Playlist
Show Playlist
Hide Playlist
Seborrheic Dermatitis, Allergic and Irritant Contact Dermatitis
-
Slides Atopic Contact and Seborrheic Dermatitis.pdf
-
Reference List Dermatology.pdf
-
Download Lecture Overview
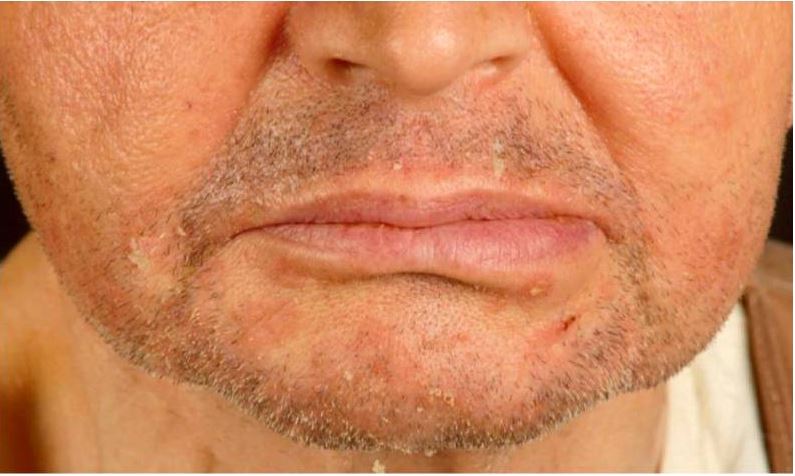
00:01 So, first up, seborrheic dermatitis. Now, this is also known as cradle cap in infants, but it's important to know that it can also cause disease in adults. I'm hoping that that's not a picture of our female 18-year-old English major. 00:16 But either way, we do know that seborrheic dermatitis is a chronic, relapsing, mild dermatitis. Doesn't really have any systemic manifestations or cause particular trouble down the road. The etiology is actually unknown, though strangely, it is associated with malassezia, which is a type of fungus, and it does respond, oftentimes, to an topical azole, you know, like ketoconazole, that kind of thing. 00:40 So, still unusual exactly what the pathogenesis is. As I said, infants, adults, the only time where it can really cause significant problems is in an HIV positive patient. Has a predilection for a number of different sites. Can cause problems on the scalp, behind the ears, the eyebrows, the nasolabial folds, the upper chest, the back, the ears, lots of issues with the eyelids, so called blepharitis, and rarely even can manifest in the axilla. And importantly, the extremities are spared. You're not going to see this kind of itchy lesions, eczematous lesions in the antecubital fossa or down the volar surface of the wrist, as we might be seeing in our patient. 01:23 Is it pruritic? Yes, but pretty mild, not intensely pruritic. 01:28 Shown here again, in our picture is this scaly, flaky, so-called greasy-looking plaques. That's the term that should jump off the page at you when you're reading it in a board question. 01:40 Treatment, as I said, selenium sulfide which has some antifungal properties, and of course, an azole shampoo like ketoconazole, fluconazole, that kind of thing. 01:50 Next up, let's talk about allergic and irritant contact dermatitis. 01:54 First off, allergic contact dermatitis. This is a localized immune-response to a topical antigen, the most common of which is something like poison ivy. The urushiol, which is an oil resin in poison ivy and poison oak, that sort of thing. It's T cell-mediated. 02:11 It's a delayed-type hypersensitivity reaction. 02:14 Doesn't immediately cause skin findings. 02:17 It's more delayed over a couple of days. Acutely though, after a couple days, you'll see these erythematous plaques that will evolve into vesicles, and as we're seeing in this patient, may eventually lead to bullae. 02:30 Over time, if you're constantly exposed to this allergen, you may develop erythematous, indurated, that is, fullness of the skin and scaly plaques over time. 02:41 The most common allergens hands down, no pun intended, it's urushiol, which is the oil that we find in poison ivy, poison sumac, and poison oak. Interestingly, we know this is an allergy-mediated process as opposed to some sort of intrinsically toxic component in urushiol because about 50% of people actually have no response when exposed to urushiol. Other common allergens include nickel, cobalt, latex, some topical antimicrobials, and the preservatives in a number of different soaps, shampoos, and fragrances. And that's why it's such an important point to take a very thorough history, a detailed history of every possible environmental exposure when you're talking to patients who are presenting with this kind of picture. 03:28 Treatment, obviously, it's going to be to remove the avoidable or remove the offending agent. You can use anti-histamines to help with discomfort. Patients really are very itchy with this condition and they're asking for something to help them and some anti-histamines can be helpful. Occasionally, we'll use topical or even systemic steroids in severe cases, or if it involves the face or other sorts of areas. 03:53 Now let's talk about irritant contact dermatitis. 03:57 Rather than being immune-mediated, this is an acute or chronic, local inflammatory reaction to a cytotoxic stimulus, whether it's physical or chemical. 04:08 That substance is actually directly causing a disruption of the epidermal barrier with direct injury to keratinocytes or to the cell membranes. It is, for whatever reason, more common in women. There's this association that historically or traditionally, women were more social professions involving cleaning and using hand solvents, things like that. So there has been an increased risk of occupational exposures amongst women. 04:35 Common irritants, as I'm suggesting, detergents, some surfactants, alkali-based compounds, bleaching agents. 04:45 In a chemical plant, you may see this happen with fiberglass exposure, some dusts, plants, of course, some types of toxic alcohols. 04:54 And in kids, simply a diaper dermatitis, , the mixture of stool and urine and a moist environment can cause this irritant contact dermatitis as well. Treatment, very similar. 05:06 Just remove or avoid the offending agent. 05:10 And we can still use those other things like anti-histamines and occasionally, steroids to help. So, putting these 2 side by side, contact dermatitis, it's a T cell-mediated response to an allergen. 05:24 Considered a delayed type hypersensitivity reaction, and it can be acute or chronic. The irritant type is a localized inflammatory response to something that is physically or chemically toxic. 05:35 And it's a direct cytotoxic response that you're seeing. 05:39 This can also be either acute or chronic. It depends on how much of the agent you're being exposed to over how long a span of time. 05:48 So, going back and thinking about our patient, this is occurring on both extremities in the antecubital fassa. It's clearly symmetric So, is it possible that she has been applying some lotion to the area and the lotion itself is what's precipitating the immune response, therefore being an allergic contact dermatitis? It's something to consider and it would certainly be important to talk to our patient and inquire about what she's applied to the area for her symptoms. 06:16 Now let's talk about psoriasis. Psoriasis has variety of different subtypes, the most common of which is simply plaque psoriasis. And this picture shows both some plaque psoriasis subtypes, as well as in the bottom picture there, you can see so called Palmo pustular psoriasis with more of those vesicles and pustules. 06:36 But typically, we're looking for silvery scale. 06:39 That's the classic description you'll see on the boards, is this silvery plaque on an erythematous bed, and if you were to scrape off one of those plaques, you'd get this punctate bleeding that would occur right underneath the plaque And that's, again, it's one of those pathognomonic findings that you would see with psoriasis. 06:57 So, let's go back and revisit the case and see if any particular points about atopic dermatitis jump out at us. So, again, our 18-year-old English major had a history of "dermatitis." Who knows exactly what that means to this particular patient? But we do know that atopic dermatitis is more common in children, far more so than in adults. 07:21 The vast majority will have symptoms before the age of 5. 07:24 So if you have a patient coming in with a new dermatitis, and they're in their 20s, or 30s, atopic dermatitis would be much less likely to be the cause. 07:34 In fact, atopic dermatitis, most commonly, gradually remits with age, such that those children who had atopic dermatitis before the age of 5, only about 5% will still have symptoms by the time they're 20 years of age or older. 07:49 And that's similar to the, sort of, natural history for childhood asthma. 07:56 Next up, the types of features that will be relevant to make us thinking about atopic dermatitis. We see here that in the social history, our patient had a mother with asthma, a brother who's allergic to "everything." And then looking above that in the HPI, our patient has a history of allergic rhinitis, mild asthma, seasonal allergies. 08:15 These are all bells that should be ringing saying, "Family history and personal history of atopy." Importantly, the cause of atopic asthma is really still unknown. All we know is that it is some sort of immune-mediated process, but exactly what triggers it is not clear. It's possible that it's a problem with skin barrier dysfunction and that certain external antigens are penetrating the skin and triggering immune cells in the skin to become inflamed and to release certain cytokines into the skin. There may be simultaneously some immune dysregulation, or may just be some cutaneous hyper reactivity to normal environmental stimuli. 09:00 And lastly, on this page, when we think about the physical exam, these are the classic features that you should be looking for, and these things really make the clinical diagnosis. You shouldn't need a biopsy. 09:12 Dry, lichenified, erythematous plaques, with possibly some scattered papules, lots of excoriations from all that scratching. 09:20 And the most common places are going to be the antecubital fossa, perhaps the volar aspect of the wrist, the flexural creases behind the legs. 09:27 Those are the types of areas you should be thinking about. 09:30 If you were to do any blood testing and largely unnecessary, but IgE levels would likely be elevated. 09:37 And you could do specific skin prick testing to see if there's any particular allergens that trigger atopic eczema in this particular patient.
About the Lecture
The lecture Seborrheic Dermatitis, Allergic and Irritant Contact Dermatitis by Stephen Holt, MD, MS is from the course Allergic and Immune-mediated Skin Disorders.
Included Quiz Questions
Which of the following is true regarding seborrheic dermatitis?
- It presents with scaly, flaky, greasy-looking plaques.
- It presents with lesions that appear to be stuck on the skin surface.
- It presents with carbuncles over the groin.
- It is treated with systemic corticosteroids.
Which of the following is true regarding allergic contact dermatitis (ACD)?
- It acutely presents with erythematous plaques, vesicles, and bullae.
- Low-potency oral steroids may be used in severe cases or if it involves the face.
- It is caused by an IgE-mediated hypersensitivity reaction.
- The appearance of punctate bleeding spots when the scales are scraped off is pathognomonic of ACD.
Which of the following is associated with irritant contact dermatitis?
- Direct cytotoxic response
- Exposure to nickel and cobalt
- T cell-mediated response
- More common in men
Which of the following is associated with allergic contact dermatitis?
- Exposure to latex
- Immunosuppression
- Exposure to alcohols
- Elevated IgG levels
Which of the following pairings is correct?
- Irritant contact dermatitis – Diaper dermatitis
- Allergic contact dermatitis – Seasonal allergy
- Atopic dermatitis – Malassezia infection
- Seborrheic dermatitis – Exposure to urushiol
- Psoriasis – Scaly, greasy-looking scales
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |