Playlist
Show Playlist
Hide Playlist
SIADH (Syndrome of Inappropriate Antidiuretic Hormone Secretion) in Children
-
Slides DIandSIADH Pediatrics.pdf
-
Download Lecture Overview
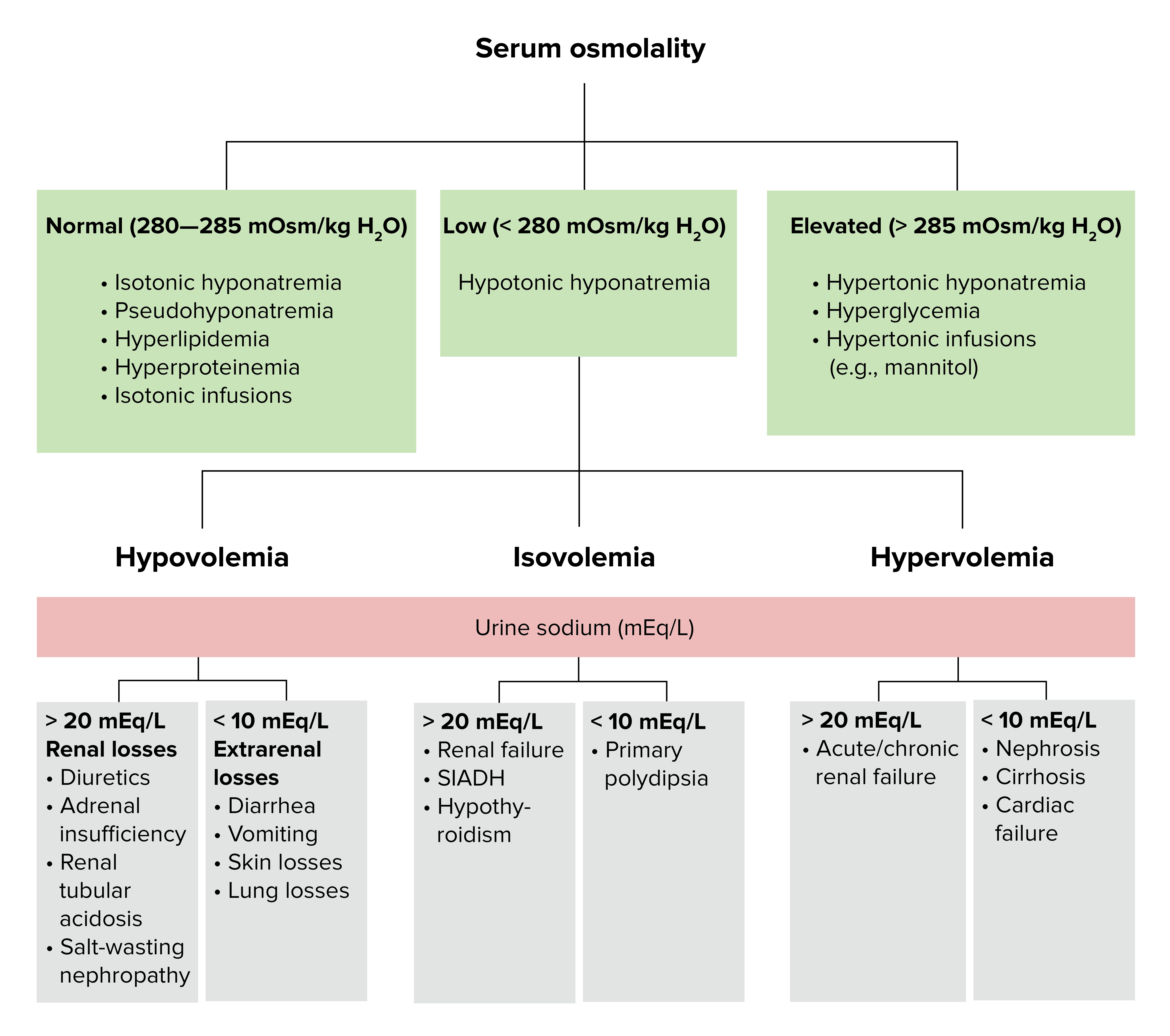
00:01 Let's switch gears and talk about SIADH. 00:05 Instead of too little ADH, there is too much ADH. 00:09 This excessive ADH in the blood cause an excessive insertion of this aquaporin channels which results an increased water retention. 00:19 Thus, the urine is excessively concentrated. 00:23 This results in a low sodium, as the water is more prevalent in the serum. 00:31 ADH can be secreted by not just your pituitary, it secreted by a host of other cells as well and usually in certain pathologic settings. 00:42 For example, the brain will secrete ADH when there is irritation of the meninges so, we may see ADH in meningitis. 00:51 In the lung, the type II pneumocyte produces ADH. 00:56 We commonly see patients with a bad pneumonia having low sodiums as a result of too much SIADH. 01:04 The GI tract also can create SIADH typically in patients with gastroenteritis this is probably an evolutionary way of protecting ourselves from becoming dehydrated in the sense of a sick child. 01:20 Additionally, some drugs can cause an excessive secretion of ADH. 01:27 Let's go through one of these things that cause it. 01:30 In the CNS, tumors, meningitis, encephalitis, hemorrhage, vasculitis and surgical trauma. 01:39 All of these things can result in a transient or more permanent SIADH. 01:44 In lung tissue, certainly pneumonias but also even bronchiolitis can cause SIADH. 01:50 Patients with cystic fibrosis may develop SIADH and certainly certain long malignancies although exceptionally rare in children can cause SIADH. 02:01 Gastroenteritis can cause a mild SIADH which can cause problems if unrecognize or if rarely severe. 02:10 Also, certain medications can cause SIADH and we typically think of some of the psychiatric medications. 02:18 The tricyclic antidepressants, the serotonin specific re-uptake inhibitors or SSRIs. 02:25 But also, PPIs or Protein Pump Inhibitors as well as ACE inhibitors can cause SIADH. 02:32 So, we may sometimes simply find a patient where we check a Chem-7 and say, hey look at that they have a low sodium and this how we make the diagnosis. 02:45 This is usually on patients with fairly mild disease. 02:50 And by mild, typically these patients are asymptomatic, if their sodium is low but still above 125. 02:57 A patient with a sodium of 130 isn't really gonna notice. 03:01 They're gonna be accommodating that okay. 03:03 However, in these severe cases where the sodium gets low and below 125 these patients can develop lethargy, confusion, you may see papilledema on the exam as their brain is swelling or they may develop seizure. 03:18 Some of these symptoms depend on the speed at which that sodium has been falling. 03:24 We'll talk about brain accommodation at the end but if that sodium has been falling very gradually over time the brain can accommodate that and they can have fewer symptoms. 03:34 If the sodium fell very rapidly patients can get in trouble in terms of CNS disease very quickly. 03:42 The diagnosis of SIADH can be somewhat complicated. 03:46 Typically, we will see as low sodium, a sodium in the blood should be really less than 135. 03:52 The serum osmolarity should be also low and the urine osms should be high. 03:59 The urine sodium is going to be high. 04:02 Remember the reason the patient is having a high water in the blood is because of an insertion of those aquaporins. 04:12 So, the sodium is still coming out. 04:15 The urine sodium will be high and the fractional excretion of sodium which is determined by this equation here is more than 0.5%. 04:24 So, let's think about how we fix sodium. 04:31 When we're fixing sodium be at high or low we need to it slowly and that's because sodium shifts that are rapid can cause problems in the brain. 04:42 Let's look at this closely because I think people tend to get confused about which problem causes which problem in the brain. 04:50 Imagine here we have a brain cell and a blood vessel. 04:54 These two compartments need to have the same osms in them. 04:59 They need to have the same osms so that there aren't fluid shifts one way or the other. 05:04 If fluid shifts into the brain, one would get cerebral edema. 05:08 If fluid shifts out of the brain what we typically see is central pontine myelinolysis which is really bad. 05:17 It's a disturbance of the pons which can cause problems with the basic functions of the body. 05:22 So, now let's imagine we have a certain number of sodiums in the blood. 05:27 This would be let's say a normal number of sodiums. 05:30 Likewise, the brain will create small proteins that exist a longer surface of the brain cell and we'll call those idiogenic osmoles. 05:39 So these small tiny proteins are providing an osmotic force that bounces out the sodium and allows a prevention of fluid shifts one way the other. 05:49 Now, if a patient were to get hypernatremic, let's say they had diabetes insipidus and they were gradually becoming more and more hypernatremic. 06:00 The brain could adjust by creating more osms, this osm would balance things out and would allow that patient to continually function even the presence of a high sodium. 06:12 We would see this for example in a profoundly dehydrated state. 06:15 However, if we would have go in and try and fix this problem quickly. 06:21 Let's say the patient had a sodium 180 that have been there for a long time. 06:25 And we went in and gave them very hypertonic fluid and rapidly removed the sodium from the blood space. 06:32 What would happen now is fluid would flow out of the blood space and into the brain and that would cause cerebral edema. 06:41 So, an overly rapid correction of a long-standing hypernatremia leads to cerebral edema. 06:50 Let's go back to this brain again now, here we have a patient with a normal sodium and a normal number of idiogenic osmoles. 06:58 Let's say this patient now develops hyponatremia the brain will accommodate accordingly and downregulate the idiogenic osmoles. 07:08 So that we have an equal amount of osmotic particles in both compartments and no fluid shift. 07:15 If we see this patient with a sodium of 120, let's say they have SIADH and we were to rapidly correct the problem by bringing up their sodium too quickly. 07:27 We would have suddenly fluid shifting out of the brain into the blood and there is one we would be at risk for central pontine myelinolysis. 07:37 I hope that clarifies that whole thing for you nicely and easily. 07:42 So if we have a patient with SIADH, we want to bring up their sodium slowly. 07:49 We may initially give 3% saline injection but only in cases with a patient has symptomatic hyponatremia for example seizure. 07:59 If this child is actively seizing we're going to give 3% saline boluses until the child is stabilized. 08:07 This would prevent further brain edema. 08:10 However, now we have to play our things fairy slowly and we're gonna gradually give fluids such that there is a slow sodium rise of about 0.5 milliequivalents per hour or no more than 12 milliequivalents per day. 08:27 That means if the patient has a sodium of 120. 08:30 We should be taking several days bringing that sodium back up. 08:34 We may need to free water restrict the patient to about 1 liter per meter square per day to achieve an appropriate water stasis for this patient. 08:45 In patients where restrictions of fluid is not possible we can use Demeclocycline. 08:51 Demeclocycline inhibits renal activity of ADH, so it may inhibit the activity of the excessive ADH in the blood. 09:01 Ultimately, the goal for SIADH is to treat the underlying disease. 09:07 The reality is that for cases like pneumonia or meningitis treatment of the condition, usually results in a resolution of problems. 09:17 I hope this lecture is clarified for you the differences between diabetes insipidus and ADH. 09:23 Thanks for your attention.
About the Lecture
The lecture SIADH (Syndrome of Inappropriate Antidiuretic Hormone Secretion) in Children by Brian Alverson, MD is from the course Pediatric Endocrinology. It contains the following chapters:
- Pathology
- Clinical Presentation
- Diagnosis
- Management
Included Quiz Questions
A patient has been gradually getting sicker over the past several weeks. Serum sodium level is found to be 185 mEq/L. The doctor rapidly corrects it to 140 (normal). What is a potential complication this patient may suffer?
- Cerebral Edema
- Central Pontine Myelinolysis
- Diabetes insipidus
- Diarrhea
- Urinary retention
Which of the following is not commonly associated with SIADH?
- Migraine
- Pneumonia
- Meningitis
- CNS tumor
- Tricyclic antidepressants
Which of the following plays a major role in patients developing symptoms of hyponatremia namely, lethargy, confusion, and seizures?
- Rate at which the sodium level decreased
- Duration of Hyponatremia
- Level of serum sodium below 130 mEq/dl
- Associated Pneumonia
- These symptoms only develop in Drug-associated SIADH
Which of the following lab findings is most consistent with SIADH?
- Serum Osm < 280 mOsm/kg and Urine Osm > 100 mOsm/kg
- Serum Osm > 280 mOsm/kg and Urine Osm > 100 mOsm/kg
- Serum Osm < 280 mOsm/kg and Urine Osm < 100 mOsm/kg
- Serum Osm < 300 mOsm/kg and Urine Osm > 300 mOsm/kg
- Fractional Excretion of Sodium < 0.5%
What is the mechanism of development of Cerebral edema when serum sodium is rapidly corrected in a patient with chronic hypernatremia due to Diabetes insipidus?
- Shift of fluid from interstitial space to brain cells
- Shift of fluid from brain cells to interstitial space
- Shift of fluid from vascular space to interstitial space
- Shift of fluid from vascular space to CSF
- Shift of fluid from CSF to vascular space
What will happen if we correct the sodium rapidly in a patient with chronic hyponatremia due to SIADH?
- Central Pontine Myelinolysis
- Cerebral Edema
- Brain Herniation
- Papilloedema
- Vertebral Disc Herniation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This is one of the best lectures of the pediatrics course. As usual complex topics made simple and memorable. Having put the dedication to explain the 2 central mechanisms for these phenomena (brain + kidney) helps tremendously! Thank you very much!