease to receive this therapy. 03:26 The FDA approved the use of this drug for all types of SMA with an SMN1 mutation, from infant-onset SMA type 1 to adult-onset SMA type 4. 03:37 Nusinersen uses synthetic (man-made) genetic material called antisense oliigonucliotide to improve the splicing of the SMN2 gene. 03:47 This helps children to make more SMN protein needed for healthy motor neurons.
About the Lecture
The lecture Spinal Muscular Atrophy (SMA) in Children by Brian Alverson, MD is from the course Pediatric Neurology.
Included Quiz Questions
Which of the following is TRUE about type 1 spinal muscular atrophy (SMA)?
- It is an autosomal recessive disorder.
- It produced an upper motor neuron disease.
- It is the mildest type.
- Children with this disease usually live until their teen years.
- It presents after 6 months of age.
Which type of spinal muscular atrophy (SMA) often affects infants and is life-threatening?
- SMA I
- SMA II
- SMA III
- SMA IV
- SMA V
Which of the following is a feature of spinal muscular atrophy (SMA)?
- Progressive, symmetrical muscle atrophy.
- Hyperreflexia
- Dermatitis
- Anaphylaxis
- Tongue hypertrophy
A 20-month-old boy presents with difficulty walking for the past month after previously meeting all developmental milestones. He is diagnosed with spinal muscular atrophy. Which of the following is the most appropriate treatment option?
- Physiotherapy and orthopedic care
- Nutritional supplements with respiratory support
- Only respiratory support
- High dose steroids
- IV plasmapheresis
Which of the following statements is TRUE about the pathophysiology of spinal muscular atrophy (SMA)?
- Degeneration of the anterior horn cells of the spinal cord
- Upper motor neuron disease
- Large muscles are not innervated, while small muscles are innervated.
- Dystrophin protein is not present in muscle fibers
- It is an autosomal dominant inherited disease.
A 10-year-old child has had difficulty walking for the last 2 months. The mother mentions a normal developmental history. She also indicates a similar disease in one of her parents. On examination, he can sit, shows no signs of abnormal cognition, but has difficulty ambulating, and shows tongue fasciculation, which the mother also mentions have been present since the child was 2 years old. Which is the most likely diagnosis?
- Type III SMA
- Guillian-Barré syndrome
- Polio
- Type I SMA
- Type II SMA
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture as usual: clear, concise, easy to remember. Thanks!