Playlist
Show Playlist
Hide Playlist
SIADH: Diagnosis and Treatment
-
Slides ActionOfADH EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
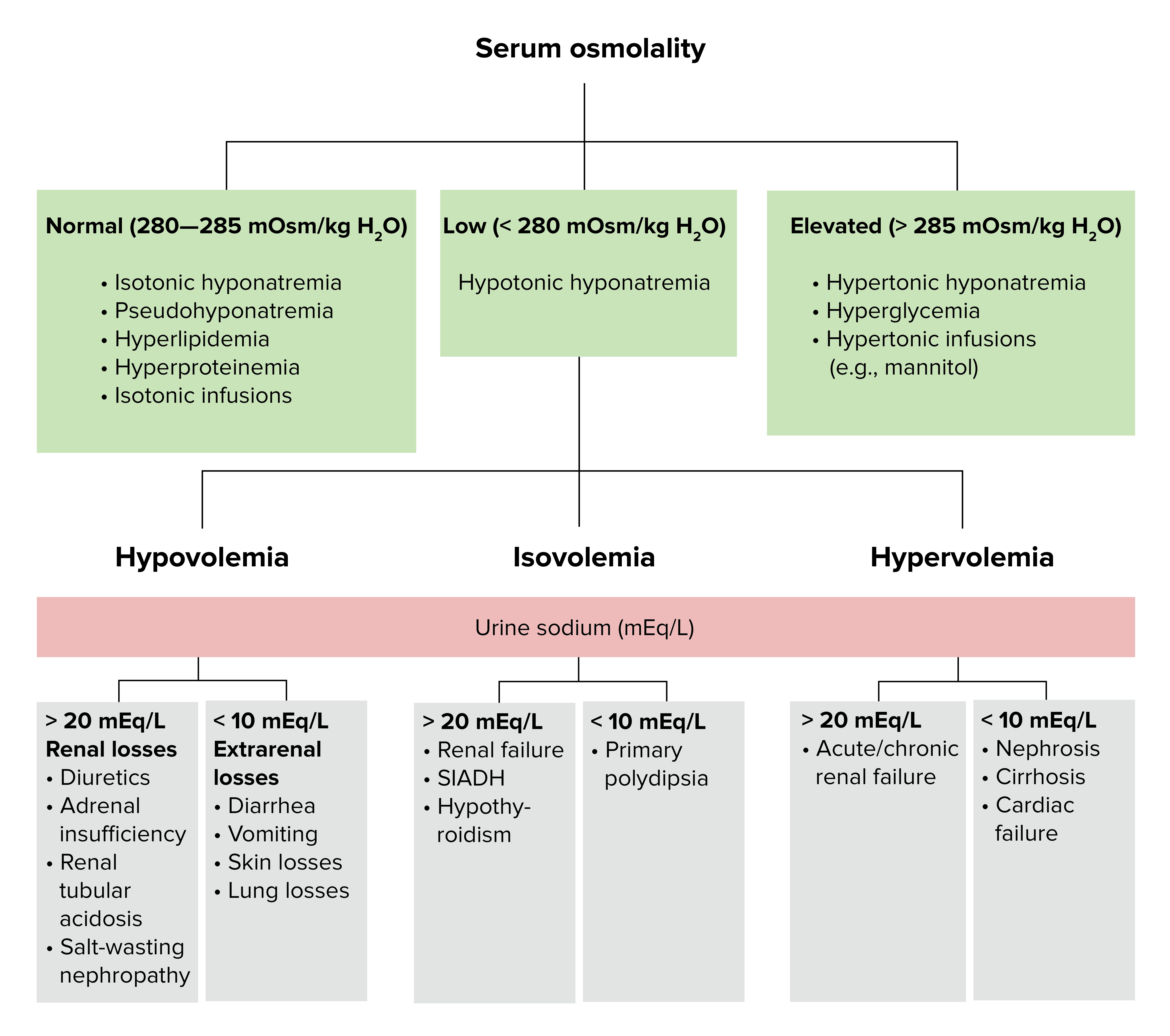
00:01 Let’s talk further about SIADH. 00:03 History and physical for sure; findings, here you go. 00:07 Euvolemic patient, what does that mean? What’s eu- mean, the prefix? It means normal. 00:13 You’ve heard of euthyroid, here we have euvolemia. 00:17 Serum sodium levels and plasma osmolarity, ridiculously low. 00:22 What about urine osmolarity? High. 00:28 Plasma osmolarity? Low. 00:31 Urine sodium? High. 00:35 Low BUN, serum uric acid, everything is being diluted, diluted, diluted. 00:43 Now, at the very bottom of this, it’s important, SIADH cannot be diagnosed without excluding hypothyroidism and adrenal insufficiency. 00:54 Once again, keep in mind that whenever you are dealing with ADH, other endocrine dysfunctions, especially thyroid and the adrenals, are important for you to make sure that you rule out. 01:08 What do you want to do? Always come to the underlying cause. 01:14 If your issue was a lung cancer, completely different steps of management. 01:19 If your patient was on drugs, which is carbamezapine, obviously remove the offending agent. 01:26 Whatever it may be, you want to keep things in mind, pulmonary disease and treatment, cessation of drugs, hormonal replacement and adrenal insufficiency or even perhaps hypothyroidism. 01:36 Things... 01:37 These are things that you are paying attention to when dealing with SIADH. 01:41 Restrict free water intake. 01:43 Here, once again, caution must be exercised with patients with SIADH secondary to subarachnoid haemorrhage due to exacerbation of the vasospasms and infarction from the drop in blood pressure. 01:57 Keep that in mind. 01:58 So, if your patient, extremely important clinical point, is the fact that if there is going to be head trauma and it’s due to subarachnoid haemorrhage, be very, very careful because if there is going to be ADH and vasospasm, it only makes matters worst up in the brain. 02:18 That’s a huge clinical point that you can use for every single board that is ever presented to you. 02:26 Restrict your free water intake please with SIADH. 02:29 If a patient becomes symptomatically hyponatremic, hypertonic saline can be given to correct sodium levels. 02:36 However, the only thing that you want to worry is the fact with any time you’re giving IV saline, whatever the indication may be, dehydration, maybe SIADH, so and so forth, is that you never give it rapidly because if doing so then you’re always worried about an interesting side effect, but nonetheless, incredibly significant called central pontine myelinolysis. 02:58 SIADH pharmacologically… high salt in conjunction with loop diuretic. 03:04 Remember, you are trying to get rid of this. 03:06 Now, is all the loop diuretic going to be effective? Well, it all depends, but sodium is going to be incredibly important. 03:14 Vasopressin receptor antagonists is what you’re thinking about here. 03:18 Why? Because there’s too much SIADH, we’ll talk about these in a second, and you have a particular V2 receptor blocker known as conivaptan and this is then given as IV only, V2 receptor blocker. 03:34 Pharmacologically speaking, with vaptan as being a V2 receptor blocker, we have an oral analog known as tolvaptan and interesting enough, you have demeclocycline and lithium. 03:50 Stop here for one second. 03:52 The boards will ask you the following. 03:53 Here’s a-Here’s a patient that requires demeclocycline, here is a patient that is bipolar taking lithium. 03:59 This, ladies and gentlemen, will bring about nephrogenic diabetes insipidus that we do know. 04:06 Now, your patient has SIADH and the patient with SIADH where there’s too much V2 receptor activity, wouldn’t you want to then induce nephrogenic diabetes insipidus? And that’s the thinking that you must have here when dealing with demeclocycline and lithium. 04:26 Antagonize ADH in action and can be used in a rare patient who cannot be treated with vaptan the drugs mentioned above. 04:37 Steps of management… restrict free water intake. 04:42 Get rid of that fluid if you’re thinking about loop diuretic, but once again keep in mind of the sodium levels. 04:48 V2 receptor blockers and these are your vaptan drugs: conivaptan, IV, tolvaptan, your PO oral. 04:58 If these are refractory, then you start thinking about drugs such as demeclocycline and lithium.
About the Lecture
The lecture SIADH: Diagnosis and Treatment by Carlo Raj, MD is from the course Pituitary Gland Disorders.
Included Quiz Questions
A patient with a classic syndrome of inappropriate antidiuretic hormone secretion (SIADH) presents with which set of findings?
- Euvolemia, low plasma osmolarity, low serum sodium
- Euvolemia, high plasma osmolarity, low serum sodium
- Hypovolemia, low plasma osmolarity, low serum sodium
- Hypovolemia, low plasma osmolarity, high serum sodium
- Hypervolemia, low plasma osmolarity, low serum sodium
Patients with SIADH have hypoosmolar hyponatremia and a euvolemic state. Which condition is most likely to have a similar presentation?
- Hypothyroidism
- Diabetes mellitus
- Adrenal hyperplasia
- Sheehan's syndrome
- Hyperparathyroidism
Which statement is not true regarding proper fluid treatment in patients with SIADH?
- The electrolyte concentration of administered fluid is less than that of the plasma.
- Free water intake is restricted.
- Intravenous saline, if indicated, is administered gradually to avoid central pontine myelinolysis.
- Conivaptan is administered intravenously.
- Hypertonic saline is rarely indicated.
Which statement about lithium and SIADH is correct?
- It diminishes the responsiveness to antidiuretic hormone.
- It increases the secretion of antidiuretic hormone.
- It increases the responsiveness to ADH.
- It diminishes the secretion of antidiuretic hormone.
- It increases the reabsorption of sodium from the distal convoluted tubules.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |